1. Background
The novelty of this study lies in its comprehensive investigation of patients’ attitudes toward various aspects of bedside teaching (BST) using a validated instrument within a representative Iranian hospital setting. Despite numerous studies conducted in Islamic countries, there is a notable lack of comprehensive research examining patients’ attitudes toward BST in the Iranian context. This study addresses this gap by exploring the perspectives of patients hospitalized in Iran, offering insights tailored to the cultural and clinical environment of the country. Despite several studies conducted in Islamic countries, there is a clear lack of comprehensive research examining patients’ attitudes towards BST in the Iranian context. This study addresses this gap by exploring the perspectives of patients hospitalized in Iran, offering insights tailored to the cultural and clinical environment of the country.
Bedside teaching is a critical component of the medical education system, equipping students with essential clinical skills such as history taking, physical examination, clinical reasoning, treatment decision-making, patient communication, and overall professional conduct as a physician (1-3). While the educator-learner relationship is often considered the most crucial aspect of clinical education, patient enthusiasm and cooperation significantly impact educational quality (4, 5). Patients, through their experiences with illness, disability, and the social determinants of health, possess unique skills that convey valuable educational messages not found in textbooks (6-8).
Research on patients’ attitudes and practices regarding clinical education reveals that most patients hold a positive view of medical students’ involvement in their care and treatment. Patients express satisfaction in contributing to the enhancement of medical students’ training, which ultimately improves community healthcare quality (9-11). However, this perspective varies across regions and is influenced by social, demographic, and cultural factors (10, 12). Studies indicate that female patients, male students, and strong adherence to religious beliefs increase the likelihood of patient non-cooperation (13-16).
In Iran, approximately half of the general medical education duration and the entirety of specialized education rely on BST. During this period, students participate in medical and surgical departments at designated times, receiving patient-based clinical training where patients serve as educational tools (17, 18). Recent cultural developments, standard guidelines, and ethical considerations have heightened attention to patient rights and informed consent, granting patients the choice regarding student involvement in their care and treatment (19, 20). Additionally, the expansion of medical education and the tenfold increase in medical student numbers have led to the establishment of more educational and medical centers, enhancing patient awareness of medical students. Understanding patients’ views on student presence at their bedside and the factors influencing their attitudes is essential to fostering maximum patient cooperation in BST.
2. Objectives
Although numerous studies worldwide have examined patients’ attitudes toward BST for medical students, most have focused on specific components of BST. Furthermore, despite many studies being conducted in Islamic countries, cultural and religious differences limit the available information about Iranian patients. This study was designed and conducted to investigate patients’ attitudes toward various aspects of BST for clinical students.
3. Methods
This cross-sectional study was conducted in 2019 on 250 patients admitted to Shahid Beheshti Hospital in Kashan, Iran. Convenience sampling was employed, selecting patients discharged from the hospital’s internal and surgical wards after completing their treatment. Sampling continued until the required sample size was achieved. Although convenience sampling may introduce selection bias by excluding certain demographic subsets, the authors attempted to mitigate this and enhance the study’s validity by controlling and assessing the sample’s representativeness.
Inclusion criteria were age over 18 years, absence of cognitive and psychiatric illnesses, and no communication disorders. Patients with decreased consciousness, acute life-threatening conditions, or those who did not complete the questionnaire despite follow-up were excluded. Informed written consent was obtained from all participants after providing a thorough explanation of the research methods and objectives. Excluding psychiatric and cognitively impaired patients ensured data quality and integrity, as these individuals might not provide reliable or informed responses. This exclusion criterion is standard in patient-attitude surveys to prevent potential biases.
The sample size was determined based on previous studies, where 79% of patients believed that student presence improved treatment quality. With a type I error of 0.05 and a margin of error (d) of 0.1, the minimum sample size was calculated to be 64 using a standard formula for estimating a population proportion at a 95% confidence level. However, the sample was increased to 250 to enhance statistical power, improve representativeness, and facilitate subgroup analysis.
Data were collected using a translated version of the "Patients’ Acceptance of Medical Students" Questionnaire designed by Marwan et al. (15). This questionnaire comprises two main sections. The first section gathers demographic information about the patients. The second section includes 11 questions assessing patients’ acceptance of various aspects of student presence at the bedside. Each question offers four response options: "Male students only", "female students only", "both sexes", and "none" from which the patient selects one.
To ensure validity, the questionnaire was initially translated from English to Persian by two individuals fluent in Persian. A specialist physician familiar with English and translation reviewed and refined the translated version. Subsequently, two other translators retranslated the Persian version back into English. A specialist physician then compared the original and back-translated English versions to ensure conceptual and structural consistency. The Persian version was presented to 10 medical education professors, and their feedback was incorporated into the questionnaire both qualitatively and quantitatively. Qualitative feedback addressed sentence structure, content, and spelling. In the quantitative assessment, professors rated each question as "necessary", "useful but unnecessary", or "unnecessary". Finally, using the following formula:
(CVR = content validity ratio, nE = number of necessary comments, and N = total number of professors)
It was initially considered to remove questions based on the content validity ratio (CVR) assessment. However, according to the results, no question was found to be unnecessary, and thus, none were deleted. It should be noted that there were no challenges in adapting the questionnaire to the local context.
To evaluate the reliability of the questionnaire, the test-retest method was employed. The questionnaire was administered twice to 30 hospitalized patients at three-day intervals. The correlation between the two administrations was examined, revealing acceptable reliability (P < 0.001, r = 0.89). A correlation coefficient of r = 0.89 indicates strong test-retest reliability, suggesting that the questionnaire consistently captures patients’ attitudes over time, making it a stable and trustworthy measurement tool.
Subsequently, the questionnaire was administered to 250 hospitalized patients at discharge, with responses collected directly from the patients. For illiterate patients, the questionnaire was completed with the assistance of a companion. All patients were given the option to participate voluntarily in the study. To maintain privacy and encourage patient cooperation, the questionnaires were completed without recording any identifying information.
The collected data were analyzed using SPSS software, version 24. Quantitative results are reported as mean ± standard deviation, while qualitative results are presented as absolute and relative frequencies. Chi-square and Fisher’s exact tests were used for data analysis. All tests were two-tailed, and P-values of less than 0.05 were considered significant.
4. Results
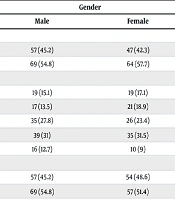
Out of 250 questionnaires distributed among patients, 237 were completed correctly. The mean age of participants was 44.11 ± 15.02 years, with an age range of 18 to 73 years. Among the participants, 126 (53.2%) were male. Additionally, 122 patients (51.5%) were hospitalized in medical wards, while the remainder were in surgical wards. The demographic characteristics of the patients by gender are presented in Table 1.
| Variables | Gender | P-Value | |
|---|---|---|---|
| Male | Female | ||
| Age (y) | 0.64 | ||
| < 40 | 57 (45.2) | 47 (42.3) | |
| > 40 | 69 (54.8) | 64 (57.7) | |
| Education | 0.66 | ||
| Illiterate | 19 (15.1) | 19 (17.1) | |
| Primary school | 17 (13.5) | 21 (18.9) | |
| Middle school | 35 (27.8) | 26 (23.4) | |
| High school | 39 (31) | 35 (31.5) | |
| University | 16 (12.7) | 10 (9) | |
| Marital status | 0.6 | ||
| Single | 57 (45.2) | 54 (48.6) | |
| Married | 69 (54.8) | 57 (51.4) | |
| Location | 0.78 | ||
| City | 98 (77.8) | 88 (79.3) | |
| Village | 28 (22.2) | 23 (20.7) | |
| Type of disease | 0.22 | ||
| Internal | 66 (52.4) | 67 (60.4) | |
| Surgical | 60 (47.6) | 44 (39.6) | |
Demographic Characteristics of Study Patients a
Regarding patients’ acceptance of medical students’ presence for BST, it was generally found that patients agreed with the presence of students, irrespective of gender. The highest rate of disagreement pertained to performing diagnostic or therapeutic measures without the supervising professor (19.4%), while the lowest disagreement was related to students studying medical records (5.1%). Female students were preferred over male students by patients. The presence of a professor during medical history taking, examinations, and diagnostic/therapeutic procedures by students increased patient agreement. Table 2 illustrates patients’ attitudes toward various dimensions of BST in medical students.
| Variables | Permit Male Students Only | Permit Female Students Only | Permit Both Genders of Students | Not to Permit Either Gender of Students |
|---|---|---|---|---|
| To read medical files | 7 (3) | 10 (4.2) | 208 (87.8) | 12 (5.1) |
| To be present in outpatient clinic | 6 (2.5) | 12 (5.1) | 183 (78.2) | 36 (15.2) |
| To attend the ward rounds | 8 (3.4) | 8 (3.4) | 205 (86.5) | 16 (6.8) |
| To be present in the operation theatre | 3 (1.3) | 5 (2.1) | 208 (87.8) | 21 (8.9) |
| To take medical history with the presence of a supervising professor | 10 (4.2) | 13 (5.5) | 198 (83.5) | 16 (6.8) |
| To take medical history without the presence of a supervising professor | 12 (5.1) | 13 (5.5) | 188 (79.3) | 24 (10.1) |
| To be present in examination procedure | 7 (3) | 10 (4.2) | 204 (86.1) | 16 (6.8) |
| To examine with the presence of a supervising professor | 6 (2.5) | 13 (5.5) | 196 (82.7) | 22 (9.3) |
| To examine without the presence of a supervising professor | 10 (4.2) | 13 (5.5) | 176 (74.3) | 38 (16) |
| To perform diagnostic/other procedures with the presence of a supervising professor | 12 (5.1) | 12 (5.1) | 180 (75.9) | 33 (13.9) |
| To perform diagnostic/other procedures without the presence of a supervising professor | 12 (5.1) | 27 (11.4) | 152 (64.1) | 46 (19.4) |
Patients’ Attitudes Towards Bedside Teaching a
In terms of factors affecting patients’ attitudes toward BST, women were significantly more opposed than men to examinations conducted without a teacher and to diagnostic and therapeutic measures performed with or without a teacher. Conversely, men reported disagreement only regarding students’ presence in outpatient clinics (23.8% vs. 5.4%, P < 0.001) and during surgery (12.7% vs. 4.5%, P = 0.04) compared to female patients.
The age group of patients influenced attitudes toward student presence during inpatient visits, surgery, and medical history taking, both in the presence and absence of a professor, as well as examinations and diagnostic/therapeutic measures. Patients over 40 years of age showed less disagreement than younger patients.
Regarding the relationship between education level and attitudes toward BST, patients with higher education levels showed more disagreement, particularly concerning student presence during examinations in inpatient departments, surgery, and medical history taking without a professor, as well as examinations by students in the presence of a professor.
Place of residence significantly affected attitudes toward diagnostic/therapeutic procedures without a teacher, with rural patients expressing less disagreement (P = 0.001). Patients with a history of hospitalization were significantly more opposed to students performing examinations without a professor and to diagnostic/therapeutic measures with a professor present.
Patients hospitalized for internal diseases showed more disagreement during medical history taking without a professor, examinations by students with a professor present, and diagnostic/therapeutic measures with or without a professor, compared to surgical ward patients. Tables 3 and 4 present the factors affecting patients’ attitudes toward BST.
| Variables and Attitudes | Gender | Age | Education | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | P-Value | < 40 | > 40 | P-Value | Middle School and Lower | High School and Upper | P-Value | |
| To read medical files | 0.15 | 0.14 | 0.57 | ||||||
| Agree | 9 (7.1) | 3 (2.7) | 8 (7.7) | 4 (3) | 6 (4.4) | 6 (6) | |||
| Disagree | 117 (92.9) | 108 (97.3) | 96 (92.3) | 129 (97) | 131 (95.6) | 94 (94) | |||
| To be present in outpatient clinic | > 0.001 | 0.42 | 0.12 | ||||||
| Agree | 30 (23.8) | 6 (5.4) | 18 (17.3) | 18 (13.5) | 25 (18.2) | 11 (11) | |||
| Disagree | 96 (76.2) | 105 (64.6) | 86 (82.7) | 115 (86.5) | 112 (81.8) | 89 (89) | |||
| To attend the ward rounds | 0.12 | 0.02 | 0.008 | ||||||
| Agree | 12 (9.5) | 4 (3.6) | 12 (11.5) | 4 (3) | 4 (2.9) | 12 (12) | |||
| Disagree | 114 (90.5) | 107 (96.4) | 92 (88.5) | 129 (97) | (97.1) 133 | (88.0) 88 | |||
| To be present in the operation theatre | 0.04 | > 0.001 | > 0.001 | ||||||
| Agree | 16 (12.7) | 5 (4.5) | 20 (19.2) | 1 (0.8) | 3 (2.2) | 18 (18) | |||
| Disagree | 110 (83.7) | 106 (95.5) | 84 (80.8) | 132 (99.2) | 134 (97.8) | 82 (82) | |||
| To take medical history with the presence of a supervising professor | 0.3 | 0.06 | 0.24 | ||||||
| Agree | 11 (8.7) | 5 (4.5) | 11 (10.6) | 5 (3.8) | 7 (5.1) | 9 (9) | |||
| Disagree | 115 (91.3) | 106 (95.5) | 93 (89.4) | 128 (96.5) | 130 (94.9) | 91 (91) | |||
| To take medical history without the presence of a supervising professor | 0.59 | 0.005 | 0.03 | ||||||
| Agree | 14 (11.1) | 10 (9) | 17 (16.3) | 7 (5.3) | 9 (6.6) | 15 (15) | |||
| Disagree | 112 (88.9) | 101 (91) | 87 (83.7) | 126 (94.7) | 128 (93.4) | 85 (85) | |||
| To be present in examination procedure | 0.8 | 0.6 | 0.09 | ||||||
| Agree | 9 (7.1) | 7 (6.3) | 8 (7.7) | 8 (6) | 6 (4.4) | 10 (10) | |||
| Disagree | 117 (92.9) | 104 (93.7) | 96 (92.3) | 125 (94) | 131 (95.6) | 90 (90) | |||
| To examine with the presence of a supervising professor | 0.14 | 0.05 | 0.03 | ||||||
| Agree | 15 (11.9) | 7 (6.3) | 14 (13.5) | 8 (6) | 8 (5.8) | 14 (14) | |||
| Disagree | 111 (88.1) | 104 (93.7) | 90 (86.5) | 125 (94) | 129 (94.2) | 86 (86) | |||
| To examine without the presence of a supervising professor | 0.03 | 0.02 | 0.73 | ||||||
| Agree | 14 (11.1) | 24 (21.6) | 23 (22.1) | 15 (11.3) | 21 (15.3) | 17 (17) | |||
| Disagree | 112 (88.9) | 87 (78.4) | 81 (77.9) | 118 (88.7) | 116 (84.7) | 83 (83) | |||
| To perform diagnostic/other procedures with the presence of a supervising professor | 0.005 | 0.04 | 0.68 | ||||||
| Agree | 10 (7.9) | 23 (20.7) | 20 (19.2) | 13 (9.8) | 18 (13.1) | 15 (15) | |||
| Disagree | 116 (92.1) | 88 (79.3) | 84 (80.8) | 120 (90.2) | 119 (86.9) | 85 (85) | |||
| To perform diagnostic/other procedures without the presence of a supervising professor | > 0.001 | 0.47 | 0.6 | ||||||
| Agree | 13 (10.3) | 33 (29.7) | 18 (17.3) | 28 (21.1) | 25 (18.2) | 21 (21) | |||
| Disagree | 113 (89.7) | 78 (70.3) | 86 (82.7) | 105 (78.9) | 112 (81.8) | 79 (79) | |||
The Effects of Gender, Age Group and Educational Status on Patients’ Attitude Towards Bedside Teaching a
| Variables and Attitudes | Living Place | Admission History | Type of Disease | ||||||
|---|---|---|---|---|---|---|---|---|---|
| City | Village | P-Value | Yes | No | P-Value | Internal | Surgical | P-Value | |
| To read medical files | 0.99 > | 0.77 | 0.56 | ||||||
| Agree | 10 (5.4) | 2 (3.9) | 8 (5.6) | 4 (4.3) | 8 (6) | 4 (3.8) | |||
| Disagree | 176 (94.6) | 49 (96.1) | 135 (94.4) | 90 (95.7) | 125 (94) | 100 (96.2) | |||
| To be present in outpatient clinic | 0.91 | 0.52 | 0.42 | ||||||
| Agree | 28 (15.1) | 8 (15.7) | 20 (14) | 16 (17) | 18 (13.5) | 18 (17.3) | |||
| Disagree | 158 (84.9) | 43 (84.3) | 123 (86) | 78 (83) | 115 (86.5) | 86 (82.7) | |||
| To attend the ward rounds | 0.2 | 0.16 | 0.13 | ||||||
| Agree | 15 (8.1) | 1 (2) | 7 (4.9) | 9 (9.6) | 12 (9) | 4 (3.8) | |||
| Disagree | 171 (91.9) | 50 (98) | 136 (95.1) | 85 (90.4) | 121 (91) | 100 (96.2) | |||
| To be present in the operation theatre | 0.58 | 0.75 | 0.06 | ||||||
| Agree | 18 (9.7) | 3 (5.9) | 12 (8.4) | 9 (9.6) | 16 (12) | 5 (4.8) | |||
| Disagree | 168 (90.3) | 48 (94.1) | 131 (91.6) | 85 (90.4) | 117 (88) | 99 (95.2) | |||
| To take medical history with the presence of a supervising professor | 0.53 | 0.73 | 0.13 | ||||||
| Agree | 14 (7.5) | 2 (3.9) | 9 (6.3) | 7 (7.4) | 12 (9) | 4 (3.8) | |||
| Disagree | 172 (92.5) | 49 (96.1) | 134 (93.7) | 87 (92.6) | 121 (91) | 100 (96.2) | |||
| To take medical history without the presence of a supervising professor | 0.79 | 0.51 | 0.02 | ||||||
| Agree | 20 (10.8) | 4 (7.8) | 13 (9.1) | 11 (11.7) | 19 (14.3) | 5 (4.8) | |||
| Disagree | 116 (89.2) | 47 (82.2) | 130 (90.9) | 83 (88.3) | 114 (85.7) | 99 (95.2) | |||
| To be present in examination procedure | 0.99 > | 0.85 | 0.13 | ||||||
| Agree | 13 (7) | 3 (5.9) | 10 (7) | 6 (6.4) | 12 (9) | 4 (3.8) | |||
| Disagree | 173 (93) | 48 (94.1) | 133 (93) | 88 (93.6) | 121 (91) | 100 (96.2) | |||
| To examine with the presence of a supervising professor | 0.43 | 0.56 | 0.04 | ||||||
| Agree | 19 (10.2) | 3 (5.9) | 12 (8.4) | 10 (10.6) | 17 (12.8) | 5 (4.8) | |||
| Disagree | 167 (89.8) | 48 (94.1) | 131 (91.6) | 84 (89.4) | 116 (87.2) | 99 (95.2) | |||
| To examine without the presence of a supervising professor | 0.35 | < 0.001 | 0.34 | ||||||
| Agree | 32 (17.2) | 6 (11.8) | 12 (8.4) | 26 (27.7) | 24 (18) | 14 (13.5) | |||
| Disagree | 154 (82.8) | 45 (88.2) | 131 (91.6) | 68 (72.3) | 109 (82) | 90 (86.5) | |||
| To perform diagnostic/ other procedures with the presence of a supervising professor | 0.96 | < 0.001 | 0.04 | ||||||
| Agree | 26 (14) | 7 (13.7) | 10 (7) | 23 (24.5) | 24 (18) | 9 (8.7) | |||
| Disagree | 160 (86) | 44 (86.3) | 133 (93) | 71 (75.5) | 109 (82) | 95 (91.3) | |||
| To perform diagnostic/ other procedures without the presence of a supervising professor | 0.001 | 0.003 | 0.007 | ||||||
| Agree | 44 (23.7) | 2 (3.9) | 19 (13.3) | 27 (28.7) | 34 (25.6) | 12 (11.5) | |||
| Disagree | 142 (76.3) | 49 (96.1) | 124 (86.7) | 67 (71.3) | 99 (74.4) | 72 (88.5) | |||
The Effects of Living Place, Admission History and Type of Disease on Patients’ Attitude Towards Bedside Teaching a
5. Discussion
This cross-sectional study was designed to investigate the attitudes of patients in Kashan toward BST of medical students. It was found that a significant proportion of patients have a positive attitude toward the presence of medical students in teaching hospitals. Similar results have been reported in limited studies conducted in Iran. In studies by Izadi et al. and Abdian et al., using questionnaires on outpatient patients, the majority expressed a positive attitude toward the presence of medical students at their bedside (21, 22).
Relevant studies in other countries have yielded similar findings. Sayed-Hassan et al. conducted a study in three teaching hospitals in Damascus, showing that most patients agree with the presence of medical students during consultations (12). Choudhury et al. examined patients’ attitudes in the United Kingdom and found that, generally, patients have a positive attitude toward medical students’ presence during their medical consultations (23). Haffling and Hakansson studied 495 adult patients at Swedish health centers, finding that 92% were satisfied with counseling by medical students, citing self-interest and altruism as primary reasons. Most patients expressed willingness to consult with another student (11). Other studies have reported similar results (24-27).
Although patients generally have a positive attitude toward the presence of medical students and BST, they are less satisfied with learners’ involvement in the treatment process. As students’ roles in care become more prominent and their involvement in practical processes increases, patient cooperation decreases. While most patients agree with students studying their medical records regardless of gender, they express dissatisfaction with students performing practical procedures, clinical examinations, or diagnostic and therapeutic measures. Cultural issues and religious beliefs often underlie this dissatisfaction. However, studies in areas with different cultural and religious contexts have shown similar results (11, 12, 24, 28).
We found that patients’ satisfaction and cooperation significantly increase when examinations and treatment procedures by students are conducted in the presence of supervising professors. Previous studies have reported similar findings. Ben Salah et al. conducted a study on 356 patients in Tunisia, revealing that patient satisfaction with examinations, particularly in special areas, increases significantly with the presence of professors. For instance, 63.1% of patients agreed to breast examinations by students without a supervising professor, but this rate increased to over 71% with a professor present (9). In a study by Sayad-Hassan et al. at several Damascus teaching hospitals, it was found that, in the absence of a supervising professor, patients allowed examinations by students in only 40.2% of cases, whereas this rate increased to 81.5% with a professor present (12). Marwan et al. examined 932 patients at Kuwait Medical University teaching hospitals and found that, without a supervising professor, only 38.7% of patients were satisfied with medical examinations by students, but this satisfaction increased to 72.3% with a professor’s presence and supervision (15).
Regardless of cultural or religious issues, patients’ dissatisfaction with clinical examinations, especially in certain body regions, can be attributed to concerns about privacy breaches, student moral competence, and lack of confidence in the learner’s skills. The increase in patient satisfaction with student examinations in the presence of a supervising professor confirms these factors.
This study found that patient characteristics influence their reactions to medical students’ presence in their treatment process. In cases where students have minimal direct contact with patients (such as studying medical records or taking a history), female patients are more cooperative. However, for examinations and procedures requiring student or patient contact, female patients’ acceptance significantly decreases, while male patients are more satisfied with examinations by both sexes. This may be evaluated as emotional intelligence, which is significantly higher in women compared to men, potentially improving the patient-therapist relationship (29).
Similar results have been observed in previous studies. In a study by Shann and Wilson in the United Kingdom, 500 patients at a urogenital clinic expressed their views on student presence during examinations, revealing that young women had the highest level of dissatisfaction with learners’ presence, regardless of gender (30). Shah-khan et al. assessed 100 patients at an outpatient colorectal surgery clinic and found that women were significantly less likely than men (77% vs. 86%) to accept students’ presence during examinations (31). Similar results have been reported in other studies (9, 24, 28).
Regarding the factors influencing patients’ attitudes toward examinations or diagnostic/therapeutic measures by students, it was found that older patients, those with lower education levels, those with a history of hospitalization, and patients who had undergone surgery exhibited the most positive attitudes toward BST. Older adults tend to prioritize emotionally meaningful experiences and dismiss negative emotions associated with stressful or unpleasant events. In contrast, younger adults prioritize goals related to acquiring knowledge and delaying emotional gratification (32). Although previous studies have shown that older patients have a better attitude toward examinations and interventions by students, no relationship was observed between patients’ education level and their attitude in these studies (31, 33).
In the study by Sayed-Hassan et al., it was observed that most patients are not well-informed about the role and extent of medical students’ participation in treatment and their right to accept or reject students’ involvement in these processes (12). It seems that the greater cooperation of older patients or those with lower education levels may be due to reasons other than a low level of awareness. Saeed et al. found that patient awareness and satisfaction increase positive attitudes and encourage participation in educational programs (34). Further studies are needed to accurately understand the effect of patients’ awareness on their attitudes toward different aspects of clinical education (35-37).
It is important to note that with scientific advancements across all fields, conducting more studies in this area will lead to changes in educational policies and improve patients’ perceptions of medical staff and students. The use of new technologies, such as artificial intelligence, will be beneficial in achieving this goal (38).
Most available questionnaires examining patients’ attitudes toward BST contain numerous questions or do not fully explore the various dimensions of BST. Therefore, they were not suitable for use due to potential patient non-cooperation and failure to achieve research objectives. The questionnaire used, despite being concise and useful, was not applicable to certain patient groups, such as pediatric patients, and did not allow for reviewing the opinions of healthcare providers in certain wards, such as psychiatry.
Although patients were informed that this study would not affect their treatment and was not a measure to express dissatisfaction or gratitude regarding their medical condition, it is possible that some patients conveyed their feelings about other issues through their responses. However, we lacked a tool to identify such patients. The absence of appropriate and reliable tools to accurately determine patients’ socioeconomic status and its effect on their attitude toward BST, the investigation of only one treatment center, and the sampling method were additional limitations of this study.