1. Background
In most countries, undergraduate medical students follow books published by private publications as basic study materials. Foreign publishers of developed countries often ignore public health issues pertaining to developing nations. Most of these books do not include community-oriented World Health Organization (WHO) recommended guidelines. Government medical councils usually do not publish standard books. As a result, undergraduate medical students who are tomorrow’s doctors remain unaware of newer WHO guidelines. This adversely affects their case identification and management skill and eventually negatively influence public health.
According to WHO estimates, 5.2 million children died mostly from preventable and treatable causes before they reach their fifth birthday in 2019. Children aged 1 month to 4 years accounted for 2.8 million of these deaths. Pneumonia, diarrhea, and malaria are the leading causes of death in children under 5 years of age. Sub-Saharan Africa and Southeast Asia contributed to 80% of these deaths (1).
According to an estimate, pneumonia caused 900,000 deaths among children under 5 years of age in 2015. About 32 % of these global deaths were from India alone (2). As per WHO estimates, nearly 1.7 billion cases of childhood diarrheal diseases occur every year. Diarrheal diseases are the second leading cause of death and kill around 525,000 children younger than 5 years of age annually (3).
Integrated management of childhood illness (IMCI) strategy was launched in the mid-1990s by WHO and United Nations Children’s Fund (UNICEF) (4, 5). Studies done in Brazil, Peru, Uganda, and Tanzania established the efficacy and cost-effectiveness of the IMCI strategy in the management of childhood illnesses (6-9).
Previous studies have established the overall effectiveness of IMCI in reducing child mortality. However, only a few studies have directly quantified the improvement in case identification and management skills among health care workers. Studies assessing the impact of training among undergraduate medical students are even more limited.
2. Objectives
Using the IMCI guideline, this current study was done to quantify the skill enhancement using the standard IMCI module training for 12 days. Findings of this study highlight the need to reorient medical pedagogy based on the individual health goals of each country.
3. Methods
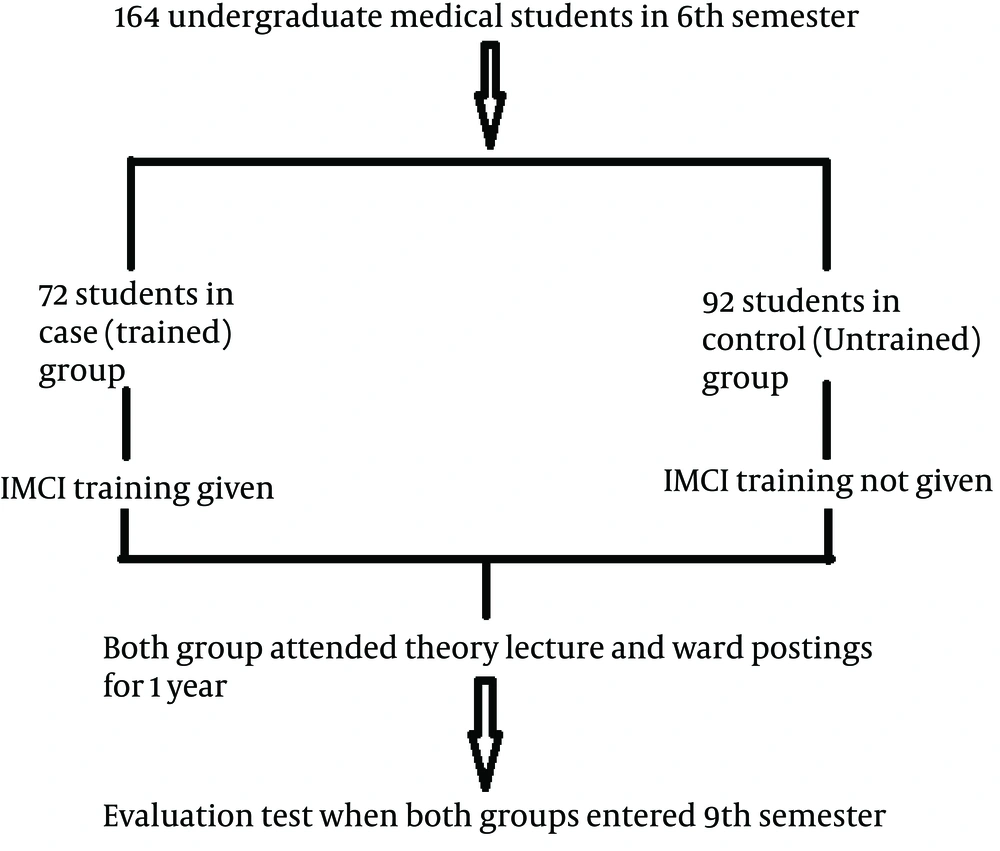
This case-control study was done on 144 undergraduate medical students in the 6th semester at Lala Lajpat Rai Memorial Government Medical College, Merrut, Uttar Pradesh province, India. The study was approved by the studied hospital ethics committee. Chit-Pull system was used to randomize 72 and 92 undergraduate medical students in the case (trained) and control (untrained) group, respectively.
Participants of the trained group underwent standard IMCI module training over 12 days. Theory lectures were given 3 h each day for 6 alternate days with the help of the interactive printed module, PowerPoint slides, and video tools. Each theory lecture was followed by 3 h of relevant case demonstration and discussion session in the children’s ward. Untrained group participants were not given IMCI training. The attendance of each student was recorded on each day of the training session (Figure 1).
In the next year, participants of both groups attended regular theory lectures in the children’s ward clinics. When participants entered the 9th semester, they were evaluated through a structured questionnaire. It comprised of 50 clinical case scenarios covering all aspects of IMCI, having one or more correct answers with audio-visual hints and tools. Prior to the assessment, the participants were taken into confidence, and the purpose of the study was explained to them. Unwilling students were excluded from the study. Students who received IMCI training but eventually did not appear in the evaluation were also excluded. Feedback of students was taken on a written Performa after evaluation.
Data were collected on a Microsoft Excel sheet and analyzed using Epi info statistical software for epidemiology developed by the Centers for Disease Control and Prevention (CDC) in Atlanta, the USA, available for Microsoft windows. Categorical data were analyzed by chi-square test. Karl Pearson coefficient of correlation was used to analyze the association of marks scored and attendance percentage.
4. Results
Participants of the trained group showed significantly higher skill levels in identification and management of general danger signs, pneumonia, dehydration, persistent diarrhea, dysentery, fever, malnutrition, and anemia (P < 0.05). However, no significant difference was found in the assessment of immunization status (P > 0.05) (Table 1).
| Diagnosis and Management Skill | Correct Responses in the Trained Group (N = 72) | Correct Responses in the Untrained Group (N = 92) | P-Value |
|---|---|---|---|
| Identifying danger sign | 56 | 17 | 0.012 |
| Pneumonia | 40 | 24 | 0.026 |
| Dehydration | 60 | 60 | 0.043 |
| Persistent diarrhea | 50 | 22 | 0.015 |
| Dysentery | 58 | 12 | 0.007 |
| Fever | 50 | 40 | 0.033 |
| Malnutrition | 62 | 25 | 0.019 |
| Anemia | 35 | 25 | 0.030 |
| Immunization | 62 | 70 | 0.067 |
In the trained group, 56 (75%) participants had 100% attendance, and 7 (11%) participants had 83% attendance in training sessions. A strong positive correlation (r = 0.87) existed between the attendance percentage of the trained group participants and marks scored in the evaluation (P < 0.001) (Table 2).
| Attendance, d | Number of Students | Average Marks Obtained, % |
|---|---|---|
| 6 | 3 | 50 |
| 8 | 6 | 62 |
| 10 | 7 | 71 |
| 12 | 56 | 75.6 |
ar = 0.87; P < 0.001.
More than 90% of students gave excellent or very good feedback regarding IMCI training (Table 3).
| Feedback | Number of Students, No. (%) |
|---|---|
| Excellent | 33 (45.8) |
| Very good | 18 (25) |
| Good | 15 (20.8) |
| Average | 1 (1.4) |
5. Discussion
National health priorities of developing and developed countries are different. Unlike developed countries, under-equipped health system in developing countries is struggling with malnutrition, diarrhea, pneumonia, and malaria. Medical education in developing countries needs to put greater emphasis on these challenges, which continue to be a major cause of mortality in children aged < 5 years. Authors of foreign publications give little importance to these ailments. The WHO guidelines on these ailments are rarely included in foreign books. IMCI is one of several WHO-recommended strategies, which has revolutionized the management of common childhood illness. However, it has been ignored in most of the foreign medical books.
The rationale for the integrated strategy adopted in IMCI is that children brought for medical treatment in the developing world are often suffering from more than one condition. This overlap means that a single diagnosis may not be possible or appropriate and treatment may be complicated by the need to combine therapy for several conditions (10-17).
Multi-country evaluation (MCE) was conducted in Brazil, Peru, Uganda, and the United Republic of Tanzania assessed the cost-effectiveness of the IMCI strategy. IMCI implementation resulted in lower under-five mortality, improved nutritional status, and at the same time, and it costs up to six times less per child compared with the conventional approach (6-9).
In a randomized trial done in Bangladesh, Arifeen et al. (18) reported lower child mortality rate, higher exclusively breastfeeding rate, lower prevalence of stunting in children aged 24 - 59 months, improved health-worker skills, health-system support, family and community practices and increased care-seeking for illnesses in rural areas where IMCI was implemented.
Few studies have been done to assess the impact of IMCI training on case identification and management skills among health care workers. In a study done in Ethiopia, Simoes et al. (19) reported better performance by basic health care workers in the detection of individual clinical signs and classification of pneumonia or severe pneumonia, dehydration, dysentery, and malnutrition.
A study done in India by Rani et al. (20) in 2009 reported that IMCI training of medical students resulted in a significant improvement in case identification, making a correct clinical diagnosis, providing emergency treatment, and making referral decisions.
The current study also reported similar findings. Compared with the untrained group, IMCI-trained students are more likely to recognize general danger signs (P = 0.012). General danger signs include convulsions, lethargy/unconsciousness, inability to drink/breastfeed, and vomiting. Being more able to identify danger signs ensures that fewer severely ill children who need urgent attention will be overlooked.
Similarly, participants of the trained group performed significantly well in the diagnosis and management of dysentery (P = 0.007), persistent diarrhea (P = 0.015), and dehydration (0.043) compared with participants of the untrained group. Diarrheal diseases are the second leading cause of mortality in children aged < 5 years and a major cause of malnutrition (3). Skill acquired through IMCI training will help medical students in the diagnosis and management of diarrheal diseases and reduce mortality due to these ailments.
Participants of the trained group scored significantly higher in diagnosis and management of malnutrition (P = 0.019), pneumonia (P = 0.026), anemia (P = 0.030), and fever (P = 0.033). Pneumonia is the major cause of death in cases younger than 5 years (2). Malnutrition is a known risk factor contributing to higher mortality in infectious and diarrheal diseases. IMCI training will help in morbidity and mortality reduction in these cases.
Massive government emphasis on immunization in the regular medical course and mass media has led to the increased awareness regarding immunization in both trained and untrained group participants. This probably is the reason behind no significant improvement regarding the assessment of immunization status.
A strong positive correlation between attendance percentage and marks scored by participants suggests that the IMCI module is highly effective in the skill enhancement of trainees.
This study is significant as it highlights the direct impact of IMCI training on the skills of medical students. Most studies have highlighted the impact of IMCI implementation on the overall mortality and morbidity of children. This study has a few limitations. Since our study was part of a post-graduate thesis, it was done at a single center with a limited number of participants. Furthermore, more studies should be done assessing different centers with a greater number of participants.
5.1. Conclusions
This study indicated that IMCI training of undergraduate students for 12 days is very effective in improving performance in the diagnosis and management of childhood illnesses. Inclusion of IMCI in undergraduate medical pedagogy and curriculum will significantly help medical students when they leave medical schools and resume the role as primary health physicians in the government health facility. These trained doctors can also play a key role in the IMCI training and support of health workers.
Regulatory bodies entrusted with the responsibility of development and implementation of the medical curriculum in developing countries should lay more emphasis on community-oriented WHO guidelines in the endeavor of achieving national health goals.