1. Background
There is a rapid transition from traditional to digital platforms in medical education and clinical practice (1). This technologically-driven transition (2) has significantly altered communication, teaching, learning, and practice patterns of different healthcare professions (3). Advances in mobile technology and increased smartphone ownership have paved a bright way for the transition to digital platforms in medical education and clinical practice (4). Now healthcare professionals use smartphones for their daily activities (1, 4). Smartphone technologies have combined telephone communications and informatics in portable devices (5, 6). As a result of increased penetration of smartphones, app usage is also growing, as these applications are projected to play a significant role in supporting education generally, particularly medical education (3).
Thus, smartphone applications have become an important and useful component of medical education (7). As such, some medical training institutions have accredited smartphone-based educational, medical apps resources for training their students (Robinson et al., 2013). It's widely believed that these smartphone-based medical apps can facilitate quick access to medical information and deliver optimal learning outcomes (5, 7-9).
Many medical universities have embraced this new technology as a part of training their medical students by promoting medical apps resources on their websites and maintaining licenses for these apps (10). While the transition to mobile learning in medical education is on the rise in the developing countries (11), they may face significant and peculiar barriers in adopting this new platform, especially those in sub-Sahara Africa (12). It is reported that students in developing countries are not eager to use medical apps (13). Based on the literature, most students believed that medical apps could restrain them from their education and acts as a hurdle to their academic pursuit (14). Also, medical students appeared uncertain about the superiority of medical apps to medical books (15). Another study reported that smartphones can act as a source of nuisance as depicted by most medical students because of frequent notifications of applications and more use of social networking apps, especially during study hours (16). As such, using smartphones for learning has not been fully incorporated into medical education methods in the majority of African medical schools (17).
2. Objectives
The current study aimed to determine knowledge, perception, and medical apps use among medical students of a Nigerian University.
3. Methods
In this cross-sectional study, 320 medical students (193 males and 127 females) are participated. The sample size was estimated using the following formula (18):
where, n = sample size, N = population size (1568), and e = error margin estimated at 0.05.
Thus, n = 1568/ 1 + 1568 (0.05)2.
Hence, the total sample size was calculated as 320. To allow for non-response and invalid data, the sample size was increased by 10%. Therefore, the sample size was increased to 352. A response rate of 90.9% (i.e. 320/352*100) was obtained in this study. The respondents were medical students in Dentistry, Medicine, Nursing, Occupational Therapy, and Physiotherapy at the Obafemi Awolowo University, Ile-Ife, Nigeria. The study was carried out over a period of 5 months (March-July, 2020).
The face and content validity was determined by obtaining experts’ opinions on the appropriateness and representativeness of items to measure the targeted construct. A questionnaire was used to obtain information on knowledge, perception, and use of medical applications, as well as socio-demographic characteristics. This questionnaire contained four sections and was developed based on Koh et al., (19), as follow: (a) information about the demographic characteristics and mobile phone ownership and usage; (b) using medical apps; (c) perception about medical apps; and (d) information on barriers and facilitators of medical apps use. The study is approved by the Ethics Committee of the Institute of Public Health, Obafemi Awolowo University, Ile-Ife, Nigeria. Besides, written informed consent was obtained from all respondents. The confidentiality of information was ensured.
3.1. Data Analysis
Data were summarized using descriptive statistics of mean, standard deviation, frequency, and percentage. Thereafter, responses were transformed and scored as ‘one’ (correct) and "zero" (wrong). Analyses were performed on total scores. Based on percentile cut points, the levels were determined. For knowledge level, scores less than the median, between the median and the 75th percentile, and greater than the 75th percentile were defined as low, moderate, and high, respectively. While for perception, scores less and greater than the median were classified as poor and good, respectively. The Pearson chi-square test was used to evaluate the association between each of the knowledge, perception, and use of medical apps and respondents’ characteristics. Alpha level was set at P < 0.05. Data analysis was performed using IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. IBM Corp.
4. Results
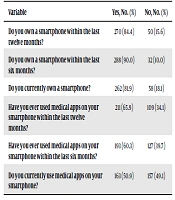
The socio-demographic characteristics of respondents are shown in Table 1. The mean age of respondents was 22.0 ± 2.47 years. Most of the respondents (40%) were within the age group of 21 - 23 years, male (60.3%), and of Christian religion (77.2%). The smartphone usage profile of respondents is shown in Table 2. As shown in the table, 90% and 84.4% of respondents owned a smartphone within the last twelve and six months, respectively, while 81.9% had a smartphone when the study was performed. Also, 65.9% and 60.3% of respondents had a history of using medical apps on their smartphones within the last twelve and six months, while 50.9% had a medical app on their smartphones when the study was performed.
| Variable | Values |
|---|---|
| Age (y) | 22.0 ± 2.47 |
| ≤ 20 | 99 (30.9) |
| 21 - 23 | 128 (40.0) |
| 24 - 27 | 82 (25.6) |
| 28 above | 11 (3.4) |
| Sex | |
| Male | 193 (60.3) |
| Female | 127 (39.7) |
| Religion | |
| Christians | 247 (77.2) |
| Islam | 73 (22.8) |
| Marital Status | |
| Single | 247 (77.2) |
| Married | 73 (22.8) |
| Tribe | |
| Yoruba | 264 (82.5) |
| Igbo | 24 (7.5) |
| Others | 32 (10.0) |
| Academic Level | |
| 200 | 92 (28.8) |
| 300 | 70 (21.9) |
| 400 | 71 (22.2) |
| 500 | 69 (21.6) |
| 600 | 18 (5.6) |
aValues are presented as No. (%) or mean ± SD.
| Variable | Yes, No. (%) | No, No. (%) |
|---|---|---|
| Do you own a smartphone within the last twelve months? | 270 (84.4) | 50 (15.6) |
| Do you own a smartphone within the last six months? | 288 (90.0) | 32 (10.0) |
| Do you currently own a smartphone? | 262 (81.9) | 58 (18.1) |
| Have you ever used medical apps on your smartphone within the last twelve months? | 211 (65.9) | 109 (34.1) |
| Have you ever used medical apps on your smartphone within the last six months? | 193 (60.3) | 127 (39.7) |
| Do you currently use medical apps on your smartphone? | 163 (50.9) | 157 (49.1) |
The findings on Knowledge and perception about medical applications, perception of using medical applications, and barriers to using medical applications are described in Table 3. Based on the results, most of the respondents agreed that medical apps cover communication between patients and healthcare professionals (75%), help with patients monitoring and surveillance (66%), have increased their level of medical education (70.6%), and are useful in personal health tracking (52.2%) (Table 3). Most of the respondents agreed that medical apps are essential tools for medical undergraduate (75.3%). However, many respondents agreed that medical apps are not superior to medical books (63.7%), as good as medical books (66.6%), and are not potential breaches of patients’ confidentiality (55.4%) (Table 3). Also, participants mostly agreed that medical apps can improve clinical decision-making (65.3%), save time academically and clinically (64.4%), allow faster access to national clinical practice guidelines (72.8%), allow faster access to common laboratory values (71.9%), and help in making differential diagnoses (66.6%) (Table 3). However, the most important barriers to the use of medical apps were not accrediting medical apps by valid health institutions (63.1%), lack of motivation in using medical applications (45.4%), and lack of adequate necessary network and communication infrastructures (51.9%). On the other hand, 70.4% of the respondents agreed that using smartphones for academic use is time-wasting (Table 3). The results concerning the association between knowledge of medical apps and socio-demographic characteristics (age, sex, and academic level) of respondents are described in Table 4. There was a significant association between knowledge on medical apps and each of age (χ2 = 38.79, P = 0.001) and academic levels (χ2 =24.88, P = 0.002). The results indicated that the majority of respondents (81. 9%) had high knowledge of smartphone-based medical-related apps (Table 4).
| Variable | SA, No. (%) | A, No. (%) | D, No. (%) | SD, No. (%) |
|---|---|---|---|---|
| Knowledge about medical applications | ||||
| Medical apps cover communication between patient and healthcare | 85 (26.6) | 155 (48.4) | 67 (20.9) | 13 (4.1) |
| Medical apps use help with patients monitoring and surveillance | 79 (24.7) | 132 (41.3) | 92 (28.8) | 17 (5.3) |
| My use of medical apps have increased my level of medical education | 95 (29.7) | 131 (40.9) | 60 (18.8) | 34 (10.6) |
| Medical apps are useful in personal health tracking | 72 (22.5) | 167 (52.2) | 80 (25) | 1 (0.3) |
| Medical apps aid in decision making | 88 (27.5) | 158 (49.4) | 72 (22.5) | 2 (0.6) |
| Medical apps help inpatient monitoring | 64 (20.0) | 117 (36.6) | 115 (35.9) | 24 (7.5) |
| Medical apps are essential tools for medical undergraduate studies | 80 (25.0) | 161 (50.3) | 50 (15.6) | 29 (9.1) |
| The use of medical apps help in diagnosis | 64 (20.0) | 117 (36.6) | 115 (35.9) | 17 (5.3) |
| Medical apps are superior to medical books | 17 (5.3) | 99 (30.9) | 123 (38.4) | 81 (25.3) |
| Medical apps are as good as medical books | 38 (11.9) | 175 (54.7) | 88 (27.5) | 19 (5.9) |
| Medical apps are inferior to medical books | 50 (15.6) | 100 (31.1) | 128 (40.0) | 42 (13.1) |
| Perception about medical applications | ||||
| Medical apps are essential tools for medical undergraduate studies | 80 (25.0) | 161 (50.3) | 50 (15.6) | 29 (9.1) |
| Medical apps are superior to medical books | 17 (5.3) | 99 (30.9) | 123 (38.4) | 81 (25.3) |
| Medical apps are as good as medical books | 38 (11.9) | 175 (54.7) | 88 (27.5) | 19 (5.9) |
| Medical apps are inferior to medical books | 50 (15.6) | 100 (31.1) | 128 (40.0) | 42 (13.1) |
| Medical apps can replace medical books | 68 (21.3) | 90 (28.1) | 82 (25.6) | 80 (25.0) |
| Medical apps supplement medical books | 61 (19.1) | 155 (48.4) | 67 (20.9) | 37 (11.6) |
| Medical apps provide useful medical information at ‘point-of-care’ | 72 (22.5) | 143 (44.7) | 74 (23.1) | 31 (9.7) |
| All medical students should own a smart phone | 88 (27.5) | 111 (34.7) | 84 (26.3) | 37 (11.6) |
| All medical students should use medical apps on their smart phone devices | 88 (27.5) | 109 (34.1) | 84 (26.3) | 39 (12.2) |
| Free medical apps are inferior in quality compared to paid apps | 41 (12.8) | 105 (32.8) | 145 (45.3) | 29 (9.1) |
| There are no dangers in using medical apps for patient care | 14 (4.4) | 108 (33.8) | 118 (36.9) | 80 (25.0) |
| There are potential breaches of patient’ confidentiality when using medical apps for patient care. | 3 (0.9) | 140 (3.8) | 133 (41.6) | 44 (13.8) |
| The use of medical apps will help in quick access to medical information and improves clinical management of patients | 91 (28.4) | 164 (51.3) | 53 (16.6) | 12 (3.8) |
| Perception of use of medical applications | ||||
| The use of medical apps improve clinical decision making | 89 (27.8) | 120 (37.5) | 83 (25.9) | 28 (8.8) |
| Medical apps use save time academically and clinically | 62 (19.4) | 144 (45.0) | 71 (22.2) | 43 (13.4) |
| Medical apps allow faster access to national clinical practice guidelines | 82 (25.6) | 151 (47.2) | 71 (22.2) | 16 (5.0) |
| Medical apps allow faster access to common laboratory reference values | 72 (22.5) | 158 (49.4) | 66 (20.6) | 24 (7.5) |
| Medical apps help in making differential diagnoses | 44 (13.8) | 169 (52.8) | 72 (22.5) | 35 (10.9) |
| Medical apps perform useful medical related calculations. (e.g. estimate creatinine clearance) | 65 (20.3) | 136 (42.5) | 70 (21.9) | 49 (15.3) |
| Medical apps allow faster access to reliable sources of medical knowledge | ||||
| Medical apps allow faster access to reliable sources of clinical and academic skills | 103 (32.2) | 148 (46.3) | 54 (16.9) | 15 (4.7) |
| Medical apps allow accurate medicine dosages calculation | 79 (24.7) | 115 (35.9) | 84 (26.3) | 42 (13.1) |
| Medical apps allow faster access to evidence-based medical practice | 79 (24.7) | 115 (35.9) | 84 (26.3) | 42 (13.1) |
| Barriers to the use of Medical Applications | ||||
| There is a lack of accreditation of medical apps by valid health institutions | 72 (22.5) | 130 (40.6) | 96 (30.0) | 22 (6.9) |
| I lack adequate skills to use medical applications | 34 (10.6) | 71 (22.2) | 165 (51.6) | 50 (15.6) |
| I do not have the motivation in using medical applications | 60 (18.8) | 85 (26.6) | 137 (42.8) | 38 (11.9) |
| I fear the lack of academic reliability of medical applications | 50 (15.6) | 89 (27.8) | 137 (42.8) | 44 (13.8) |
| The school lacks the necessary network and communications infrastructure | 82 (25.6) | 84 (26.3) | 100 (31.1) | 54 (16.9) |
| I lack knowledge about the benefits of medical apps | 56 (17.5) | 72 (22.5) | 146 (45.6) | 46 (14.4) |
| Using smartphones for academic use is time-wasting | 52 (16.3) | 173 (54.1) | 48 (15.0) | 47 (14.7) |
| I fear problems relating to problems relating to insecurity and confidentiality of information | 71 (22.2) | 68 (21.3) | 161 (50.3) | 20 (6.3) |
| I lack knowledge about awareness and medical apps benefits | 41 (12.8) | 68 (21.3) | 185 (57.8) | 26 (8.1) |
| Using medical apps for diagnostic and academic purposes will make me over-dependent | 22 (6.9) | 85 (26.6) | 150 (46.9) | 63 (19.7) |
| Variable | Knowledge | χ2 | P Value | ||
|---|---|---|---|---|---|
| Low, No. (%) | Moderate, No. (%) | High, No. (%) | |||
| Age (years) | 38.790 | 0.001 | |||
| ≤ 20 | 3 (0.9) | 6 (1.9) | 90 (28.1) | ||
| 21 - 23 | 9 (2.8) | 8 (2.5) | 111 (34.7) | ||
| 24 - 27 | 24 (7.5) | 7 (2.2) | 51 (15.9) | ||
| 28 above | 1 (0.3) | 10 (3.1) | |||
| Sex | 4.371 | 0.112 | |||
| Male | 16 (5.0) | 13 (4.1) | 164 (51.3) | ||
| Female | 20 (6.3) | 9 (2.8) | 98 (30.6) | ||
| Academic Level | 24.88 | 0.002 | |||
| 200 | 4 (1.3) | 3 (0.9) | 85 (26.6) | ||
| 300 | 11 (3.4) | 7 (2.2) | 52 (16.3) | ||
| 400 | 13 (4.1) | 2 (0.6) | 56 (17.5) | ||
| 500 | 8 (2.5) | 10 (3.1) | 51 (16.0) | ||
| 600 | 18 (5.6) | ||||
| Total | 36 (11.3) | 22 (6.9) | 262 (81.9) | ||
The association between socio-demographic characteristics (age, sex, and academic level) of respondents and their perception of medical applications is shown in Table 5. No significant association was observed between sex (χ2 = 1.051, P = 0.305), academic level (χ2 = 8.244, P = 0.083), and respondents’ perception of medical apps. However, there was a significant association between age and respondents’ perception of medical apps (χ2 = 13.554, P = 0.004). Also, 59.4% of the respondents had a good perception of medical apps (Table 5).
| Variable | Perception | χ2 | P Value | |
|---|---|---|---|---|
| Poor, No. (%) | Good, No. (%) | |||
| Age (years) | 13.554 | 0.004 | ||
| ≤ 20 | 46 (14.4) | 53 (16.6) | ||
| 21-23 | 51 (15.9) | 77 (24.1) | ||
| 24-27 | 24 (7.5) | 58 (18.1) | ||
| 28 above | 9 (6.9) | 2 (1.1) | ||
| Sex | 1.051 | 0.305 | ||
| Male | 74 (23.1) | 119 (37.2) | ||
| Female | 56 (17.5) | 71 (22.2) | ||
| Academic level | 8.244 | 0.083 | ||
| 200 | 44 (13.8) | 48 (15.0) | ||
| 300 | 19 (5.9) | 51 (15.9) | ||
| 400 | 31 (9.7) | 40 (12.5) | ||
| 500 | 27 (8.4) | 42 (13.1) | ||
| 600 | 9 (2.8) | 9 (2.8) | ||
| Total | 130 (40.6) | 190 (59.4) | ||
The results on the association between long-term use/current use of medical apps and socio-demographic characteristics are shown in Table 6. A significant association was found between long-term use of medical apps and each of age (χ2 = 30.541, P = 0.0001) and academic level (χ2 = 19.27, P = 0.001). Also, there was a significant association between current use of medical apps and each of age (χ2 = 12.018, P = 0.007) and academic level (χ2 = 11.297, P = 0.002).
| Variable | Use of Apps | |||
|---|---|---|---|---|
| Yes, No. (%) | No, No. (%) | χ2 | P Value | |
| Long Term Use | ||||
| Age (years) | 30.541 | 0.001 | ||
| ≤ 20 | 82 (25.6) | 17 (5.3) | ||
| 21-23 | 85 (26.6) | 43 (13.4) | ||
| 24-27 | 36 (11.2) | 46 (14.4) | ||
| 28 above | 8 (2.5) | 3 (0.9) | ||
| Sex | 0.97 | 0.325 | ||
| Male | 94 (29.4) | 99 (30.9) | ||
| Female | 69 (21.6) | 58 (18.1) | ||
| Academic Level | 19.27 | 0.001 | ||
| 200 | 49 (15.3) | 43 (13.4) | ||
| 300 | 38 (11.9) | 32 (10.0) | ||
| 400 | 24 (7.5) | 47 (14.7) | ||
| 500 | 36 (11.2) | 33 (10.3) | ||
| 600 | 16 (5.0) | 2 (0.6) | ||
| Total | 163 (50.9) | 157 (49.1) | ||
| Current Use | ||||
| Age (years) | 12.018 | 0.007 | ||
| ≤ 20 | 50 (15.6) | 49 (15.3) | ||
| 21-23 | 53 (16.6) | 75 (23.4) | ||
| 24-27 | 54 (16.9) | 28 (8.8) | ||
| 28 above | 6 (1.3) | 5 (1.6) | ||
| Sex | 1.608 | 0.205 | ||
| Male | 122 (38.1) | 71 (22.2) | ||
| Female | 89 (27.8) | 38 (11.9) | ||
| Academic Level | 11.297 | 0.02 | ||
| 200 | 66 (20.6) | 26 (8.1) | ||
| 300 | 46 (14.4) | 24 (7.5) | ||
| 400 | 42 (13.1) | 29 (9.1) | ||
| 500 | 40 (12.5) | 29 (9.1) | ||
| 600 | 17 (5.3) | 1 (0.3) | ||
| Total | 211 (65.9) | 109 (34.1) | ||
5. Discussion
This study investigated knowledge, perception, and use of medical apps among Nigerian medical students. Harnessing the potentials of apps for healthcare has become a focal point of innovation (20). With students believing that mobile technologies contribute to their medical education, it remains no surprise that institutions concerned with medical education and practice are beginning to unlock this potential. Specifically, Robinson et al. (21), in a study on clinical medical students in the United Kingdom, found that the students were positive towards the concept of smartphones as future educational aids; however, they surmised that the affordability of such devices is important for their universal acceptance.
Most medical students perceived medical apps as essential tools for undergraduate medical studies and felt that all medical students should own a smart device and use medical apps installed on their devices (20). Thus, students are smartphone viable populations than the older ages, and the apparent lack of insight into medical students' opinions regarding medical applications is unexpected, given the popularity of smartphone usage in medical settings (22). Dennison et al. (2013) showed that younger adults are considerably more likely to use smartphone-based medical apps, and the likelihood of adults' medical apps use decreases significantly with age. Thus, the young adult population seemed to be a suitable age category for this study (23).
Based on the findings, most of the students currently owned smartphones, and an appreciable number of students were using medical-related apps, which is similar to the study carried out by Payne (24) in the United Kingdom where 79% of medical students owned smartphones and were using medical apps for self-learning in clinical environments. Furthermore, in the present study, 81. 9% of the students had high knowledge of smartphone medical-related apps. Also, about 60% of the students had a positive perception of medical apps, while 80% of them had a positive perception of using medical apps. This finding is in line with the study carried out by Koh, et al., (19) on medical students’ perceptions regarding the impact of mobile medical applications on their clinical practice. They found that 88% of medical students had positive perceptions toward medical apps and agreed that these apps have a positive impact on their studies and clinical practice. Similarly, in the present study, medical students reported little awareness about the potential breach of patients' confidentiality with the use of medical. Koh et al., (19) found that medical students had little awareness about the potential breach of patient confidentiality with the use of medical apps.
Also, according to the findings, not accrediting medical apps by valid health institutions, lack of adequate skills and motivation in using medical apps, and lack of adequate necessary network and communications infrastructures were identified as barriers preventing students from using medical apps for academic purposes. According to Ibrahim et al. (25), some of the barriers to using smartphones and medical apps include inadequate technology and poor design issues; cost and inadequate security; the need for skills and competence, as well as learning necessities that bother in face-to-face teaching, time-demanding nature of e-learning, computer anxiety, and lack of institutional support. This study showed that medical apps have an important role in diagnosis and making decisions, personal health tracking, and monitoring patients. Similar findings are reported by Van et al., (26), which revealed that medical apps are useful in learning, decision-making, medical calculation, and better interpretation of clinical tests.
Furthermore, this study showed that knowledge about medical apps was significantly influenced by age and academic level. Also, the perception of medical apps was found to be significantly associated with age. Similar patterns are reported by Koh et al., (19), who reported that socio-demographic (age, sex, marital status, and class) characteristics were significantly correlated with perception of medical apps. Similarly, the present study found that the use of medical apps was significantly influenced by age and academic level. Similar patterns are observed by Sandholzer et al., (27), who reported that socio-demographic factors (age and academic level) were significantly correlated with the use of medical apps. The findings of the present study indicate the popularity of smartphones among medical students at the College of Health Sciences, Obafemi Awolwo University, Ile-Ife, Nigeria.
Also, several students were using medical apps on their smartphones, and most of them had a positive perception towards medical-related apps. This empirical finding is valuable for University administrators and educators in Nigeria, and possibly other countries in sub-Sahara Africa, to make decisions regarding adopting mobile platforms in medical education. Currently, more than 13,000 medical apps are available for smartphones, both android and iOS (20, 24). Furthermore, a market survey has indicated that smartphone penetration in Nigeria is so high so that currently, about 25 to 40 million Nigerians are using smartphones, and it is expected to grow to more than 140 million by 2025 (28). However, as it currently stands, medical institutions in Nigeria are yet to take advantage of the high penetration of smartphones for medical training.
In conclusion, smartphones and their applications are widely using by Nigerian medical students. Also, the students had high knowledge and positive perception toward using medical apps, which age and academic levels are major contributors.