1. Background
In the last few decades, progress and innovation in all branches of surgery, especially minimally invasive surgeries, have been very significant, and new technologies and techniques have replaced traditional methods in surgical procedures (1). Laparoscopy is a series of minimally invasive surgeries in which the surgeon performs surgical interventions through small incisions in the abdominal wall using long instruments. Reduced pain, less bleeding, and decreased hospitalization time are the advantages of laparoscopic surgery compared to open surgical procedures (2, 3). Researchers have discussed human errors and adverse events during surgery for many years. Technical and non-technical errors during surgery may cause adverse complications after surgery, but there is an agreement that these errors should be identified and prevented by education (4).
Although anatomical vision has improved in laparoscopic surgery, the risk of postoperative complications and patient mortality has increased due to technical errors during surgery. Untrained surgical assistants do not provide good vision for the surgeon and the surgical team, which increases the errors of the surgical team and consequently reduces the patient's safety (1). In laparoscopic surgery, there is no freedom of the hands, a direct touch of the viscera, and three-dimensional vision. In fact, laparoscopy requires understanding the depth and coordination of the hands and eyes while controlling the instrument for a long time in a particular position (5-7). During a standard laparoscopic procedure, the first assistant, who may be a first-year assistant or a surgical technologist, is usually less experienced. During the surgery, the assistant should perform skills such as surgical instruments to assist the surgeon, facilitate surgical interventions, and expose the surgical site with camera navigation (8, 9). Because the surgeon cannot guide the camera and perform the surgical procedure simultaneously, s/he assigns this task to the assistant, and somehow the surgeon's eyes are in the hands of another person (10, 11). The skills needed in laparoscopic surgery require hand-eye coordination, while in open access surgeries, this skill is not much important due to direct vision (12, 13). Therefore, the laparoscopic surgery team needs to be trained in a practical and simulated environment before working in the operating room. Learning should occur in practice, not at the patient's bedside, to reduce complications and technical errors. To improve learners' skills at different levels, we need to use new methods such as simulation so that learners can perform their tasks on patients with more confidence, making sure of no harm to patients (14, 15). Therefore, due to the rapid development of surgical technology, especially in minimally invasive surgeries, we need to use new training programs to align surgical technologists with new plans and tasks (14).
In the late 1990s, the American Society of Gastroenterological Endoscopic Surgeons published the fundamentals of laparoscopic surgery Program. This program includes two components: Theoretical knowledge and practical skills. This standard training program aims to achieve a set of theoretical and practical knowledge for learners and trainees of laparoscopic surgery that can bring them to a safe level of knowledge and skills to provide laparoscopic care (16). In this program, a simulation environment is suggested to train skills and surgical techniques. Studies have shown that training-simulated laparoscopic skills improve people's skills in the operating room. Today, laparoscopic skills training is often performed in a minimally invasive surgical simulation environment. Various techniques are used through a training box or virtual reality simulator in this pervasive environment without harming the patient. This new training method increases skills and improves adaptation to specific ergonomic challenges during surgery (17-19). In a 2016 study by Torricelli et al., which assessed the effect of laparoscopic surgery training in a simulation environment on surgeons' skills in the operating room, the training in the simulation environment improved skills (20). Numerous studies have shown that teaching laparoscopic surgery knowledge and skills according to the fundamentals of laparoscopic surgery Program can improve surgical assistants' and trainees' knowledge, skills, confidence and significantly promote their skills in the operating room (20-22).
In many operating rooms, surgical technologists as assistant surgeons in the laparoscopic surgical team are responsible for camera navigation and peg transfer, so it is essential to teach them these skills when they are students.
2. Objectives
This study aimed to investigate the effect of the fundamentals of laparoscopic surgery curriculum on the competence of surgical technology students in performing camera navigation, pattern cutting, and peg transfer.
3. Methods
This interventional study was designed and conducted with the ethics code IR.IUMS.REC1396.9511101009 at the Iran University of Medical Sciences in 2018. The study population included all eighth-semester undergraduate operating room students (n = 30) who were doing internships in the field. A census method was used for sampling.
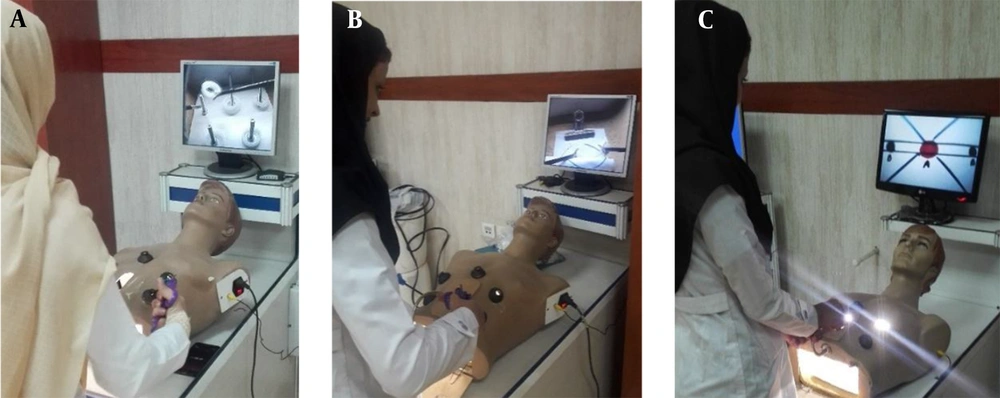
Inclusion criteria were students' willingness to participate in the study and setting up a gastrointestinal surgery technology course. The study was designed and conducted based on Kern's six-step model: Needs assessment, targeted needs assessment, goals and objectives, educational strategies, implementation, and evaluation. A needs assessment was performed based on a survey according to the surgical technologist's job description form. A list of items was prepared based on the operating room staff's job descriptions required before, during, and after surgery. Then, based on agreements and scores, the items were selected for educational purposes. After assessing the needs of different groups of operating room experts and surgeons, the educational objectives were determined in a specialized panel in the presence of experts in this field. Then, based on a review of studies and opinions of university faculty members, the educational content (triple skills required for surgical assistants in the FLS curriculum) to achieve the goals was determined. For determining the educational strategy and teaching method, training by demonstrating and practicing practical skills on training boxes for laparoscopic surgery was selected and performed in a simulated training environment (Figure 1A, B, and C). In the evaluation phase, as a final step in curriculum development, students were qualified to acquire three skills: Camera navigation, cutting a circular pattern, and peg transfer, as the basic skills in laparoscopic surgery using the task completion time (TCT) checklist and standard criteria.
(A) Training and assessing triple laparoscopic surgery skills in the minimally invasive surgeries research center at Rasoul Akram Hospital, peg transfer skill; (B) Training and assessing triple laparoscopic surgery skills in the minimally invasive surgeries research center at Rasoul Akram Hospital, pattern cutting skill; (C) Training and assessing triple laparoscopic surgery skills in the minimally invasive surgeries research center at Rasoul Akram Hospital, camera navigation skill.
Thus, after coordinating and reserving the minimally invasive surgery research center, the students were divided into three groups. Each group consisted of 10 students. A single day was allocated for training and practicing the practical skills of each group in the center. Camera navigation, pattern cutting, and peg transfer skills were taught according to the fundamentals of laparoscopic surgery curriculum by two faculty members of the operating room. The first attempt to perform each skill was recorded as the pretest, and the skill assessment results after six and 10 repetitions were considered the posttest scores. This criterion was recorded to measure the ability of individuals performing different laparoscopic skills in the simulation environment based on the amount of time in seconds. The TCT score included recording the time from the start of the skill to its completion. Mishra designed and validated this criterion in 2008 to evaluate laparoscopic skills in a simulation environment (23). In this criterion, the TCT score is calculated by controlling the number of errors and measuring the time required to perform each skill. The TCT score was calculated and recorded for each skill for the first time (pretest), the sixth time, and the 10th time (posttest). An ideal score is defined for the three skills in the fundamentals of laparoscopic surgery Program. This score refers to the standard time for completing each skill. The ideal score is 60 s for camera navigation, 48 s for peg transfer, and 98 s for pattern cutting (24).
Analysis of variance with duplicate data was used to compare operating room technology students in triple skills. A t-test with Bonferroni correction was used between different times for each skill to make comparisons. Data were analyzed using R statistical software.
4. Results
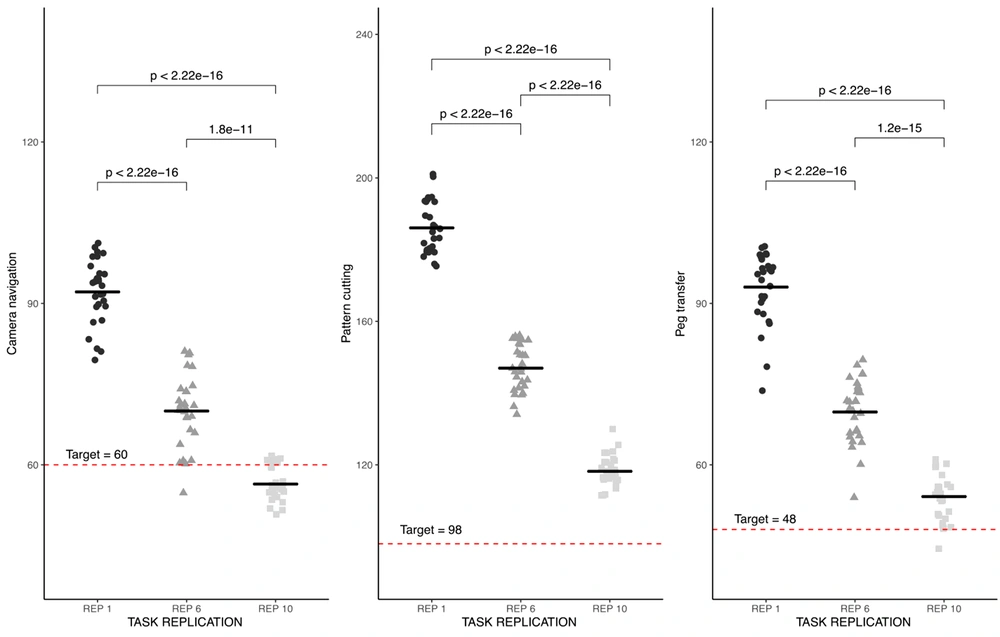
Out of 30 students participating in this study, 68% (n = 20) were women with a mean age of 25.3 ± 23.05, and 32% (n = 10) were men with a mean age of 22.67 + 1 years. Figure 2 shows the acquired scores of students in three skills of camera navigation, pattern cutting, and peg transfer in the first, sixth, and 10th repetitions of each skill. In this figure, the horizontal line in each repetition represents the average score of the participants in that repetition for each skill. For example, the average camera navigation skill for people in the first iteration was a little over 90 s. The average was reduced to approximately 70 s in the sixth iteration, and less than 60 s in the 10th iteration. In this diagram, the dashed horizontal line shows the desired score level for each skill. For example, the optimal score is 60 s for camera navigation, 98 s for pattern cutting, and 48 s for peg transfer. Figure 2 shows that although the time to perform the skill was significantly reduced from the first repetition onwards (the time difference between all time points was statistically significant at P < 0.001), individuals' average camera navigation performance reached the desired score level only in the 10th repetition. It seems that more repetition was needed to cut the pattern and move the pieces because, after the 10th repetition, the participants' performance was still far from the desired level.
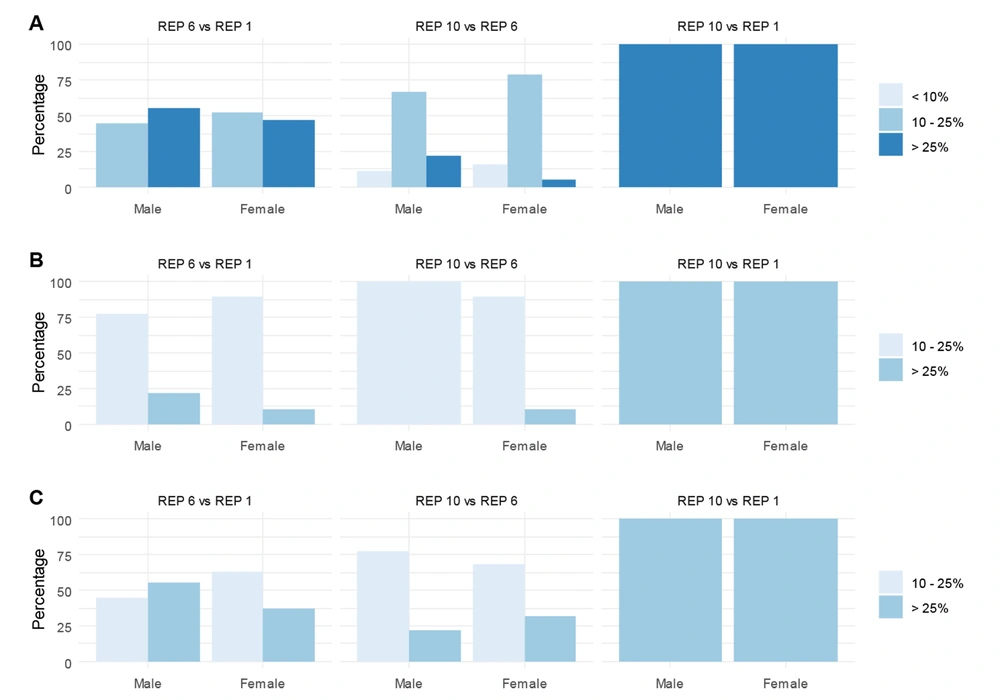
As Figure 3 shows, individuals' performance improved over time and with the repetition of skill performance. Given that this rate of performance improvement was less than 10%, 10 - 25%, or more than 25%, they were calculated separately for men and women in Figure 3.
In Figure 3, a comparison of camera navigation performance (panel A) shows that the performance improved more than 25% in both men and women in the 10th repetition compared to the beginning of the study and between 10 and 25% compared to the sixth repetition. Comparison of individuals' performance in pattern cutting (panel B) and peg transfer (panel C) showed at least 10% of individuals' functional changes. Also, in the 10th repetition compared to the start of the study, none of the subjects improved more than 25%. In the 10th repetition, all subjects (men and women) performed the same in the three skills compared to the beginning of the study, so that 100% of the subjects showed a performance improvement of more than 25% in camera navigation and 10 - 25% improvement in the other two skills.
Figures 2 and 3 show that the average time required for students to perform each skill in the first, sixth, and 10th repetitions gradually decreased, indicating an improvement in students' skill level by the end of the study. According to the reproducibility structure of skills, the analysis of variance was used for repetitive data to compare the average time of skills at different repetitions, as shown in Table 1.
| Skill | Repetition | F(2/26) (MANOVA) | Sex | Age | Time * Sex |
|---|---|---|---|---|---|
| Camera navigation | < 0.001 | 628.47 | 0.863 | 0.876 | 0.533 |
| Pattern cutting | < 0.001 | 1864.88 | 0.833 | 0.180 | 0.673 |
| Peg transfer | < 0.001 | 573.12 | 0.635 | 0.995 | 0.914 |
Results of Analysis of Variance for Duplicate Data. Numbers Represent the P Value of Each Factor
Table 1 shows that the only factor that affected participants' performance improvement was the time (or skill repetition). Age and gender did not significantly affect the rate of performance improvement and their interaction.
5. Discussion
The study showed that after practicing laparoscopic skills in the training box, the skill performance quality of novices without any previous experience in laparoscopic surgery improved with a gentle slope. Of course, other studies should consider the quality of skills performed in the operating room by people trained in the simulation environment with the training box. In a study by Kunert et al. they concluded that the administration of simulated training of skills in a safe environment would accelerate the learning process and give people a better understanding of three-dimensional space (25, 26). According to the study results, by practicing and performing skills repeatedly in the simulation environment, the accuracy and speed of students in doing skills increased gradually. For example, the time required to perform the first part of the practice to accomplish the skill of peg transfer was 93 s, which was reduced to 54 s in the 10th repetition. In line with the present study results, a 2011 study by Vitish-Sharma et al. that compared simulation training with a training box and a virtual reality simulator also showed that simulation training with both methods helped acquire psychomotor skills. According to Vitish-Sharma et al.'s study, in simulation training, due to a safe environment and the lack of concern for injury to the patient, learning time was reduced, the focus of surgical trainees on basic knowledge was increased, and their skills were improved (27).
In this regard, a study conducted by Alam et al. in 2017 to design and evaluate a tool to improve camera navigation skills showed that the average time required for camera navigation skills and related errors such as central errors, horizontal errors, and maintaining distance from the center were significantly reduced after training (28). Also, Nilsson et al., in 2017, conducted a study aimed at teaching camera navigation and transferring skills to operating room students, which showed that the simulated training of camera navigation helped operating room students overcome unfamiliar environments and better focus on the duties of a surgical assistant in laparoscopic surgery. Also, in this study, students gained higher skills by increasing practice and repetition of camera navigation skills, and their errors were reduced (29), which is in line with the present study results.
According to a 2008 study by Mishra, the ability to work in a three-dimensional environment by viewing a two-dimensional image on a screen was the most basic requirement for performing basic laparoscopic techniques (23). In this regard, he conducted a study to design a tool to assess laparoscopic skills. The results confirmed the effect of repetition and practice of skills in the training box on improving people's two-dimensional and three-dimensional perception in laparoscopic surgery. In all participants, the time of performing the skill for the 10th time was significantly reduced compared to the beginning, indicating an increase in the participants' abilities during the study (23). Consistent with the results of Mishra's study, in the present study, surgical technologists also advanced in performing triple skills in laparoscopic surgery. Comparison of the results in the first, sixth, and 10th repetitions of each skill showed that with practice and repetition, students could overcome the ergonomic challenges of the laparoscopic workspace and perform these skills faster with fewer errors.
5.1. Limitation
The small number of samples in this study is one of its limitations that could affect the generalizability of the results. One of the strengths of this study is the use of a laparoscopic surgical curriculum, which was used for surgical residents before this study.
5.2. Conclusions
The study showed that the application of the fundamentals of laparoscopic surgery curriculum in the academic course of surgical technologists improved the competence of surgical technology students in performing camera navigation, pattern cutting, and peg transfer skills, as the basic skills in laparoscopic surgeries whose learning plays a vital role in the successful performance of laparoscopic procedure and increases the safety of patients. Therefore, implementing this program in the educational program of surgical technology students is recommended.