1. Background
Clinical education is a vital component of physician education and training, where medical students learn by attending to patients and applying their knowledge and reasoning to solve their problems. This process helps students develop professional competencies to deliver safe and optimal patient care (1, 2). However, studies have shown that many medical students in the country’s universities struggle to acquire procedural skills, which are the ultimate goal of clinical education (3, 4). Therefore, it is important to identify and address the factors affecting clinical education's quality and effectiveness (5, 6).
Pediatrics is a specialized field that requires residents to acquire various procedural skills and professional attitudes to provide better health services to children and families (7). The pediatrics residency program lasts three years and aims to enhance the residents’ capabilities, responsibility, and commitment. However, the current curriculum may not adequately prepare the residents for the practical field of pediatrics, as many variables influence their clinical training. To improve the situation, clinical educators must assess the program's strengths and weaknesses and incorporate the residents' feedback and opinions as an educational element (7).
Previous studies in different countries have reported that many pediatric residents do not achieve competence in essential procedural skills by the end of their training and face various challenges and barriers in their clinical education. These studies have also suggested ways to improve procedural skills training and assessment quality and effectiveness, such as standardizing the curriculum, providing feedback and supervision, using simulation-based training, and implementing more valid and reliable evaluation methods (8, 9).
This study evaluated the essential procedural skills acquired by pediatric residents in Mofid Children’s Hospital based on their self-report. Self-report is a useful method for collecting information about one’s learning and performance, as few people have a more honest and continuous view of oneself than oneself (10).
2. Objectives
We also aimed to identify the strengths and weaknesses of the program and suggest ways to enhance the learning of procedural skills. We defined essential procedural skills as those expected to be learned by the residents according to their academic year.
3. Methods
This descriptive cross-sectional study used a researcher-made questionnaire conducted from 2019 to 2020 at Mofid Children’s Hospital.
The sample consisted of 115 pediatric residents at Mofid Children’s Hospital, who were included in the study through convenience sampling. Inclusion criteria included all specialized pediatric residents of Mofid Children’s Hospital who had passed at least one semester of their entry into the internship. Residents unwilling to complete the questionnaire were excluded from the study.
Out of 120 Mofid Children's Hospital pediatric residents, 115 returned the questionnaires.
3.1. Research Tools
To formulate a researcher-made questionnaire, the first 33 essential procedural skills were extracted from an approved pediatric residency curriculum, and the number of times they were performed in three training methods (observation, performing with help, and independent performance) was recorded (Table 1).
| Skill Title | Observations Skills, N | Performing with Help, N | Performing Independently, N | Required Times, Total |
|---|---|---|---|---|
| Basic life support | 5 | 5 | 5 | 15 |
| Advanced life support | 2 | 3 | 5 | 10 |
| Advanced resuscitation methods | 2 | 3 | 5 | 10 |
| Insertion of different types of umbilical catheters | 2 | 2 | 4 | 8 |
| Arterial blood sampling | 2 | 3 | 10 | 15 |
| Umbilical vein blood sampling | 2 | 2 | 6 | 10 |
| Subcutaneous, intradermal, intramuscular, and intravenous injection | 3 | 3 | 24 | 30 |
| Inserting NG tube | 1 | - | 9 | 10 |
| Bladder aspiration | 2 | 2 | 6 | 10 |
| Treatment of interosseous | 1 | 1 | 1 | 3 |
| LP | 2 | 3 | 5 | 10 |
| Plural tap | 1 | 1 | 3 | 5 |
| Ascites tap | 1 | 1 | 3 | 5 |
| Bone marrow aspiration | 2 | 2 | 3 | 7 |
| Total blood exchange | 1 | 1 | 1 | 3 |
| Preparation of smear and gram staining and Giemsa | 2 | 2 | 8 | 12 |
| Microscopic urine analysis | 1 | - | 2 | 3 |
| Urinary tract catheterization | 2 | 2 | 6 | 10 |
| Bone marrow biopsy | 1 | 1 | - | 2 |
| Administration of surfactant through endotracheal tube | 2 | 3 | 5 | 10 |
| Electrocardiography | 1 | - | 4 | 5 |
| Peritoneal dialysis | 1 | 1 | 1 | 3 |
| Working with a ventilator | 3 | 2 | 15 | 20 |
| Core needle liver biopsy | 1 | 1 | 1 | 3 |
| Circumcision | 1 | 1 | 8 | 10 |
| Intravenous catheterization | 1 | 1 | 8 | 10 |
| Chest tube insertion | 1 | 1 | 2 | 4 |
| Peripheral, central optimal catheter | 5 | 5 | 5 | 15 |
| Working with the supraglottic device | 5 | 5 | 5 | 15 |
| Insulin injection and work with glucometer | 1 | 1 | 8 | 10 |
| How to use and learn how to use asthma spacer | 1 | 1 | 8 | 10 |
| Clinical skills of vaccination | 3 | 3 | 10 | 16 |
| Clinical skills in performing PPD | 1 | 1 | 10 | 12 |
Abbreviations: LP, lumbar puncture; PPD, purified protein derivative.
Before using the questionnaire, the content was reviewed in a meeting attended by (4 experts) to validate its content and match it with the opinions of experts. After exerting the experts' opinions, the experts again confirmed the modified questionnaire. The reliability of the questionnaire was examined by calculating Cronbach’s alpha, which was equal to 80%.
In addition to the demographic information, the mentioned questionnaire consists of two parts (Appendix 1 in Supplementary). The first part evaluates the number of residents faced with 33 essential procedural skills of the curriculum approved by the Ministry of Health and Medical Education in the three areas (observation, performing with help, and independent performance) from the view of pediatric residents. The second part is assigned to the self-evaluated pediatric residents in learning the 33 skills based on the 5-point Likert scale (very poor to excellent).
The content validity of the questionnaire was determined by reviewing the literature and consulting with four experts in pediatrics and medical education. The experts’ opinions were used to modify and confirm the questionnaire. The reliability of the questionnaire was estimated by calculating Cronbach’s alpha coefficient, which was equal to 0.80.
Descriptive statistics such as frequency, percentage, mean, and standard deviation were used to describe the data. The data was analyzed by Friedman's comparison test and Spearman's coefficient. Finally, a P-value less than 0.05 was considered statistically significant. All analyses were performed by statistical software SPSS 24.0.
This study was approved by the Ethics Committee of the Virtual School of Medical Education and Management, Shahid Beheshti University of Medical Sciences, Tehran, Iran, with the approval number of IR.SBMU.SME.REC.1398.045. The study details were explained to all participants, and their information was kept confidential.
4. Results
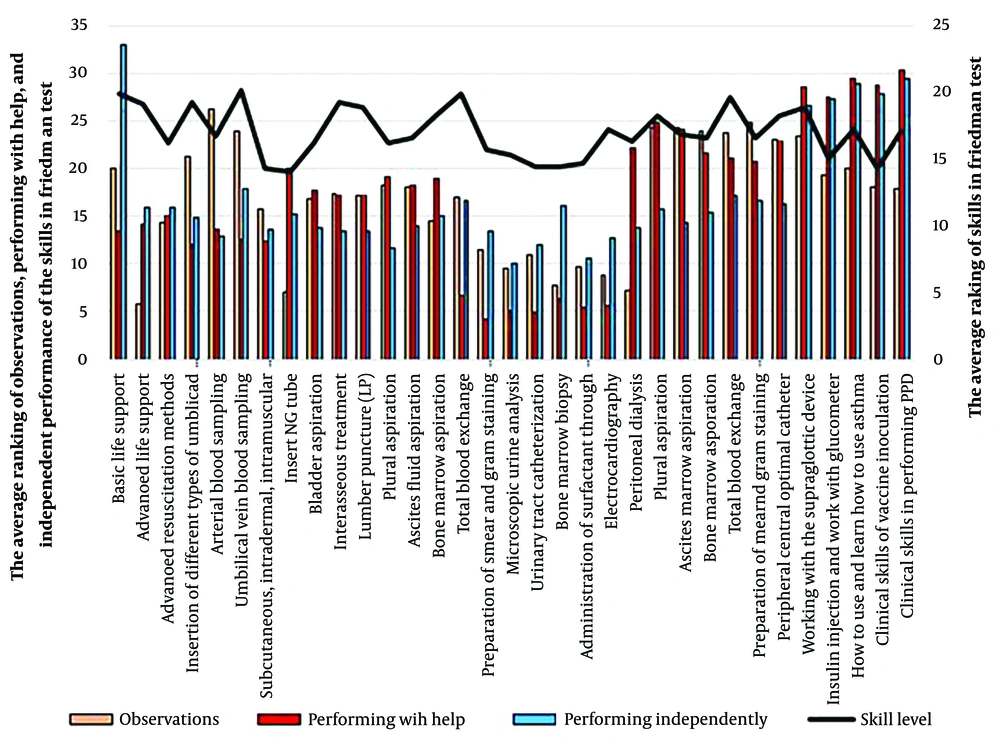
Since completing the questionnaire voluntarily, 115 questionnaires were fully completed and analyzed. In total, 42% of the male and 58% of the female residents with a mean age of 32 participated in this study. To evaluate the training state, first, the statistical characteristics of the skills were obtained from the view of observation, performing with help and independent performance, and then ranked with the Friedman comparison test (P-value < 0.001). The results showed that the number of pediatric residents exposed to arterial blood sampling skills by observation method had the highest ranking with an average of 14 times, and skills of advanced resuscitation methods by observation method had the lowest ranking with an average of six times. In terms of performing with the help of each skill, the number of encounters with procedural skills purified protein derivative (PPD) with an average of 17 times had the highest ranking, and the number of encounters with the skill of preparation of smear and gram staining and Giemsa with an average of eight times had the lowest ranking. Independent performance of airway intubation skills, with an average of 18, had the highest ranking, and independent performance of microscopic urine analysis test, with an average of nine, had the lowest ranking compared to other skills regarding the number of encounters (Figure 1).
The average participant's performance of all skills in all three methods of observation, performing with help, and independent performance complied with the standards approved by the Ministry of Health and Medical Education, except for the independent performance of subcutaneous, intramuscular, and intravenous injection skills (in standards it’s estimated to be 24 times and 10 times on average in the evaluation of this research) and skills of working with a ventilator (in standards it’s calculated to be 15 times and 10 times on average in this study). This shows the special need for revising the pediatrics residency curriculum for more exposure and independent performance of the essential procedures according to approved standards (Table 2).
| Item | The Mean of Independent Performance | The Means of Performing with Help | The Mean of Observations |
|---|---|---|---|
| Number of independent performing of basic life support | 17.88 | 11.92 | 11.35 |
| Number of independent performing of advanced life support | 10.08 | 12.19 | 10.11 |
| Number of independent performing of Advanced resuscitation methods | 10 | 12.35 | 6.73 |
| Number of independent performing of insertion of different types of umbilical catheters | 9.92 | 11.46 | 11.84 |
| Number of independent performing of arterial blood sampling | 9.5 | 11.88 | 14 |
| Number of independent performing of umbilical vein blood sampling | 10.46 | 11.65 | 12.46 |
| Number of independent performing of subcutaneous, intradermal, intramuscular, and intravenous injection | 9.61 | 11.53 | 10.03 |
| Number of independent NG tube insertion | 9.88 | 13.46 | 7.26 |
| Number of independent bladder aspirations | 9.61 | 12.96 | 10.23 |
| Number of independent performing of treatment of interosseous | 9.61 | 12.76 | 10.5 |
| Number of independent performing of LP | 9.65 | 12.92 | 10.46 |
| Number of independent performing of Plural tap | 9.38 | 13.38 | 10.65 |
| Number of independent performing of ascites tap | 9.69 | 13.19 | 10.84 |
| Number of independent performing of bone marrow aspiration | 9.84 | 13.46 | 9.61 |
| Number of independent performing of total blood exchange | 10.34 | 8.84 | 10.38 |
| Number of independent performing of preparation of smear and gram staining and Giemsa | 9.73 | 8.26 | 8.84 |
| Number of independent performing of microscopic urine analysis | 9.03 | 8.5 | 8.19 |
| Number of independent performing of urinary tract catheterization | 9.26 | 8.23 | 8.65 |
| Number of independent performing of bone marrow biopsies | 10.26 | 8.42 | 7.69 |
| Number of independent performs of administration of surfactant through endotracheal tube | 9.07 | 8.5 | 8.34 |
| Number of independent performing of electrocardiography | 9.42 | 8.34 | 8 |
| Peritoneal dialysis | 9.73 | 14.30 | 7.5 |
| Number of independent performing of working with a ventilator | 10 | 15.11 | 12.46 |
| Number of independent performing of core needle liver biopsy | 9.76 | 15 | 12.5 |
| Number of independent performing of circumcision | 9.84 | 14.11 | 12.38 |
| Number of independent performing of Intravenous catheterization | 10.23 | 14 | 12.30 |
| Number of independent performing of chest tube insertion | 10.15 | 13.80 | 12.73 |
| Number of independent performing of the peripheral, central optimal catheter | 10.15 | 14.53 | 12.23 |
| Number of independent performing of working with the supraglottic device | 12.61 | 16.73 | 12.19 |
| Number of independent insulin injections and work with a glucometer | 12.96 | 16.57 | 11.23 |
| Number of independent using and learning how to use asthma spacer | 13.26 | 16.96 | 11.26 |
| Number of independent performing of clinical skills of vaccination | 12.88 | 16.46 | 10.80 |
| Number of independent performing of clinical skills in performing PPD | 13.80 | 17.26 | 10.76 |
Abbreviations: LP, lumbar puncture; PPD, purified protein derivative.
In the second part of the questionnaire, to assess the current state of the skills acquired by the residents, first, the statistical characteristics obtained from the self-evaluated score, each skill was calculated for each resident based on a 5-point Likert scale (from very poor to excellent). Then, the Friedman test (P-value < 0.045) was used to compare skills and identify strengths and weaknesses. The results obtained from the skills ranking indicated that the residents rated the skills of arterial blood sampling, total blood exchange, and basic life support as the highest and rated the skill of inserting an NG tube, procedural skills of vaccination, and subcutaneous, intradermal, intramuscular, and intravenous catheterization as the lowest (Figure 1).
Spearman coefficient was used to examine the degree of dependence of each skill and the type of training in terms of observation, performing with help, and independent performance. The results of this analysis in all skills indicated that the skill level has a significant correlation with independent performance, and observation and performing with help had less effect on the rate of skill performance. Therefore, it is important to pay attention to the independent performance of skills in the residency curriculum (Table 3).
| Item | Correlation with the Number of Observations | Correlation with the Number of Performing with Help | Correlation with the Number of Independent Performances | |||
|---|---|---|---|---|---|---|
| Correlation Coefficient | P-Value | Correlation Coefficient | P-Value | Correlation Coefficient | P-Value | |
| Basic life support | -0.056 | 0.784 | 0.335 | 0.094 | 0.671 | < 0.001 |
| Advanced life support | 0.108 | 0.6 | 0.175 | 0.394 | 0.551 | 0.004 |
| Advanced resuscitation methods | -0.264 | 0.193 | 0.128 | 0.532 | 0.58 | 0.002 |
| Insertion of different types of umbilical catheters | 0.388 | 0.05 | 0.174 | 0.395 | 0.597 | 0.001 |
| Arterial blood sampling | -0.026 | 0.9 | -0.058 | 0.782 | 0.497 | 0.01 |
| Umbilical vein blood sampling | 0.044 | 0.831 | 0.068 | 0.74 | 0.323 | 0.049 |
| Subcutaneous, intradermal, intramuscular, and intravenous injection | 0.489 | 0.011 | 0.035 | 0.865 | 0.652 | < 0.001 |
| Insert NG tube | -0.242 | 0.233 | 0.15 | 0.465 | 0.442 | 0.024 |
| Bladder aspiration | -0.342 | 0.088 | 0.261 | 0.198 | 0.85 | < 0.001 |
| Treatment of interosseous | 0.3 | 0.136 | 0.395 | 0.046 | 0.784 | < 0.001 |
| LP | 0.146 | 0.477 | 0.531 | 0.005 | 0.671 | 0.001 |
| Plural tap | -0.035 | 0.866 | 0.521 | 0.006 | 0.807 | < 0.001 |
| Ascites tap | -0.108 | 0.6 | 0.013 | 0.942 | 0.788 | < 0.001 |
| Bone marrow aspiration | 0.211 | 0.3 | 0.38 | 0.056 | 0.711 | < 0.001 |
| Total blood exchange | 0.338 | 0.091 | 0.015 | 0.941 | 0.583 | 0.002 |
| Preparation of smear and gram staining and Giemsa | 0.007 | 0.971 | 0.142 | 0.489 | 0.687 | < 0.001 |
| Microscopic urine analysis | 0.068 | 0.74 | 0.029 | 0.889 | 0.857 | < 0.001 |
| Urinary tract catheterization | 0.3 | 0.137 | 0.297 | 0.14 | 0.89 | < 0.001 |
| Bone marrow biopsy | 0.323 | 0.108 | 0.135 | 0.511 | 0.895 | < 0.001 |
| Administration of surfactant through endotracheal tube | 0.061 | 0.767 | 0.107 | 0.603 | 0.76 | < 0.001 |
| Electrocardiography | 0.07 | 0.735 | 0.371 | 0.062 | 0.806 | < 0.001 |
| Peritoneal dialysis | 0.088 | 0.67 | 0.149 | 0.466 | 0.742 | < 0.001 |
| Working with a ventilator | -0.115 | 0.576 | 0.216 | 0.288 | 0.886 | < 0.001 |
| Core needle liver biopsy | 0.401 | 0.042 | 0.175 | 0.393 | 0.695 | < 0.001 |
| Circumcision | -0.115 | 0.576 | 0.339 | 0.045 | 0.892 | < 0.001 |
| Intravenous catheterization | 0.044 | 0.831 | 0.178 | 0.384 | 0.857 | < 0.001 |
| Chest tube insertion | 0.239 | 0.24 | 0.495 | 0.01 | 0.809 | < 0.001 |
| Peripheral, central optimal catheter | 0.191 | 0.35 | 0.571 | 0.002 | 0.873 | < 0.001 |
| Working with the supraglottic device | -0.069 | 0.737 | 0.162 | 0.429 | 0.66 | < 0.001 |
| Insulin injection and working with a glucometer | 0.174 | 0.394 | 0.454 | 0.02 | 0.885 | < 0.001 |
| How to use and learn how to use asthma spacer | 0.01 | 0.962 | 0.345 | 0.084 | 0.754 | < 0.001 |
| Clinical vaccination skills | 0.025 | 0.952 | 0.343 | 0.086 | 0.827 | < 0.001 |
| Clinical skills in performing PPD | 0.186 | 0.363 | 0.018 | 0.93 | 0.876 | < 0.001 |
Abbreviations: LP, lumbar puncture; PPD, purified protein derivative.
5. Discussion
This study aimed to evaluate the essential procedural skills acquired by pediatric residents in Mofid Children’s Hospital and identify the factors affecting their clinical education. Procedural skills are important for pediatricians who enter the practical field after completing their residency program and strive to reduce suffering and ensure a child's health.
In the present study, based on the results obtained from the first part of the questionnaire, the average performance of each procedure was compared with the numbers approved in the pediatrics residency curriculum. The average performance of all skills from all three methods of observation, performing with help and independent performance, matched with the approved standards, except for independent subcutaneous, intramuscular, and intravenous injection skills (in the program, it’s estimated to be 24 times and the average performance in the evaluation of this research it was 10) and the skill of working with a ventilator (15 times in the program and the average of 10 times in this study). This finding is consistent with a previous study that indicated that the level of students’ confrontation with and performing those procedures directly influences their skills (11). Moreover, some studies reported that the desired standards are not totally observed in clinical training centers and that the procedural skills standard had the lowest score (12, 13).
In the second part of the questionnaire, according to the self-evaluation of the pediatric residents about the level of their skills in performing the essential procedures in curriculum, obtaining the lowest rank in inserting NG tube, and procedural skills of vaccination and subcutaneous, intradermal, intramuscular and intravenous injection. Because the skill of subcutaneous, intradermal, and intramuscular injection had the lowest average number of independent performances.
This finding indicates that the existing clinical learning methods do not stimulate the intellectual development of the residents and that they only acquire a technician's ability (13). Furthermore, some studies indicated that many physicians feel unprepared to commence clinical work after completing their medical education and face serious problems in clinical practice (12, 14, 15).
This study found that some essential procedural skills had lower exposure frequencies and independent performance than the approved standards, which may indicate residents’ insufficient experience and practice. We also found that the residents’ self-rated proficiency in performing these skills was low, which may reflect their lack of confidence and competence in clinical settings. These findings suggest a gap between the expected and actual outcomes of clinical education for pediatric residents.
Several factors may contribute to this gap, such as the availability and suitability of clinical conditions, the presence and supervision of instructors and professors, the level of stress and motivation of the residents, and the quality and quantity of feedback and evaluation. Previous studies have reported similar findings and challenges in clinical education for medical students and residents (16-19). They have also suggested some strategies to improve the situation, such as enhancing interaction and collaboration with the learners, promoting self-directed learning, providing more opportunities for practice and reflection, and creating an effective learning environment (18, 19).
Therefore, based on the results of this study and a review of previous studies in this field, we recommend that the implementation of the essential procedural skills training program for pediatric residents should be reviewed and revised in terms of how and how often the procedures are performed. This would help increase the level of skills acquired by the residents in the procedures that are considered important for their professional development.
5.1. Conclusions
Based on the opinion of the residents in this study, the current pediatrics residency curriculum implemented in Mofid Children’s Hospital, Shahid Beheshti University of Medical Sciences, was generally useful and effective. However, they also mentioned some obstacles and limitations which need plans, solutions, and monitoring. Therefore, it seems imperative to review the implementation of the curriculum and implement effective measures, including providing more confrontation conditions for independent procedures.