1. Context
The word - pandemic is coined from two Greek words- ‘pan’ and ‘demos’ meaning ‘all’ and ‘people’ respectively. It is a disease that affects a substantial number of people at global proportions. The causative organism can either be a bacterium, a new virus, or a new strain of a virus that has not infected humans for a long time and is capable of infecting a larger population rapidly beyond international borders (1). It is worthy to note that an endemic widespread of a disease that affects several continents but with a stable number of infected people is not considered as a pandemic, so also is a disease that is neither infectious nor contagious but has resulted in the death of many such as cancer. Example of notable pandemics that have occurred include Black Death (also known as the plague), smallpox, Spanish flu, Asian flu (1957 - 1958 Influenza A H2N2 pandemic), Hong Kong flu amongst many others. COVID-19 and HIV/AIDS are the current pandemics (1).
According to the World Health Organization, there are six-stages to be undergone by a novel infection before it is termed a pandemic (2). After the criticisms by pharmaceutical companies who rushed to develop drugs and vaccines for the 2009 swine flu pandemic over the rush by the WHO to declare the outbreak as a pandemic but later turned out to be mild, the WHO has suspended the used of the six-stages of classification (3). As a result of that, there was a delay in declaring COVID-19 a pandemic (4).
This six-stage classification was applied to describe the process by which the influenza virus is considered a pandemic from the initial infection of few people (5). The WHO classification does not consider mortality rate and virulence of the causative organism, but rather defined the phases by the spread of the disease (6).
Phase 1: Infection circulates only among domesticated or wild animals, with no animal-human transmission. The estimated probability of pandemic is uncertain (7, 8).
Phase 2: The causative organism is now capable of infecting humans i.e. there is animal-human transmission of infection. This is a potential pandemic threat (7, 8).
Phase 3: Sporadic or small clusters of infections in humans that is insufficient to cause sustained community-level outbreak (7, 8).
Phase 4: Transmission of infection among humans that is sufficient enough to cause sustained community-level outbreaks (7, 8).
Phase 5: Same causative organism capable of causing sustained community-level outbreaks in at least two countries in one WHO region (7, 8).
Phase 6: Same causative organism capable of causing sustained community-level outbreaks in at least two countries in one WHO region and at least one other country in a WHO region (7, 8).
‘Suppression’, a more extreme long-term non-pharmacological measure is another strategy that was adopted during past and present pandemics to reduce the basic reproduction number of the causative organism to less than 1 in a bid to reverse the pandemic (9, 10). It includes, total lockdown of countries with exception to essential services such as healthcare (pharmacy and hospitals), security, fire services, and security, isolation of infected people, social distancing, and household quarantine (11, 12).
2. Objectives
We conducted a qualitative systematic review that focused on identifying past, present and future pandemics.
3. Data Sources
For this study, we used Grant and Booth’s 2009 definition of a qualitative systematic review: a method for combining or contrasting the results of qualitative studies or a strategy where the main research findings of primary studies are summarized but not statistically mixed (12). This approach allows for the accumulation of knowledge which may lead to the development of a new theory, a broader perspective or an interpretative translation.
3.1. Search Strategy
This review assesses available evidences including country reports, journal articles, World Health Organization reports, and other country-wide and regional reports on issues pertaining to pandemics and disease outbreaks. The review is qualitative-based. Search for relevant medical and scientific literature in biomedical databases such as MEDLINE, Google Scholar, PubMed and Web of Science was conducted with the following key terms: "Past pandemics", "Previous pandemics", "present Pandemics", and "Disease outbreaks".
3.2. Inclusion and Exclusion
This review addressed only papers focused on pandemics. For the published papers, inclusion criteria consisted of both descriptive and argumentative disease outbreak studies generally focused on pandemics and published in English. Given the comparatively limited scale of the supporting scientific evidence in this prospect, we also included books and book chapters, unpublished reports and conference proceedings, and published reports from governments and global health organizations but excluded superfluous items not related to pandemics and disease outbreaks. To evaluate whether articles satisfied these criteria, paper selection was conducted by analyzing abstracts and titles, in addition, utilizing supplemental sources obtained from the reference lists of the papers. No date and geographical restrictions were applied to the search results.
4. Results
4.1. COVID-19 (SARS-CoV-2 Infection)
COVID-19 is a highly contagious disease caused by the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), affecting more than 165 countries within 3 months including China, United States of America, India, United Kingdom, amongst many others. The virus is spread via small droplets produced by sneezing, coughing, and talking between people in close contact, touching the nose, mouth, or eyes after touching a contaminated surface. Infected asymptomatic patients can still transmit the virus too others (13). It first originated in a city- Wuhan, China, in late 2019 and has spread to several other countries, with the World Health Organization declaring it a pandemic on 11th March, 2020. This was followed by several other measures put in place by government of countries in a bid to curtailing the spread of the virus. These include: nationwide lockdowns, social distancing, mandatory use of facemasks, washing the hands with soap and clean running water and the use of hand sanitizers afterwards. These measures resulted in several disruptions to many areas of human life including healthcare, economy, recreational services, religious activities, and academic activities.
There is no approved guideline for the treatment of COVID-19, however, the World Health Organization made available guidelines to help provide symptomatic relieve (management of the symptoms) for instance, antipyretics for fever, immune boosters, oxygen therapy for respiratory distress, and caution to be taking when dealing with vulnerable groups such as children, pregnant women, and those with other co-morbidities. Several countries have adopted this with significant country-to-country variations (14, 15). Due to an increase in international flights rapid urbanization, the rate at which the virus spread is much wider than what was experienced in recent pandemics. SARS-CoV-2 has a higher rate of infectivity but lesser severity of symptoms than the conventional severe acute respiratory syndrome (SARS) (15). Preventive measures include the following: disinfecting surfaces with disinfectants such as 70% isopropyl alcohol, 0.5% hydrogen peroxide, or 0.1% sodium hypochlorite, contact tracing, practicing respiratory hygiene, frequent hand washing with running water and soap, or the use of alcohol-based sanitizers, avoiding touching the mouth, eyes, and nose, social distancing, closure of places of mass gathering, travel ban, Isolation from confirmed and suspected cases, and temperature screening.
4.2. Asian Flu (H2N2 Viral Infection)
Asian flu was caused by a strain of H2N2 virus and transmitted via contact with infected person or animal (16). The pandemic originated from Southern China, spread to Singapore, Japan, Hong Kong, and Taiwan afterwards, and to the rest of the world in the summer (between June and September) of 1957. There were two routes by which the disease spread: the first route was to Scandinavia and Eastern Europe from Russia and to other countries from United States of America. Within 6 months, the disease spread to other countries of the world, infecting many (17).
Peramivir, vitamin D, amantadine, lanimivir, oseltamivir, rimantadine, zanamivir, and umifenovir were drugs used in the treatment of the disease (18).
4.3. Hong Kong Flu (H3N2 Viral Infection)
The Hong Kong flu was a highly infectious disease with milder severity than the Asian flu caused by the H3N2 viral strain. Vietnam War veterans going back to the U.S spread the virus to others. 1n 1969, the virus spread to other countries, notably United Kingdom, Canada, Japan, Wales, and Australia (19). Social distancing, respiratory hygiene, hand washing hygiene, and use of facemask were some of the steps taken to contain the spread of the virus.
4.4. SmallPox (Variola Virus Infection)
For many decades, smallpox plagued humanity and is spread through respiratory droplets from infected cases as well as contact (20). Before the emergence of the historic vaccine developments made by Edward Jenner, smallpox was a serious global threat. As a natural disease, the origin of smallpox is lost in prehistory. It is estimated to have appeared during the time of the first pastoral settlements in north-east Africa around 10,000 BC (21-23) after which it spread to India by means of ancient Egyptian merchants. The Crusades, Arab expansion and exploration of the West Indies all led to the transmission of the disease (24). Smallpox had an impact on every level of the society. For instance, in Europe, 400,000 people died of smallpox annually in the 18th century, and a third of the survivors went blind (25). The case-fatality amongst infants was particularly alarming as figures approached 80% in London and 98% in London during the late 1800s (25-27).
4.5. Tuberculosis (Mycobacterium tuberculosis Infection)
Tuberculosis is the leading cause of deaths amongst infectious diseases with about 3 million deaths annually (28). In the history of mankind, tuberculosis has had its toll on a lot of victims and had posed a challenge to human existence. During transhumance out of Africa 1.7 million years ago (29), there were tendencies that the early migrants carried the tuberculosis disease alongside (28) as it was known to have been well established in East Africa in the 19th century. At the beginning of the 19th century, insights into the pathogenesis of tuberculosis began to unravel and transmissibility of the disease was demonstrated in 1865 (28). However, in 1882, this unprecedented disease became better understood following the discovery of Mycobacterium tuberculosis as its causative agent by Robert Koch (30). Reportedly, there were about 8.7 million cases and 1.4 million deaths attributed to tuberculosis alone (30, 31) with about 2 billion people latently infected (28). Prior to this, scientists suffered a lot of setbacks in understanding the aetiology of the tuberculosis in infected patients and this had a significant impact on the quest for treatment. For instance, fresh air, milk and sea voyages were recommended as treatment for tuberculosis while “Just sleep and eat nutritious foods” was given as advice to tuberculosis patients in the 1800s. While these approaches lacked prominence, deaths caused by tuberculosis in London, Hamburg and Stockholm had approached 100,000 at that time (29, 30) including some American cities (31, 32).
4.6. Black Death (Yersinia pestis Infection)
Black Death pandemic was also known as ‘The Plague’. This was one of the most disastrous disease outbreaks epidemics in human history (33). This was Europe's first human plague and it killed tens of millions of people; an estimated 30 - 50% of the population in Europe from 1347 - 1351 (33, 34). The Black Death killed indiscriminately as the risks of death varied amongst age groups (35). Physicians during this time could not provide an effective treatment for the disease outbreak neither could they understand its epidemiology. In order to curtail further spread of the disease, these physicians recommended consumption of simple diets, avoidance of excessive sleep and sex, and the collection regular enemas. However, none of these recommendations had a significant impact on the spread of the disease.
4.7. Spanish Flu (H2N2 Viral Infection)
This was one of the longest-lasting and repetitive pandemics that affected humans’ life and resulted in the death of many people - 20 - 100 million deaths globally. The first place where the outbreak emerged was not clear, but it was suggested that China was the possible origin of the virus. The first outbreaks however occurred in North America as well at the same time in March 1918 (36). Spanish flu was transmitted by respiratory droplets, direct and indirect contact. Preventive Measures taken were good hygiene, Physical distancing, quarantine, and Isolation. There were no vaccines and antivirals at that time.
4.8. 2009 Swine Flu (H1N1 Viral Infection)
H1N1 2009 pandemic emerged from Mexico, spread to 122 countries within six months due to global trade and travels, and resulted in the death of over 284, 000 people globally. There were three waves of the H1N1 pandemic- in spring, summer, and fall. There were generally mild waves in spring and early summer but a more severe wave re-emerged shortly after schools were reopened. Children and younger adults were more susceptible to 2009 H1N1 pandemic than older adults above the age of 50. The infection was transmitted by respiratory droplets, direct and indirect contact.
Vaccination, good hygiene, physical distancing, quarantine, and isolation of infected people were steps taken to control the spread of the virus. Vaccines H1N1 pandemic were available and antivirals used include Tamiflu, Relenza, Rapivab, Xofluza etc (37).
4.9. HIV/AIDS
The Human Immunodeficiency Virus is a retrovirus that affects the immune system of an infected person consequently making them susceptible to all manner of infections. AIDS; Acquired Immune Deficiency Syndrome results when the immune system is so weakened that opportunistic infections have gained ground and overpowered it. HIV is transmitted by unprotected sex, sharing of contaminated sharp objects, transfer from mother to child, and through bodily fluids. Safe sex, abstinence, screening blood products, and safety habits are ways of preventing the infection. A vaccine has not been discovered yet, however, there are drugs known as Antiretrovirals that help increase the body’s CD4 count while decreasing the viral load. HIV pandemic results in not less than 32 million deaths globally (Table 1) (38).
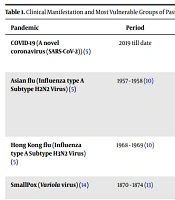
| Pandemic | Period | Clinical Manifestation | MVG | ERN |
|---|---|---|---|---|
| COVID-19 (A novel coronavirus (SARS-CoV-2)) (5) | 2019 till date | Cough, shortness of breath or difficulty breathing, fever, chills, muscle pain, sore throat, loss of taste or smell. | Elderly | 5.7 (5) |
| Asian flu (Influenza type A Subtype H2N2 Virus) (5) | 1957 - 1958 (10) | Fever, body aches, chills, weakness, loss of appetite, dry cough, sore throat, and difficulty in breathing. Complications include pneumonia, seizures, heart failure, and death. | Pregnant women, people with pre-existing heart and lungs disease, Elderly, Latin America, United Kingdom, China (10) | 1.8 (11) |
| Hong Kong flu (Influenza type A Subtype H3N2 Virus) (5) | 1968 - 1969 (10) | Fever, body aches, chills, weakness, loss of appetite, dry cough, sore throat, and difficulty in breathing. | Children, elderly | 1.06 - 2.06 (12) |
| SmallPox (Variola virus) (14) | 1870 - 1874 (13) | Appearance of the ‘speckled monster’ on the skin. | Infants | N/A |
| Black Death also known as the Plague (Yersinia pestis) | 1347 - 1351 (14) | High fever, painful localized swollen lymph nodes. | All age groups | N/A |
| Tuberculosis (Mycobacterium tuberculosis) | 19th - 20th century (15, 16) | Weight loss, and hemoptysis. | All ages | N/A |
| Spanish flu (Influenza type A Subtype H2N2 Virus) (39) | 1918 - 1919 (39) | Fever, nausea, aches, diarrhoea (40) | Ages 20 - 40 (40), Asia, Sub Sahara Africa, Latin America (39) | First wave; 1.49 - 2.8, Second wave; 3.75 (26) |
| 2009 Swine flu (H1N1 Influenza virus) (40) | 2009 - 2010 (40) | Fever, chills, cough, breathing difficulty, body aches (40) | Ages 5 - 19 (27), China, Australia, Italy, Greece, Chile, Korea | Range of 1.4 - 1.6 (28) |
| HIV/AIDS ( Human immune deficiency virus (29) | 1997 - till date | Fever, chills, cough, rashes, aches, weight loss | Young people between ages 20 - 24, Countries in Sub Sahara Africa, Asia and the Pacific, the Caribbean, Eastern Europe and Central Asia | N/A |
Abbreviations: MOT, mode of transmission; MVG, most vulnerable groups; ERN, estimated reproductive number; CO, causative organism.
4.10. Lessons Learnt from Past Pandemics and Future Recommendations
On critical examination of the nature, death rate, mode of transmission and clinical manifestations of past pandemics, a lot of useful insights can be drawn from how they were handled and most importantly, how the world can learn from these lessons so as to prepare better for future disease threats and pandemics. This study has shown that pandemics are recurring throughout history and have continued to shape and reshape human lives, behaviours and activities.
4.10.1. Early Planning and Proper Responsive Measures
One of the identified issues from past pandemics is the need for local, national and global bodies to collaborate through proper information sharing networks across countries. Adequate standard operating procedures must be put in place to ensure that pandemics are effectively contained (41). A review of past pandemics has brought to light the need for early detection and testing, scrutiny, and an improved virological surveillance and contact tracing to cushion the spread of the virus (41). The activation of the Strategic Health Operations Centre (SHOC) during the 2009 H1N1 influenza pandemic formed the mainstay for coordination between WHO and member countries and facilitated a lot of proper emergency response activities against influenza (41).
Furthermore, the WHO-coordinated Global influenza Surveillance and Response System Network proved to be very instrumental in cushioning the effect and severity of the 2009 Influenza pandemic (42). Another important lesson to note is that containment and quarantine measures did little to stop the spread of influenza virus. From our research, influenza shows uncanny similarities with the novel coronavirus in terms of clinical manifestations and as such it would seem that containment and quarantine measures are impractical in combating the novel coronavirus (43, 44).
4.10.2. Consideration for Vulnerable Groups
Due to the severity of pandemics, in the past and even now, a lot of funds and high priority is employed in cushioning the effect and flattening the pandemic curve. a a pandemic is no joke and the harshest of blows are dealt on countries with weak health system structures. However, while attempting to salvage the situation, populations that are at risk for contracting the disease either due to their age (the young and the elderly) or pre-existing medical conditions or pregnancy are often neglected or relegated to the background. Past pandemics have revealed that there is need for proper pandemic consideration for the vulnerable groups when making decisions to cater for the health needs of the people. The vulnerability of these populations, probably due to a weaker immune system than the rest of the population, makes them at risk for easily contracting the disease and furtherance of the spread. Therefore, a lot of economic, social and health considerations have to be put in place to protect and ensure their safety (41, 45, 46).
Refugees in displacement camps constitute a greater population of the vulnerable groups that need to be given closer considerations during a pandemic. Over 10 million of people in WHO regions live in displaced and refugee settings. This is quite problematic and they must be considered when designing a policy response for influenza and other epidemic- and pandemic-prone acute respiratory diseases (41, 46).
4.10.3. Timely and Accurate Information Against False Information
Past pandemics have been closely associated with a surge in the spread of false information. Unfortunately but true, a lot of harm experienced comes from false health information or the lack of. During the Ebola outbreak in 2013, a lot of Nigerians were hospitalised due to ingestion of too much salt as it was rumoured to prevent the contraction of the virus. Fast forward to the COVID-19 pandemic, a lot of Asians died from ingesting excess alcohol as it was believed to be effective against the novel virus (47). Pandemics are commonly associated with high panic levels of the general public therefore, disseminating timely and accurate information to the general public can help prevent panic and abate worries (48). This will go a long way to ensuring that people are properly informed on how to behave, respond, prevent and protect themselves in the midst of a pandemic (49-51).
4.10.4. Health Systems Strengthening
One of the beauty of pandemics is that it has openly revealed to the world the lapses and weaknesses of the health system of many countries, especially low and middle income industries. There is a need to expand the capacity of local and national health centres in preparedness for future threats (49). Our health systems are not designed properly to be able to cater for a public health emergency in terms of facilities, infrastructures and medical personnels. As the revised 2013 pandemic guidance notes: “The objectives of emergency risk management for health are to: strengthen capacities to manage the health risks from all hazards; embed comprehensive emergency risk management in the health sector; and enable and promote multi sectorial linkage and integration across the whole-of government and the whole-of-society” (52-56).
4.10.5. Adherence to Laid-Down Guidelines
Some measures put in place to curtail the spread of the virus such as social distancing, quarantine, mask-wearing, and use of hand sanitizers should be adhered to strictly. This will likely help decrease the risk of infection. Also, resilient health systems should be built, and therapeutic protocols followed.
5. Conclusions
Pandemics have long been in existence and have continued to influence the world in more ways than we thought was possible. The world has recorded a lot of casualties in the past but they have not been without profitable lessons and useful insights that will ensure our preparedness to facing off future pandemic threats. From past pandemics and with the current novel coronavirus pandemic which shares uncanny similarities with other respiratory viruses, it is evident that we must adopt better and effective strategies to mitigate the present COVID-19 and prevent future pandemics. Challenges such as non-compliance or partially compliance with health protocols among population are also commonly found in many countries, especially low and medium income countries e.g. African countries. Measures like physical distancing are effective in preventing transmission of COVID-19 and should be employed in the future for similar respiratory infectious diseases (57).
Another measure is to boost immune systems by eating healthy and taking supplements which is very useful against combating an infection (58). In order to reduce the number of patients’ visits to the hospital during a pandemic like COVID-19 due to the possibility of getting the virus, the gospel of telemedicine should be preached and strongly encouraged (59).