1. Background
The coronavirus disease (COVID-19) pandemic continues to have devastating effects on health systems worldwide (1, 2). People have experienced severe impacts on various aspects of their lives, and healthcare workers have suffered indescribable levels of anxiety, stress, and depression (3, 4).
Bedside teaching, the core component of residency medical education (ME), evolved after the pandemic (5, 6). At the beginning of the outbreak, all residents in different specialties had to visit COVID-19 cases as the dominant case. In 2020, approximately 900 million undergraduate and postgraduate students were affected. Therefore, they were unable to interact with patients like before or receive feedback during direct supervision (7). This led to an inevitable crisis in ME. Shifting to virtual and simulation-based learning to compensate for defects in traditional clinical teaching could put the quality of ME in danger.
The Accreditation Council for Graduate Medical Education adopted new principles in 2020. Some researchers claimed that ME and its inspection would likely be very different at the end of 2020 (8). For instance, surgical specialties in educational training centers had to prioritize urgent operations and postpone the elective ones. They utilized virtual reality, online platforms, video conferences, and simulation workshops to overcome the problems. This might result in the lower experience and proficiency of surgery residents (3, 7, 9, 10).
COVID-19 also affected all components of emergency medicine (EM) residency training courses as the specialty in the frontline of fighting against the disease. It is verified that the increased workload, shift hours, and burnout after the pandemic disrupted many essential learning objectives in this field. This consequence led learners to lose their enthusiasm and motivation to acquire needed skills and knowledge (11, 12). A cross-sectional survey of seven EM residency programs examined the pandemic effects on the educational experiences of residents and confirmed the negative impact on residency education, wellness, and clinical rotations (3). In this regard, the Council of Residency Directors in Emergency Medicine Application Process Improvement Committee recommended some serious changes and adjustments in EM residency programs to reduce the pandemic impact (4, 13).
2. Objectives
By the start of the outbreak, we have faced a major challenge in dealing with COVID-19 outcomes in Iran. Few studies have estimated its sequel on residency training courses in our country. Consequently, we conducted the present study to directly assess the perceptions of EM residents of their wellness and ME quality during the pandemic.
3. Methods
3.1. Study Design
This descriptive survey, conducted from November 2021 to February 2022, used a questionnaire developed by researchers to understand EM residents' perception of COVID-19's impacts on their ME and wellness. We obtained written consent from participants prior to the study. The study was approved by the Ethics Committee of Tehran University of Medical Science (TUMS) (IR.TUMS.MEDICINE.REC.1400.1071).
3.2. Participants and Setting
The current study was conducted in three educational hospitals affiliated with TUMS. All hospitals have been admitting COVID-19 cases since the first outbreak. The enrolled subjects were all residents (PGY1, PGY2, and PGY3) being trained from 2021 to 2022 and all who had graduated as EM residents during the past 2 years: 2019 and 2020.
Emergency medicine residency program in TUMS mainly consists of (1) bed-side emergency department (ED) clinical teaching, (2) clinical teaching in forms of other rotations outside the ED, (3) theoretical classes, including case presentations, lectures, morning reports, morbidity and mortality reports, journal clubs, as well as book and board reviews, and (4) practical classes, such as simulation and procedural workshops. During the pandemic, almost all theoretical classes were conducted virtually via online and university platforms. Some workshops and rotations were canceled due to COVID-19 precautions. Minimum requirement workshops were held with the least attendants due to social distancing. Such limitations made us design and implement innovative courses, such as gamification and game-based learning, in new training environments outside the ED (14).
3.3. Questionnaire Contents and Validation
The questionnaire was designed in Persian (the items were translated into English for this manuscript) and began with a section about residents’ baseline and demographic data. Next, in the following areas, questions about COVID-19 involvement and concerns were asked (items are presented in Tables 1 and 2).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 25 (35.2) |
| Female | 46 (64.8) |
| Marital status | |
| Married | 51 (71.8) |
| Single | 20 (28.2) |
| Residency entrance year | |
| 2017 | 20 (28.2) |
| 2018 | 14 (19.7) |
| 2019 | 20 (28.2) |
| 2020 | 10 (14.1) |
| 2021 | 7 (9.9) |
| Hospital | |
| Imam Khomeini | 33 (46.5) |
| Sina | 17 (23.9) |
| Shariati | 21 (29.6) |
| Past medical history (diabetes mellitus, hypertension, hyperlipidemia) | |
| Yes | 7 (9.9) |
| No | 64 (90.1) |
| Working as a general practitioner before residency | |
| Yes | 60 (84.5) |
| No | 11 (15.5) |
| Variables | No. (%) |
|---|---|
| Previous history of COVID-19 infection | |
| Yes, outpatient | 53 (74.7) |
| Yes, hospital ward admission | 5 (7.0) |
| Yes, intensive care unit admission | 0 (0.0) |
| None | 13 (18.3) |
| Concern about COVID-19 transmission to your family that made you change where you lived | |
| I live alone. So, I did not have such concern. | 13 (18.3) |
| I live with my family in spite of that concern. | 53 (73.2) |
| I live in the same place, but I asked my family to move to another place. | 2 (2.8) |
| I moved to another place. | 4 (5.6) |
| Concerns about COVID-19 (More than one choice could be chosen) | |
| I do not have any concerns because I believe it will not be severe if I get the infection. | 4 (5.6) |
| I have a lot of concerns because I believe it will be severe if I get the infection. | 29 (40.8) |
| I am worried about the possibility of infecting my family due to my job. | 64 (90.1) |
| Being on the frontline is causing me anxiety. | 7 (9.9) |
| I am concerned about the decrease in my income. | 2 (2.8) |
| I have concerns about the residency training. | 27 (38.0) |
| The increased pressure on my colleagues is causing me concern. | 17 (23.9) |
| Preferred learning method during COVID-19 infection (More than one choice could be chosen) | |
| Self-learning | 54 (76.1) |
| Online courses | 39 (54.9) |
| Web-based media and the internet | 16 (22.5) |
| Asking professors | 40 (56.3) |
We searched PubMed and Embase databases but found no validated questionnaire regarding the effect of COVID-19 on residency ME. Therefore, we extracted all relevant items from selected articles and designed a preliminary questionnaire (58 questions) with four domains (education, hospital experience, clinical experience, and wellness). Afterward, we presented the questionnaire to a committee of two EM clinical attendings and one EM resident for discussion and revision. After the edition, we shared the questionnaire with 12 experts to assess content and face validity. Experts were requested to comment on the readability of items for face validity, including the location, correct scaling, and grammatical structure (15). A three-point Likert scale assessed the content validity ratio for necessity: 1 = not necessary, 2 = useful but not necessary, and 3 = necessary. Each item needed more than a 62% ratio to be valid (16). The content validity index (CVI) was evaluated using a four-point Likert scale: 1 = not relevant, 2 = somewhat relevant, 3 = quite relevant, and 4 = very relevant. Each item needed an index of more than 70% to be valid (17). Finally, the questionnaire consisted of 33 questions (5, 5, 12, and 11 about hospital experience, clinical experience, education, and wellness, respectively), with one open-ended question at the end (items are presented in Table 3). The Likert scale was from 1 = totally disagree to 5 = totally agree. After removing items with a CVI less than 0.7, we found that the mean item-level CVIs (S-CVI/Ave) for relevancy, clarity, and simplicity were 0.924, 0.975, and 0.979, respectively. The mean CVR for all 33 items was 0.828. In addition, the Cronbach's alpha coefficient was estimated to be 0.708.
| Variables | Mean ± SD | Median (IQR) |
|---|---|---|
| Hospital experience | ||
| I understand my responsibility in dealing with the COVID-19 disaster. | 3.1 ± 1.1 | 3 (2 - 3) |
| The updated COVID-19 management protocols are given to me. | 2.9 ± 1.7 | 3 (2 - 3) |
| COVID-19 has created a positive insight into emergency medicine. | 3.8 ± 1.4 | 4 (3 - 4) |
| COVID-19 has changed our residency program, and some of our rotations have been omitted. | 4.6 ± 1.2 | 4 (4 - 5) |
| COVID-19 has disrupted routine clinical care in the hospital. | 3.7 ± 0.8 | 4 (4 - 5) |
| Clinical experience | ||
| My knowledge and experience of respiratory diseases have increased. | 3.3 ± 0.7 | 3 (3 - 4) |
| My critical care skills in elderly patients have improved. | 3.0 ± 0.9 | 3 (3 - 4) |
| The diversity of diseases has declined. | 3.4 ± 0.9 | 4 (4 - 5) |
| The acuity level of diseases has decreased. | 2.4 ± 0.8 | 3 (2 - 3) |
| The opportunity for bedside learning during shifts has declined. | 4.3 ± 1.0 | 4 (3 - 4) |
| Education | ||
| The residency training program has been affected. | 4.3 ± 0.7 | 4 (4 - 5) |
| Educational activities and events (such as morning reports and classes) have been affected. | 4.2 ± 0.8 | 4 (4 - 5) |
| COVID-19 has led to holding our educational activities and events (such as morning reports and classes) on online platforms. | 4.1 ± 0.8 | 4 (3 - 4) |
| Research activities have been affected. | 3.9 ± 1.0 | 3 (3 - 4) |
| During the pandemic, it is necessary to have a longer course of residency. | 2.3 ± 1.1 | 2 (1 - 2) |
| I have experienced learning independently. | 3.7 ± 0.9 | 3 (2 - 3) |
| I feel more comfortable and flexible with online learning. | 3.2 ± 1.0 | 3 (3 - 4) |
| Online learning has unpleasant effects on colleagues’ relationships. | 2.8 ± 1.2 | 3 (2 - 3) |
| Focusing on COVID-19 patients has reduced the quality of the main contents of our education. | 3.7 ± 0.9 | 4 (3 - 4) |
| The training about COVID-19 disease is sufficient. | 3.7 ± 0.9 | 3 (3 - 4) |
| The training about the use of personal protective equipment is sufficient. | 3.1 ± 0.8 | 3 (3 - 4) |
| I have had enough time to study during the pandemic. | 2.2 ± 0.6 | 2 (2 - 3) |
| Wellness | ||
| COVID-19 has had unpleasant effects on my mental health status. | 3.7 ± 1.2 | 4 (3 - 4) |
| I feel uncomfortable while wearing personal protective equipment during the pandemic. | 3.4 ± 1.1 | 4 (3 - 4) |
| I have concerns about the safety of my family and myself. | 4.1 ± 0.8 | 4 (4 - 5) |
| COVID-19 has unpleasant effects on my social activities. | 3.8 ± 1.6 | 3 (3 - 4) |
| I have anxiety about my job career in the future after the pandemic. | 2.5 ± 1.4 | 2 (2 - 3) |
| I feel safe against COVID-19 in my workplace. | 2.3 ± 0.3 | 2 (1 - 2) |
| I have stress about the pandemic. | 3.4 ± 1.0 | 3 (3 - 4) |
| I feel depressed and uncomfortable during the pandemic. | 3.6 ± 1.9 | 3 (3 - 4) |
| My physical activity has been changed after the pandemic. | 3.4 ± 1.8 | 4 (3 - 4) |
| My sleep habit has been changed after the pandemic. | 2.9 ± 1.2 | 3 (2 - 3) |
| I am worried about being in the frontline. | 2.6 ± 1.1 | 3 (2 - 3) |
3.4. Data Collection and Analysis
We used our faculty database to find the current and former EM residents at TUMS and invited them to participate in our study via email and phone message. We sent two reminder emails the following month to encourage survey completion. To ensure the survey's integrity, we designed the online survey platform to allow only one response per computer internet protocol address. Participants had four weeks to complete the survey, and we only included completed questionnaires in our analysis. Data were described as median with interquartile range (IQR), mean with standard deviation (SD), or number with percentage (%).
4. Results
We received 71 responses from 84 residents in the survey (response rate: 84%). The participants had a mean age of 36.4 ± 7.3 years, with 46 (64.8%) being female and 51 (71.8%) married. Most of the residents (90.1%) had negative past medical histories. Baseline and demographic data are shown in Table 1.
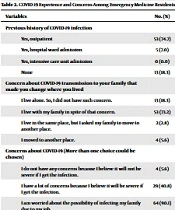
Fifty-eight out of 71 residents (81.7%) had a previous history of COVID-19 infection (mainly mild and outpatient). Most residents (n = 64, 90.1%) had concerns about transmitting the virus to their families, but 53 (73.2%) lived with their families despite the existing concern. The most preferred and popular learning methods were self-learning (n = 54, 76.1%) and asking professors (n = 40, 56.3%). Items related to COVID-19 experience and concerns are shown in Table 2.
In this survey, most residents agreed on the positive insight created by COVID-19 about EM. They also confirmed that COVID-19 changed their residency program and disrupted routine clinical care in hospitals. All these items in the category of “hospital experience” had a mean of >3 and a median of 4. As the “clinical experience” items showed, most residents agreed on the decrease in diversity and acuity of other diseases previously referred to the ED. They also referred to an increase in their knowledge and experience of respiratory diseases and critical care. They believed that these issues were responsible for a decline in bedside learning during shifts. All items had a mean of >3 and a median of 3 or 4. Most residents emphasized that COVID-19 had negative impacts on their residency training programs. This educational crisis made them learn independently and by themselves. They added that virtual learning and online programs were comfortable and flexible despite some unpleasant outcomes. All these items in the category of “education” had a mean of >3 and a median of 3 or 4. Most EM residents outlined that they had experienced anxiety and stress due to many concerns during the COVID-19 pandemic. They announced that their physical and social activities declined. Therefore, they were worried about their mental health and well-being. Enumerated “wellness” items revealed a mean of >3 and a median of 3 or 4. Data are shown in Table 3.
5. Discussion
In this survey, EM residents stated that the COVID-19 pandemic negatively affected their ME despite the better insight created about their specialty. The new educational atmosphere after the pandemic made residents learn independently and by themselves via virtual and online platforms. COVID-19 impacted all aspects of their residency training program. They suffered greater anxiety and stress during COVID-19 due to concerns about transmitting the viral disease to their families as well as changes in their physical and social activities.
5.1. Positive Impacts of the COVID-19 Pandemic on EM Education and Practice
Similar to any other disaster, COVID-19 could leave some constructive lessons and experiences behind. Across the world, ED staff faced challenges in obtaining adequate personal protective equipment (18), planning strategies for resource readiness and coping with the deficits (19), and protecting themselves and their own families and non-COVID-19 patients from catching the contagious viral disease. Struggling with the management plans and policies of such a disaster was regarded as a precious learning opportunity by our EM residents. This issue was also evident in previous studies (3, 4).
EM physicians were seriously affected by the COVID-19 pandemic. They had to effectively handle their overcrowded EDs and simultaneously provide the best care for COVID-19 and non-COVID-19 cases. They were the first physicians to intubate critical cases and directly expose themselves to a highly contagious disease. Despite the insufficient equipment and supplies, many of the EM residents in the present study were not worried about being in such a frontline position. Our study participants experienced a positive change in their perception of EM. Other studies confirmed this positive attitude towards the EM specialty after the pandemic (3, 4).
It has been indicated that EM physicians and residents gained more proficiency and competency in managing cases with acute respiratory failure in severe distress and providing them with the appropriate intensive care needed in the ED (3, 4, 9). This fact was also expressed by our residents.
An additional and beneficial outcome in the EM field occurred when modifications were inevitably made to the existing training programs. These modifications involved reducing the dependence on traditional in-person education and limiting the number of rotations outside the ED. As a result, a chance emerged for individuals to independently strengthen their knowledge, acquire skills in self-studying, and make the most effective use of online materials (9). A significant shift from traditional teaching to virtual and online education happened. In addition to online monologue lectures, numerous applications were described. These encompassed storytelling sessions, flipped classrooms, an archive of video-recorded patient interactions and surgeries, and virtual consultations integrated into telemedicine practices accompanied by discussions and in situ feedback (7, 9, 20, 21). Various methods were applied to the residency training program in our study to compensate for the resulting defects in traditional teaching after the pandemic. Some of these practices included making online and user-friendly materials (podcasts, narrating PowerPoints, and filming bed-side clinical procedures), elevating the quality and quantity of practical workshops in skill labs, using simulation, and gamification and game-based learning in a new and innovative environment outside the ED. Our residents found this new learning method more interesting, engaging, and comfortable (14).
5.2. Negative Impacts of the COVID-19 Pandemic on EM Education and Practice
A significant number of individuals we surveyed mentioned the considerable impact of COVID-19 on their mental health and well-being. As conveyed previously, the primary concern of EM residents was the risk of the potential transmission of COVID-19 to their families. Some studies proposed a strategy dividing residents into two groups: Actively present and remote (22). The suggested approach involved a two-week interval between rotations to ensure that residents were not infected.
Social distancing measures, spending less time with friends and families, and having fewer gatherings and social communication led to elevated levels of anxiety, stress, and depression among medical students and EM residents (3, 11, 23, 24). Our endpoints showed the same results.
In the field of ME, numerous challenges arose after decreasing non-COVID-19 cases, not only in delivering the required medical knowledge but also in training the necessary medical skills. For example, many disciplines had to halt elective procedures or surgeries and discontinue/omit some training rotations (3, 7, 13, 25). Our survey demonstrated these factors as an important concern for the EM residents.
Several studies focused on the abrupt switch to online learning and its disadvantages for residents as learners and educators (5, 7). Not all residents can highly benefit from online platforms and virtual classes (4, 9). Furthermore, they need to attain some digital skills and invest additional time in crafting electronic educational materials (5, 21). As a result, the literature reflects diverse feelings toward online learning (3, 5, 23). We drew the same conclusions from the present study.
5.3. Limitations
This study was performed in only one academic center (TUMS) and one specified residency program. Further analytical studies from different universities and specialties are recommended to comprehensively assess the exact impacts of the pandemic on different aspects of residents’ education and life.
5.4. Conclusions
Despite the positive perception of EM left behind (as a frontline specialty dealing with the most critical patients), the COVID-19 pandemic negatively influenced ME in the EM residency training program. Most previous bedside learning opportunities were lost, and residents had to improve their knowledge and skills through virtual and online platforms. The diversity and acuity of diseases other than COVID-19 decreased, leading to dissatisfaction among residents. Residents were exposed to greater anxiety and stress during the pandemic and were mostly worried about transmitting the disease to their families or being infected themselves.