1. Background
Games have been used to boost the desire to learn across several disciplines, including science, technology, engineering, and medicine (1-3). Game-based learning (GBL) and gamification have recently entered the realm of medical education (ME) and are now rapidly becoming a trend in professional ME (4, 5).
Traditional teaching methods primarily focus on instructor-based learning, where learners are expected to listen passively to the content provided by the teacher. This approach often results in less interactivity and engagement in the learning process (6). The application of game design elements to improve performance—such as learning attitudes, behaviors, and outcomes is referred to as “gamification” or “gamified learning” (7). Gamification introduces gaming principles into the learning process, making it fun, engaging, and even addictive (8). In contrast, GBL directly employs games to teach a specific skill or knowledge in a more motivating manner than traditional teaching (9). Both of these approaches fall under the umbrella of “active learning,” which aims to involve learners in an engaging way, emphasizing knowledge application over mere knowledge acquisition (10).
The literature recommends 12 key strategies to enhance the effectiveness of gamification in ME (11): (1) make learning fun and engaging, (2) evoke both intrinsic and extrinsic motivation, (3) incorporate progress mechanics, (4) use a narrative structure, (5) make learning experiential, (6) provide effective feedback to the player, (7) ensure sustainability, (8) utilize technology and devices, (9) emphasize repetition for learning reinforcement, (10) Incorporate competition to boost motivation, (11) focus on collaborative learning, and (12) integrate diverse player types.
Emergency medicine, with its wide range of essential skills and knowledge, is at the forefront of adopting GBL and gamification in ME. Most gamification projects in this field concentrate on specific content areas, single sessions, and frequently rely on computerized quiz-style or software-based games (12-19). A recent systematic review indicates that gamification can positively influence learning behaviors and attitudes in ME without adverse outcomes (20).
The use of medical podcasts dates back to the mid-2000s. Studies indicate that medical education through podcasts and other virtual materials has grown significantly in recent years (21). A primary critique of e-learning is the concern that non-medical professionals may misinterpret such information as medical advice. Additionally, despite its ease of access, e-learning is sometimes argued to potentially disrupt active learning among students.
In recent years, increasing patient admission rates at emergency departments (EDs), overcrowding, and various health crises such as the COVID-19 pandemic, which placed emergency physicians on the front lines have challenged every aspect of residency programs. Many traditional bedside learning opportunities have diminished in these overwhelmed settings. This unavoidable situation led us to transform challenges into opportunities, prompting the exploration of alternative learning environments outside the hospital. We integrated essential elements of both GBL and gamification into our EM training program, implementing these methods through a variety of game designs. Detailed information on the implementation phase (including game designs and review sessions) is available in our previous research (22). In this study, we focus on evaluating the impact of GBL and gamification in the EM residency program, comparing it with e-learning.
2. Objectives
We designed this research to evaluate the effects of GBL and gamification on residents’ learning within the EM educational program. Specifically, we compared the impact of GBL and gamification with that of podcasts and videos on residents’ knowledge, skills, clinical reasoning, and judgment.
3. Methods
This quasi-experimental study design included two distinct educational interventions compared across two groups of EM residents. We developed and implemented an innovative GBL and gamification course within the EM residency training program at Tehran University of Medical Sciences, starting in October 2022. Over 12 months, ten sessions covered all foundational, essential, and critical topics in the EM residency curriculum, including cardiology, respiratory, electrolyte imbalance and metabolism, orthopedics, toxicology, ventilator settings, airway management, hematology, suturing and immobilization, pediatrics, trauma, resuscitation, and life support.
During the implementation phase, our objective was to teach the requisite knowledge, procedural skills, clinical reasoning, and judgment for each residency level (PGY1, PGY2, and PGY3). We incorporated core elements of both GBL and gamification to create a learning environment characterized by enhanced interaction, competition, entertainment, encouragement, and motivation. To keep each session engaging and novel, we varied the game designs and frequently repeated sessions with the same content. Sessions were conducted through various methods and environments, including face-to-face classes or virtual classes via free university platforms, skill labs, and hospital settings.
A range of GBL and gamification formats—such as Dooz, Carts, Hot Seat, Escape Room, Escape Box, Taboo, Simulated emergency room, golden cup, control room, and matching cards—were used in both individual and group competitions. All game designs were adapted from the literature, and the implementation methods were reviewed by an expert panel comprising EM and ME faculty members. In each GBL and gamification session, residents tackled a clinical scenario, solving cases step-by-step. Each correct answer unlocked the next clue, guiding them toward the final solution. By the end of the session, all game components were pieced together like a completed puzzle, revealing the full scenario from the initial clinical presentation to the final disposition.
Each session included special awards or bonuses for the winner(s). Organized debriefing and problem-solving sessions were integral parts of the intervention (22). In this study, the course mentioned above served as the intervention for the first group of residents (Group 1).
For the second group, we created 10 medical podcasts and training videos covering the same topics and provided these materials to an equivalent number and level of residents via virtual platforms (group 2). All training podcasts were prepared and recorded by EM faculty members, featuring their voices and live videos alongside slides. Clinical features, diagnosis, management, and disposition of specific diseases and common medical cases were explained based on EM textbooks. Required procedures relevant to each case were also recorded at the bedside on actual patients as short videos (recorded live in the ED).
Both groups continued to participate in the traditional training program, which included attending lectures in theoretical classes, practicing procedures and practical skills in workshops, and engaging in active bedside learning during clinical shifts in the ED.
In the present study, we evaluated the GBL and gamification phase in the EM residency training program one year after its implementation in 2023. We enrolled 15 EM residents across three different levels (PGY1, PGY2, and PGY3) in each group. All residents at each level were randomly and evenly allocated to either group based on their residency ID number, with odd numbers assigned to group 1 and even numbers to group 2. Each group consisted of 7 PGY3 residents, 5 PGY2 residents, and 3 PGY1 residents. The sequence of interventions was implemented simultaneously in both groups.
We compared all outcomes between the GBL and gamification group (group 1) and the e-learning group (group 2). All EM residents participated in the same traditional residency training program at our university, covering the content and educational materials specified for each residency level. The themes of lectures in classrooms and workshops (for practicing EM procedures) were consistent across both groups. The sole interventions were the GBL and gamification courses conducted for the first group and the e-learning materials provided by EM professors to the second group.
All residents provided written consent to participate in this study willingly. The study was approved by the ethics committee of (anonymized for review) (ID: IR.TUMS.SHARIATI.REC.1402.059). In the EM residency training program, three general exams are administered twice a year (mid-year and at the end of the training year) to assess residents' knowledge and skills. These exams include a three-hour written exam with 150 multiple-choice questions (MCQs), a two-hour objective structured clinical examination (OSCE) consisting of 10 stations, where residents rotate through each station at specific intervals, and a four-hour Clinical Reasoning and Judgement Assessment, featuring 20 questions in formats such as patient management problems (PMP) and key feature (KF) questions. Each exam is specifically tailored to the respective residency level and comprehensively covers the essential topics in the EM curriculum. Multiple-choice question, OSCE, and PMP-KF exams are widely recognized in all residency programs and represent the minimum requirement for residency evaluations in any educational training course. The exam results were analyzed and compared between the two groups, both before and after the implementation of GBL and gamification. It is essential to note that the other teaching components of the residency program (traditional methods such as theoretical classes, workshops, simulation sessions, and book reviews) remained consistent across both groups.
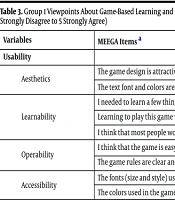
In this study, we evaluated learners’ perspectives in the first group on the new educational program using the validated Persian questionnaire, "A Model for the Evaluation of Educational Games (MEEGA)" (23). Additionally, general feedback and views of EM residents in group 1 regarding their new educational environment were collected through the validated Persian questionnaire, "The Short-Version of Postgraduate Hospital Educational Environment Measure (PHEEM)" (24). The Persian version of MEEGA includes two sections: (1) player experience, which consists of nine subscales totaling 22 questions; and (2) usability, comprising four subscales totaling nine questions. Respondents rate their answers on a Likert scale from 1 (strongly disagree) to 5 (strongly agree). The Persian short-version of PHEEM includes 12 questions in three categories, also rated on a Likert scale from 1 (strongly disagree) to 5 (strongly agree).
3.1. Sample Size Calculation and Data Analysis
All existing EM residents (30 residents across three residency levels) who participated in either intervention group were included in our study. After data collection, responses were entered into SPSS software (version 25.0). Data were tested for normal distribution using the Kolmogorov-Smirnov test. Descriptive indices such as frequency (percentage), mean (standard deviation), and median (interquartile range) were used to present the results. Independent t-tests and chi-square tests were applied to compare study variables, with a significance level set at 0.05.
4. Results
Thirty EM residents across three residency levels (PGY1, PGY2, and PGY3) participated in our study. Two parallel groups, each comprising 15 residents, were established. The mean age of participants in the first and second groups was 35.76 ± 7.36 and 32.61 ± 5.15 years, respectively. The majority of residents were female, accounting for 60.0% in group 1 and 53.3% in group 2. Data is presented in Table 1.
In the EM residency program, we evaluated residents’ performance biannually through 3 exams, each aimed at assessing especial competency. Written exam evaluated knowledge by MCQ tests, oral station exam evaluated procedural and management skills by OSCE and electronic online exam evaluated clinical reasoning and judgement by scenario-based PMP and KF questions. We compared the mean ± SD scores of these 3 important and general exams between the 2 groups after the interventions. As it is shown, we found that GBL and gamification improved all academic grades of residents more than the other group (P-value < 0.05) (Table 2).
| Exam Type | Group 1 | Group 2 | P-Value, a PGY2 | P-Value PGY2 | P-Value PGY3 | ||||
|---|---|---|---|---|---|---|---|---|---|
| PGY1 | PGY2 | PGY3 | PGY1 | PGY2 | PGY3 | ||||
| Written exam evaluating knowledge (MCQ) | 6.78 ± 1.19 | 7.35 ± 2.12 | 10.54 ± 1.19 | 7.02 ± 1.72 | 8.89 ± 2.03 | 12.31 ± 1.68 | 0.011 | 0.031 | 0.007 |
| Oral exam evaluating procedural skills (OSCE) | 7.74 ± 0.92 | 9.04 ± 0.83 | 9.36 ± 1.01 | 9.19 ± 0.89 | 10.74 ± 0.51 | 10.92 ± 0.52 | 0.005 | 0.012 | 0.036 |
| Electronic exam evaluating clinical reasoning and judgement (PMP, KF) | 5.07 ± 1.31 | 7.37 ± 1.72 | 10.04 ± 2.23 | 6.21 ± 1.41 | 9.42 ± 2.71 | 11.92 ± 1.32 | 0.023 | 0.047 | 0.005 |
Comparing the Mean Scores of Obligatory Exams After the Interventions Between the Two Groups (All Scores Are Out of 20)
In group 1, we asked residents’ viewpoints about the nature, design, strengths and weaknesses of GBL and gamification via MEEGA questionnaire. The results determined that residents were pleased with all items of “usability” and “player experience” (mean score > 3 agree and totally agree) (median score= 3 - 4). They said that the design was attractive. Rules were clear and easy to learn. Contents were useful and challenging. Games encouraged the cooperation, competition and interaction. Participating in the course was fun and effective in improving the knowledge and skills. Games increased learners’ attention and perceived learning. Data is shown in Table 3.
| Variables | MEEGA Items a | Mean ± SD | Median (IQR) |
|---|---|---|---|
| Usability | |||
| Aesthetics | The game design is attractive. | 4.36 ± 0.92 | 4 (3 - 4) |
| The text font and colors are well blended and consistent. | 4.16 ± 0.79 | 4 (3 - 4) | |
| Learnability | I needed to learn a few things before I could play the game. | 4.46 ± 0.50 | 4 (3 - 4) |
| Learning to play this game was easy for me. | 4.20 ± 0.55 | 4 (3 - 4) | |
| I think that most people would learn to play this game very quickly. | 4.03 ± 0.61 | 4 (3 - 4) | |
| Operability | I think that the game is easy to play. | 3.96 ± 0.99 | 3 (2 - 3) |
| The game rules are clear and easy to understand. | 4.00 ± 0.69 | 4 (3 - 4) | |
| Accessibility | The fonts (size and style) used in the game are easy to read. | 4.32 ± 1.12 | 4 (3 - 4) |
| The colors used in the game are meaningful. | 4.09 ± 0.94 | 4 (3 - 4) | |
| Player experience | |||
| Confidence | The contents and structure helped me to become confident that I would learn with this game. | 4.53 ± 0.50 | 4 (3 - 4) |
| Challenge | This game is appropriately challenging for me. | 4.80 ± 0.40 | 4 (3 - 4) |
| The game does not become monotonous as it progresses (repetitive or boring tasks). | 4.30 ± 0.46 | 4 (3 - 4) | |
| Satisfaction | Completing the game tasks gave me a satisfying feeling of accomplishment. | 4.13 ± 0.68 | 3 (2 - 3) |
| It is due to my personal effort that I managed to advance in the game. | 3.66 ± 1.18 | 3 (2 - 3) | |
| I feel satisfied with the things that I learned from the game. | 4.80 ± 0.40 | 4 (3 - 4) | |
| I would recommend this game to my colleagues. | 4.36 ± 0.49 | 4 (3 - 4) | |
| Social interaction | The game promotes cooperation and/or competition among players. | 3.93 ± 0.83 | 3 (2 - 3) |
| I felt good interacting with other players during the game. | 3.93 ± 0.94 | 3 (2 - 3) | |
| Fun | I had fun with the game. | 4.00 ± 0.69 | 3 (2 - 3) |
| Something happened during the game (game elements, competition, etc.) which made me smile. | 4.10 ± 0.75 | 4 (3 - 4) | |
| Focused attention | There was something interesting at the beginning of the game that captured my attention. | 3.96 ± 1.03 | 4 (3 - 4) |
| I was so involved in my gaming task that I lost track of time. | 3.53 ± 1.07 | 3 (2 - 3) | |
| I forgot about my immediate surroundings while playing this game. | 3.46 ± 0.97 | 3 (2 - 3) | |
| Relevance | The game contents are relevant to my interest. | 3.10 ± 1.12 | 3 (2 - 3) |
| It is clear to me how the contents of the game are related to the course. | 4.03 ± 0.85 | 3 (2 - 3) | |
| This game is an adequate teaching method for this course. | 3.13 ± 0.62 | 3 (2 - 3) | |
| I prefer learning with this game to learning through other ways (other teaching methods). | 4.30 ± 0.74 | 4 (3 - 4) | |
| Perceived learning | The game contributed to my learning in this course. | 4.36 ± 0.49 | 4 (3 - 4) |
| The game allowed for efficient learning compared with other activities in the course. | 3.96 ± 0.99 | 4 (3 - 4) | |
| User error protection | The game prevents me from making mistakes. | 2.43 ± 1.15 | 2 (1 - 2) |
| When I make a mistake, it is easy to recover from it quickly. | 4.50 ± 0.50 | 4 (3 - 4) |
Group 1 Viewpoints About Game-Based Learning and Gamification via Persian Model for the Evaluation of Educational Games Questionnaire (Each Item is Scored from 1 Strongly Disagree to 5 Strongly Agree)
We evaluated the overall quality of the new educational environment using the PHEEM Questionnaire after the intervention in the first group. All 15 residents shared their perspectives regarding their experience following the implementation of the GBL and gamification course. The results indicated that residents were satisfied with all aspects of "teachers' support and skills" and "work conditions and allocated time for learning" (mean score > 3, indicating agreement or strong agreement) (median score = 4). Additionally, residents highlighted an absence of harassment in this new environment post-GBL and gamification (mean score < 2, indicating disagreement or strong disagreement) (median score = 1.5 - 2). Data is presented in Table 4.
| Variables and Short-Version PHEEM Items a | Mean ± SD | Median (IQR) |
|---|---|---|
| Teachers support and skills | ||
| My clinical teachers have good teaching skills for giving consult to residents. | 4.23 ± 0.62 | 4 (3 - 4) |
| I get regular feedback from senior residents. | 4.06 ± 0.78 | 4 (3 - 4) |
| My clinical teachers provide me with good feedbacks on my strengths and weaknesses. | 4.30 ± 0.74 | 4 (3 - 4) |
| Senior residents and teachers utilize learning-teaching opportunities effectively. | 3.76 ± 0.81 | 4 (3 - 4) |
| Work conditions and allocated time for learning | ||
| My hours conform to the existing and approving rules in the ministry of health about residency program. | 3.96 ± 0.71 | 4 (3 - 4) |
| A separate time has been allocated for me as a resident, in order to use educational programs. | 4.26 ± 0.69 | 4 (3 - 4) |
| My workload in this job is fine. | 3.63 ± 0.85 | 4 (3 - 4) |
| My mandatory working hours are clearly stated to me. | 3.83 ± 0.98 | 4 (3 - 4) |
| No harassment | ||
| There is racism in this department. | 1.80 ± 0.80 | 2 (1 - 2) |
| There is sex discrimination in this department. | 1.53 ± 0.57 | 1.5 (1.5 - 2) |
| I have to perform tasks which is not suitable to my position as a resident. | 1.56 ± 0.62 | 1.5 (1.5 - 2) |
| I am being called to be present at the patient bed without any good reason. | 1.66 ± 0.75 | 1.5 (1.5 - 2) |
Group 1 Viewpoints About the New Educational Environment via Persian Short-Version of Postgraduate Hospital Educational Environment Measure Items (Each Item is Scored from 1 Strongly Disagree to 5 Strongly Agree)
5. Discussion
Gamification and GBL are establishing a significant presence in modern medical education. Today, numerous fields incorporate these innovative, engaging, and effective methods alongside traditional teaching. Although gamification and GBL differ in approach, both enhance learner motivation and engagement in the educational process (1-5).
In this study, we compared the effects of gamification and GBL with the use of podcasts and videos on EM residents' knowledge, skills, clinical reasoning, and judgment. The EM residents provided positive feedback on integrating GBL and gamification into their training program. They expressed satisfaction with all game elements, noting that GBL and gamification created an environment with consistent feedback from senior residents, designated time for each resident, constructive consultation from expert faculty, a balanced workload and work hours, and a lack of harassment or discrimination. Residents also found the GBL and gamification design, content, and rules to be enjoyable, engaging, challenging, and easy to learn. The course was described as accessible, practical, and conducive to learning. This approach fostered confidence, cooperation, focus, interaction, and healthy competition in absorbing the educational material. Additionally, it contributed to perceived learning through repeated sessions, direct supervision, and opportunities for self-assessment.
Our findings indicated a more substantial improvement in the mean exam scores of residents' medical knowledge, essential skills, and clinical reasoning following the implementation of GBL and gamification compared to the second group (P-value < 0.05).
O’Connell et al. evaluated the use of virtual gamification during COVID-19 to deliver core obstetrics and gynecology content to EM residents. They concluded that this gamification approach was effective, engaging, and educational, recommending it be included in EM residency programs (13).
Similarly, Salerno et al. demonstrated that incorporating gamification through challenging hazard simulations in the ED successfully integrated interactive training into the program. Their results showed that learners enjoyed performing procedures and collaborating with colleagues. This innovative method enhanced knowledge, psychomotor skills, and teamwork (14). Learner feedback was consistent with ours, noting the experience as fun and engaging, with sufficient allocated time, well-prepared facilitators, and content that was both useful and relevant to their learning needs.
Kobner et al. used a gamified approach combined with low-fidelity simulation to enhance clinical reasoning skills in a live virtual video conference. Participants reported an improved understanding of the topics along with increased engagement (15).
Lai et al. compared the effectiveness of a gamified approach with the conventional method in point-of-care ultrasound training (16). Similar to our findings, their study showed that gamification could improve both theoretical knowledge and practical skills, fostering greater interaction and motivation than the traditional approach.
Zhang et al. incorporated gamification into team-building exercises through an escape room experience. They concluded that gamification (escape room) combined with structured debriefing offered learners an engaging way to focus on teamwork and effective leadership. They also noted that the program's success aligned with ACGME milestones, suggesting that gamification could be integrated into the EM residency curriculum (19).
Downloading medical podcasts and educational videos has increased in recent years, especially following the pandemic (21). With virtual platforms providing easy, cost-free access, medical learners across specialties are increasingly choosing electronic learning formats. This trend began in EM and critical care and quickly spread to other fields. However, distance learning has faced criticism for its potential negative impacts on active learning and practice-changing behavior (21).
To the best of our knowledge, our newly designed course was the first to incorporate a comprehensive range of gaming models and designs, encompassing both GBL and gamification, into an EM residency training program. It covered over 70% of the core topics in the approved EM residency curriculum. The positive feedback and improved academic achievement scores underscore the importance of enhancing educational systems. Given the limitations of traditional and bedside teaching, we encourage other educational programs to adopt GBL and gamification in their training courses.
5.1. Limitation
In this study, we did not specify the sample size due to the limited number of residents at each level of residency, leading us to include all available participants in the two intervention groups. The most significant limitation was that this was a single-center study, so the results may not be fully generalizable to other similar populations. Additionally, we did not administer a pre-test exam before the intervention. Lastly, we made a concerted effort to use identical topics and content across both intervention groups.
Future studies could benefit from comparing different medical specialties with larger sample sizes and exploring diverse gamification and GBL methods.
5.2. Conclusions
The feedback received from EM residents across PGY1, PGY2, and PGY3 levels indicated that GBL and gamification effectively engaged learners in their learning process. Residents enjoyed the interactive, cooperative, and competitive environment created by these fun and engaging games. Game-based learning and gamification demonstrated the potential to enhance learners’ academic performance, as reflected by increases in mean ± SD scores in knowledge, practical skills, clinical reasoning, and judgment following the intervention.
5.3. Highlights
Game-based learning and gamification significantly improved knowledge, skills, clinical reasoning, and judgment among EM residents.
EM residents largly agreed on the positive impacts of this intervention on their residency training program.
The intervention encouraged EM residents’ cooperation, competition and interaction and also increased their attention and perceived learning.
5.4. Lay Summary
Gamification and GBL are helping traditional teaching in modern medical education. Various fields incorporate these innovative, engaging, and effective methods in order to enhance learners’ motivation and engagement in the educational process. In our study, EM residents provided positive feedbacks on integrating gamification and GBL in to their training program. They expressed that gamification and GBL created an environment with consistent feedbacks from senior residents, designated time for each resident, constructive consultation from expert faculty. They also found gamification and GBL’s design, content, and rules to be enjoyable, engaging, challenging, and easy to learn.