1. Background
Electroconvulsive therapy (ECT) is a therapeutic approach that was used in the treatment of mental disorders for the first time in the 1930s (1). The effect of this method on severe depression, controlling suicidal thoughts, and schizophrenia has been proven (2). Even in some studies, the use of ECT has been found more effective in treating patients exposed to suicide than drug therapy. Although some studies have reported complications such as epilepsy, brain damage, pain, and short-term memory impairment as the main complications of using ECT (3), more than 100,000 patients in the United States and more than one million patients worldwide are treated annually with ECT (4). Today, due to the high prevalence of mental disorders and despite its complications and high productivity, this treatment is considered as a useful and effective method. ECT is often done by a psychiatrist with the presence of an anesthetist with at least one nurse’s full support. In fact, trained nurses are responsible for organizing the provision of ECT. So, they act as a team at the patient’s bedside. Physicians join the team only for a short time, and these are the nurses who take the overall responsibility before and after performing the procedure (5).
Nurses play an important role in ECT because they are in full contact with the patient before, during, and after the procedure. The performance of the nurses who take care of patients in ECT room has a direct impact on the quality of implementation and effectiveness of this treatment (6). The World Health Organization (WHO) recommends that teamwork has a significant impact on patient safety, especially when all team members follow a single procedure. Educational exercises for nurses responsible for caring in ECT can strengthen their ability and skill in team performance (7). The presence of experienced nurses in ECT department, who are able to implement ECT, reduces complications and improves service delivery to patients. Studies have also shown that work-related factors such as support by the director and colleagues in ECT department play an important role in the quality of care (8). Therefore, nurses act as step-by-step coordinators and regulators of care measures during ECT. For example, there are two centers for training psychiatric nurses in performing ECT in England, where skilled nurses are trained by psychiatrists and upgrade their abilities to the level of physicians to manage this therapy (5). Performing ECT is like learning driving for nurses, because this method should be done step-by-step, with a regular arrangement. Part of this skill is to become familiar with these steps and to create mental confidence for taking each step during care provision in ECT process without having to mark each one in a checklist (9). Nurses who achieve full proficiency level in implementing ECT dominate the whole team’s performance and take a good position in care coordination and care control. Nurses may be anxious about their ability to control seizures, as well as making quick decisions about what to do immediately. So, they need practice to gain confidence in team leadership and keep calm under pressure (10, 11).
Today, theoretical knowledge and practical skills of ECT in all parts of the world are considered as traditional outpatient training with the current ECT tool, and there is no standard method for achieving the competency of its implementation by caregivers. This could reduce the ability of the current and future generations of caregivers, endanger patient safety, and ultimately increase the risk of ECT-related complications (12). Several studies have expressed concerns about the obvious weaknesses in the field of skills, competence, and supervision in ECT (13, 14). Therefore, this study aimed to find a method to enhance the skill and competence of ECT caregivers. One of the methods used to train nursing skills is simulation, which is a technique or tool for creating the features of real phenomena (6).
Simulation-based medical education (SBME), as a teaching method, is the activities that imitate a real clinical setting and is designed to demonstrate processes, decision making, and critical thinking using methods such as role play and tools such as educational films and mannequins (15). There are nine kinds of simulation, including low-tech (static) trainer, simulated patients, screen-based computer simulator, complex task trainers, integrated simulator, human patient simulator, low fidelity, moderate fidelity, and high fidelity. This kind of simulator can be conducted in the two settings, including off-site and in situ (16-18). Despite conducting some studies on the effect of simulation-based training in nursing, there is little empirical evidence regarding the evaluation of the results of using these methods (19-21). Among the various simulation methods, simulation implementation can be used in skill training in care during ECT. Implementing simulated scenarios in special conditions by learners allows them to develop their skills and obtain the necessary qualifications, besides gaining experience without any fear and anxiety caused by injuring patients. Therefore, using this method in nursing leads to providing safe care and favorable outcomes for the patient (16).
The learner has an active participation in the simulation method and collaborates with others as a member of the team to solve problems and make decisions using critical thinking. In the simulation method using mannequins, the learners take feedback from the mannequin while they take care of mannequin and directly observe and experience it. In question-and-answer method, an opportunity is given to the learner to review his/her activity. In fact, s/he can experience situations that are not encountered in real clinical settings (15, 16).
With regards to these explanations and considering the high-risk and vital nature of ECT process, as well as the subsequent intensive, essential, and life-saving cares, it is necessary to examine skill training and competency enhancement methods in nurses who provide ECT care. Simulation in small groups has been used as a well-known method of skill training in nursing in several cases, and it can be effective in completing clinical knowledge and operational capabilities of nurses. The literature search showed that no study has ever reported the methods to improve clinical skills of nurses in ECT, and there is a serious lack of information and research results both in Iran and worldwide. Also, few studies have targeted psychiatrists and their assistants.
2. Objectives
This study aimed to determine the effect of simulation in small groups on developing the quality of care in nurses in ECT department.
3. Methods
3.1. Study Design and Research Samples
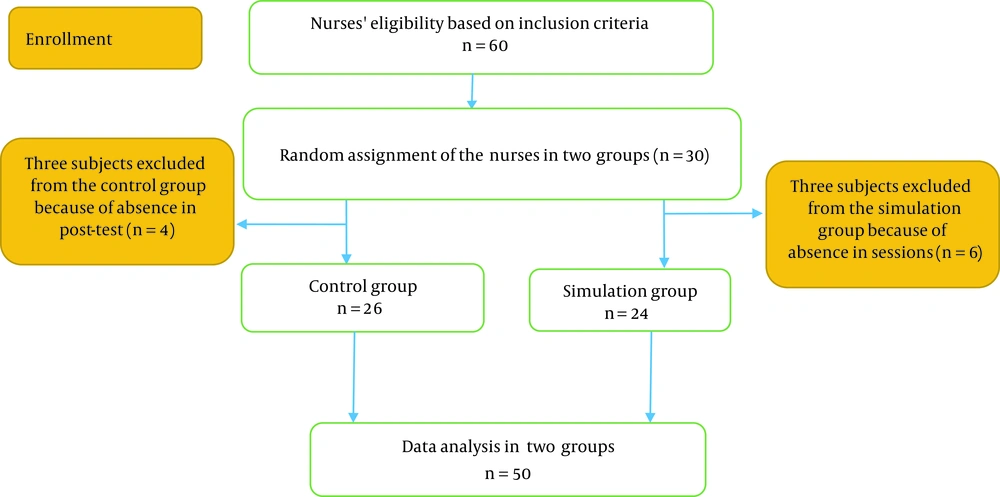
An experimental study with a two-group design before and after the intervention was adopted. The research population included all nurses working in ECT centers of Golestan and Salamat university hospitals in Ahvaz, Iran. Due to the limited number of nurses providing cares in ECT, sampling was done in an accessible manner. Finally, 60 psychiatric nurses who met the inclusion criteria were selected and randomly allocated into two groups of intervention and control.
The inclusion criteria were as follows: work experience in ECT department for six months or more as a direct provider of patient care; a steady presence in the intended department as permanent personnel and coordination with relevant assistants and psychiatrics; willingness to participate in the study; and participation in both pre-test and post-test phases. Sampling and research implementation were carried out in the second six months of 2018. To prevent the dissemination of information and the transfer of educational experiences between the individuals, the nurses were recruited from different working shifts. First, the observers were selected and oriented for data gathering. The selected subjects participated in a 2-hour session, and basic educational materials, criteria, frameworks of the study, and research checklist were explained to all subjects. Then, four trained ECT personnel were assessed in each of the three stages (before, during, and after the procedure) on the patients’ bedside in the presence of the researcher, and the probabilistic ambiguities were raised and resolved. In the next step, a pre-test was performed by a tool designed to observe all participants before intervention in a real setting and at the bedside of patients under ECT, and scores were recorded. Finally, 50 nurses (24 intervention vs. 26 control) finished SBME and participated in the post-test (Figure 1).
3.2. Instruments
Data collection instruments in this study included two parts. The first part included a questionnaire for collecting demographic information, and the second part included a checklist developed by Kaur (2012) for investigating the quality of nursing care in ECT. This checklist contains 115 items that assess ECT nursing care in four sections: before, during, after, and checking patient status. The first section on pre-ECT procedures includes three subscales of patient preparation (17 items), equipment preparation (37 items), and nurse equipment and responsibilities (5 items). These items scored (yes =1, no=0), and the sum of them was considered as the total of every individual. This checklist was designed and validated in 2012, and it is one of the few tools developed to investigate ECT nursing care. The validity of this checklist was reviewed and approved by its creators based on the Delphi method. To verify the reliability of the instrument, internal consistency method was used with Cronbach’s alpha coefficient equal to 0.86. The Cohen’s Kappa coefficient was also calculated for the reliability between evaluations, which was reported to be 0.94 (22).
3.3. Research Intervention
The designed intervention was performed only in intervention groups with 1-week interval from pre-test. The low-tech (static) trainer was used for SBME, which had two parts. In the first part, members of the intervention group attended in a briefing on care criteria immediately before, during, and after ECT, and discussed the importance, basics, and application of cares. Then, 25 nurses were randomly assigned into five small groups consisting of 5 individuals in each group. The second part consisted of three sessions of training, group discussion, and simulation in each small group. These sessions were held in one of the ECT rooms routinely used by the group, even though it was inactive during the session. The purpose of the researcher was to ensure that the conditions and the space for reviewing cares were as close as possible to the actual working conditions and space of the participants, and that all ECT tools and equipment were available to carry out simulation in the best way. Educational replica (models) was used in simulation, and all the dimensions of positioning, placement of the venous access path, patient coverage, closure of barometer cuff, pulse oximeter, and ECT electrode coupling were applied to the replica similar to the real setting. The small group members discussed team coordination for the more effective use of ECT care criteria, including task management, teamwork, position awareness, and decision making, and finally practiced and reviewed performing cares in simulation in the actual space of ECT department. The researcher was the facilitator of discussion and simulation. The facilitator tried to encourage the participants to express their experiences during practice and to support discussion and exchange of views. Also, during discussion and practice of simulation, important care points, and possible mistakes were noted. In order to prevent bias between the participants, they were requested not to disclose the framework and details of the sessions outside the session. In the final stage, one week after the last session in both groups, the post-test was performed in the actual working condition at the bedside of the patients by the same observers who held the pre-test. Observers were unaware of which nurses were in the intervention group and which were in the control group. In both pre-test and post-test stages, the observers completed the checklist with numerical criteria. Finally, total score of each sample in each test was calculated by adding up all the scores.
3.4. Ethical Considerations
In this study, no therapeutic or pharmaceutical interventions effective on the health and safety of patients were performed. The required permissions were obtained from the Vice Chancellor for Research of Ahvaz Jundishapur University of Medical Sciences, Iran, and the intended medical centers (ethics code: IR.AJUMS.REC.1397.288 and registration code: IRCT20181210041915N1). The provisions, methods, and procedures of research were described to all participants who voluntarily participated in the study. After the end of the study, the educational content was taught to the control group as well.
3.5. Statistical Analysis
The normality of data was assessed using the Shapiro-Wilk test. Chi-square test (Fisher’s exact test) was used to examine the relationship between qualitative variables. Also, independent t-test or its non-parametric equivalent (Mann-Whitney test) was used to compare quantitative variables between the two groups. The chi-square test and t-test were applied to compare categorical and continuous variables, and a P-value less than 0.05 was set as a statistically significant level. Statistical analyses were carried out using SPSS software (version 18.0).
4. Results
Out of 50 participants in the study, 21 females (87.5%) and three males (2.5%) were in the intervention group, and 19 females (73.1%) and seven males (26.9%) were in the control group. The mean age of participants was 31.50 ± 7.26 and 31.0 ± 6.5 years in the intervention and control groups, respectively. The mean work experience in ECT department was 58 months for the intervention group and 54 months for the control group. The demographic characteristics of the subjects are presented in Table 1.
| Variables | Intervention | Control | P-Value |
|---|---|---|---|
| Sex | 0.294 | ||
| Female | 21 (87.5) | 19 (73.1) | |
| Male | 3 (12.5) | 7 (26.9) | |
| Marriage | 0.227 | ||
| Single | 10 (41.7) | 6 (21.3) | |
| Married | 14 (58.3) | 20 (76.9) | |
| Job status | 0.951 | ||
| Permanent | 12 (50) | 15 (57.7) | |
| Temporary to permanent | 5 (20.8) | 5 (19.2) | |
| Projective | 6 (25.5) | 5 (19.2) | |
| Contractual | 1 (4.2) | 1 (3.8) | |
| Age (y) | 31.50 ± 7.26 | 31.0 ± 6.5 | 0.667 |
| Work experience (mo) | 76.181 | 71.849 | 0.969 |
| Working experience in the psychiatric ward (mo) | 58.199 | 54.324 | 0.969 |
aValues are expressed as No. (%) or mean ± SD unless otherwise indicated.
As shown in Table 2, there was no significant difference between the mean scores obtained in the pre-test (before the intervention) in the subscale of nursing care quality tool in ECT in both intervention and control groups (P < 0.05).
| Intervention | Intervention | Control | P-Value |
|---|---|---|---|
| Pre- ECT | |||
| Preliminary preparation | 6.1 ± 1.14 | 8 ± 91.282 | 0.387 |
| Routine preparation | 7.75 ± 0.442 | 7.76 ± 0.429 | 0.875 |
| Preparation of equipment | 48.70 ± 5.025 | 49.65 ± 3.88 | 0.605 |
| Immediately before shifting the patient to ECT room | 5 ± 0.0001 | 5 ± 0.000 | 0.99 |
| On ECT table | 4 ± 0.0001 | 3.96 ± 0.196 | 0.337 |
| During ECT | 9.196 ± 1.007 | 9.65 ± 0.845 | 0.058 |
| Post-ECT | 8.083 ± 0.88 | 8.57 ± 1.026 | 0.068 |
| Checking the patient status | 9.54 ± 0.508 | 9.61 ± 0.571 | 0.502 |
Findings of the paired t-test show the comparison of the mean scores in post-test (after running the intervention) in the subscales of "ECT nursing care quality tool" in the intervention and control groups. The results of evaluating the quality of patient’s primary preparation, post-ECT measures, and checking patient’s status were significantly different between intervention and control groups (P < 0.05). This indicates the positive impact of intervention in improving the quality of care in the intervention group compared to the control group in these three areas. The results obtained from this table show that the mean scores obtained in pre-test and post-test stages in the intervention group from the initial preparation subscales, preparation of tools and equipment, measures during ECT, post-ECT measures, and checking patient's status were significantly different (P < 0.05) (Table 3).
| Intervention | Intervention | Control | P-Value |
|---|---|---|---|
| Pre- ECT | |||
| Preliminary preparation | 8.91 ± 0.282 | 6.61 ± 1.32 | 0.0001 a |
| Routine preparation | 7.79 ± 0.414 | 7.80 ± 0.401 | 0.889 |
| Preparation of equipment | 52.85 ± 1.66 | 51.38 ± 2.77 | 0.052 |
| Immediately before shifting the patient to ECT room | 5 ± 0.0001 | 5 ± 0.0001 | 0.99 |
| On ECT table | 4 ± 0.0001 | 4 ± 0.0001 | 0.99 |
| During ECT | 10.04 ± 0.204 | 9.69 ± 0.788 | 0.06 a |
| Post-ECT | 9.87 ± 0.337 | 8.76 ± 1.041 | 0.001 a |
| Checking the patient’s status | 9.95 ± 0.204 | 9.730 ± 0.452 | 0.030 a |
aP < 0.05 indicated a significant difference.
5. Discussion
This study aimed to determine the effect of simulation-based skill training on improving the quality of ECT care in nurses working in the psychiatric wards of two university hospitals in Ahvaz, Iran. The findings showed that the mean scores obtained in pre-test and post-test in the intervention group in the preliminary preparation, during ECT, post-ECT, and checking the patient’s status were significantly different (P < 0.05). This suggests that simulation intervention in small groups was effective in improving the quality of ECT care. These results are consistent with the findings of Rabheru et al. and Raysin et al. (12, 23). However, in the study conducted by Raysin et al. (23), data collection instrument was a self-report questionnaire with lower reliability compared to the present study; they also performed data collection using a checklist and by an external evaluator. In addition, Raysin et al. (23) evaluated the quality of care in three areas of knowledge, relaxation, and capability. Another important difference between the present study and the study carried out by Rabheru et al. was related to the areas of study among the participants. They considered the subscales, including patient respect, efficiency, knowledge, communication, and overall performance, but we focused on the procedures and process of care from the beginning to the end of the procedure. Also, the present study attempted to address every single detail of the care process before, during, and after ECT, but Rabheru et al. generally evaluated cares during ECT (12).
Our results showed that simulation-based training led to the improvement of basic knowledge and technical skills of ECT in nurses. Considering much evidence regarding the use of ECT in the treatment of psychiatric disorders, as well as its inclusion as part of treatment guidelines for mentally ill people, this educational method should be included in clinical setting of all psychiatric nurses, and therefore be taught in medical educational programs (10, 24).
The results showed that simulation-based training helped to increase the level of comfort and self-confidence of assistants in performing ECT. Although the basic level of comfort was the same in both groups, those who received simulation-based training showed a higher level of comfort and confidence in ECT training. Also, nurses may show significant improvements in the actual elements related to clinical use of ECT due to the interactive nature of this training because simulation-based training creates a more realistic environment that improves both knowledge and technical skills (25, 26).
Ferrero et al. showed that simulation-based training significantly increased self-confidence, reduced anxiety, and corrected skill sets among participants (27). Assigning time to the trainee’s demands and providing an opportunity to answer the questions allow providing real-time feedback. Experimental learning through experience and correcting mistakes in real time during questioning optimize the clinical outcomes when caring for patients (28). Another point is that the usual method of teaching ECT care, which is training based on a lecture in a small learning group, is effective in promoting knowledge and self-confidence, but does not necessarily affect performing ECT skills independently. In contrast, the results of the group trained by simulation method were significantly better than the usual method of training in acquiring ECT skills. This is a considerably important finding that can have an important impact on the teaching process of ECT skills to nurses to improve the level of patient safety (12).
Simulation can also be used for rare and unplanned scenarios, and achieving critical skills that trainees may not normally be exposed to. Compared to the learning process that occurs during usual therapeutic care, simulation-based training can allow trainees to participate in difficult scenarios without fear of injuring patient or observer intervention (29). In the present study, it was expected that educating nurses to perform ECT on a simulated patient would give the trainees a greater sense of comfort, self-confidence, and awareness at the time of prescribing and administering the treatment. Implementing patient simulations for ECT training and evaluation can also be used in institutions for validating ECT nurses to rate performing ECT (30).
One of the limitations of this study was that it was conducted in two different hospitals and two groups (intervention and control), and the subjects may transfer their experiences to each other. Further studies in different centers are required to investigate the generalizability of findings.
5.1. Conclusions
Since ECT is a very effective and safe method when properly used by well-trained psychiatric nurses, it is necessary to provide an adequate in-service training for ECT nurses. Findings of the present study showed that strengthening ECT training to psychiatric nurses using simulation in small groups provides knowledge and technical learning that cannot be achieved easily through other methods. By implementing the proposed teaching method in this study, the nurses get a comprehensive experience not only in the basics of ECT theory but also in the implementation of this method. Also, they can practice their skills before performing them on a real patient.