1. Context
Breast milk is an ideal food that helps the newborn adapt to life, protects the newborn from infectious diseases thanks to its unique content, and meets the physical and psychological needs of the newborn (1-3). The World Health Organization (WHO) recommends that every neonate should be fed only breast milk (OBM) for the first 6 months (4). According to the WHO 2020 data, the rate of giving OBM for the first 6 months is 44% worldwide, and this rate is 41% in Turkey (5).
Breastfeeding is a healthy, reliable, economical, and effortless way of feeding that strengthens the bond between the mother and newborn (6). Breastfeeding has various benefits for the mother, neonate, and society. Some of these benefits include protecting the newborn from diseases (e.g., pneumonia, gastrointestinal system problems, and measles), affecting neurological development (7), contributing to uterine involution by affecting the mother’s postpartum uterine contractions, and reducing the risk of postpartum depression for mothers (6, 8). Mothers who do not have an adequate support system during the breastfeeding process might experience problems related to the process (9, 10). For this reason, breastfeeding education should be given to all mothers on breastfeeding and breast milk, starting from the pregnancy period. It is stated that especially breastfeeding education given by midwives/nurses increases the rate of breastfeeding in women and causes them to experience fewer breastfeeding problems (11-13).
In order to increase breastfeeding success, mothers and their spouses should be provided with individual or group education in the hospital environment or at home (14). Nurses, as educators, caregivers, and consultants, can contribute to the development of positive breastfeeding behavior by mothers using their roles in the breastfeeding process. According to the literature, there are studies examining the effectiveness of the training given by nurses in ensuring the continuity of breastfeeding (15-17). For example, in Öztürk’s study that evaluated the pregnant women who received or did not receive breastfeeding training during pregnancy, the rate of breastfeeding within the first hour of mothers who received training during the postpartum first week was higher (88.3%) than those who did not receive education (78.8%) (18).
Breastfeeding, breast milk, and postnatal care by health professionals in a multidisciplinary team approach is important for raising healthy generations. In addition, it will be a guide for researchers who would like to carry out scientific research to develop different educational methods and techniques to reach a source where there are theses written to date on the subject they are interested in.
The purpose of this systematic review was to examine the postgraduate theses written in the last 10 years in Turkey on breastfeeding training in the field of midwifery/nursing.
The research questions are as follows:
(1) For which sample groups did postgraduate theses in the field of midwifery/nursing provide
breastfeeding education?
(2) In which process do postgraduate theses in midwifery/nursing in Turkey usually train breastfeeding (prenatal or postnatal)?
(3) What are the results achieved at the end of the training?
2. Methods
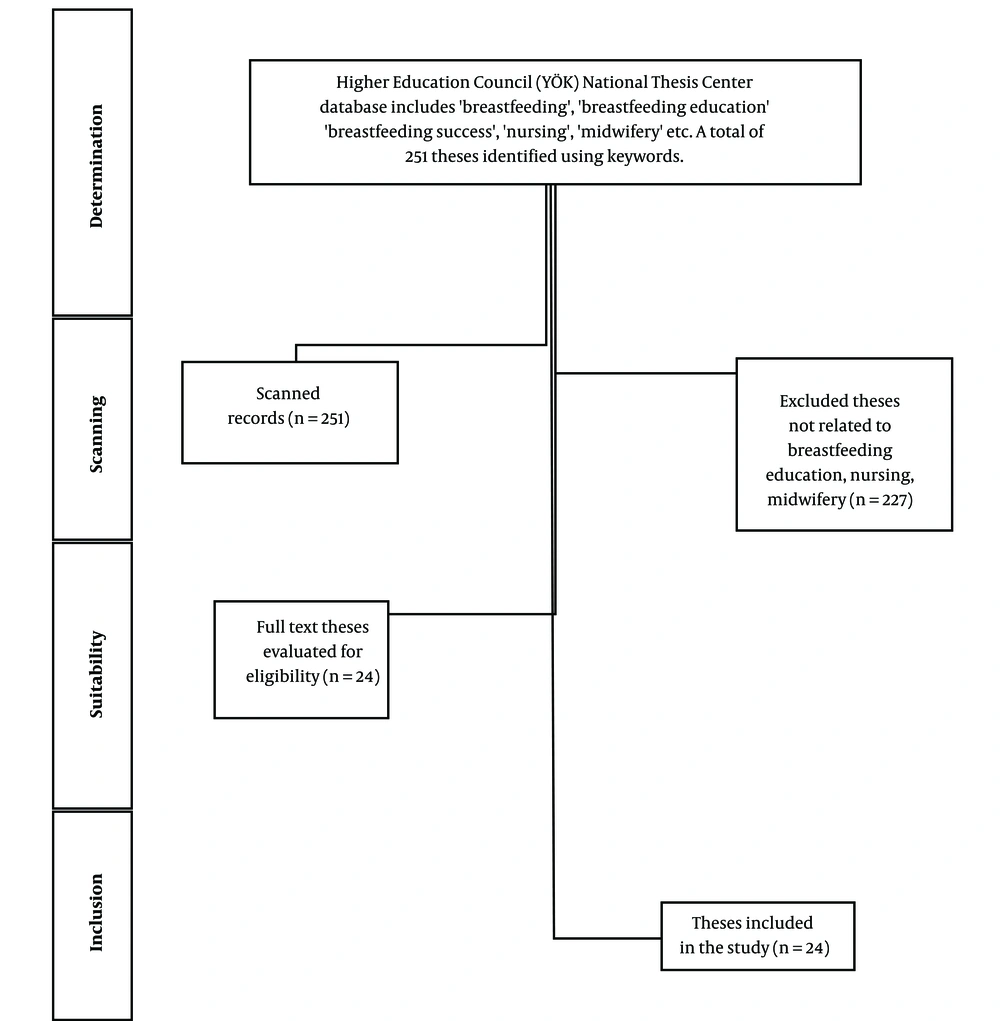
This systematic review was conducted by considering the PRISMA criteria (19). Using the National Thesis Center database of the Council of Higher Education (YÖK), 251 theses (master’s and doctorate) obtained between 2012 - 2022 constituted the universe of the study. In this systematic review, the data scanning process was evaluated in Turkish using several keywords, including “Breastfeeding”, “Breastfeeding Education”, “Breastfeeding Success”, “Nursing”, and “Midwifery”. The abstracts of 251 theses, scanned within March 20 and April 20, 2022, were systematically examined. Then, 24 theses related to breastfeeding and breastfeeding education, which were suitable for the purpose of the study, formed the sample of the research (Figure 1).
2.1. Inclusion Criteria
(1) Accessible full text
(2) In the field of nursing/midwifery
(3) About breastfeeding education
(4) Studies published in the national thesis center within 2012 - 2022
In this study, theses in the National Thesis Center of YÖK were scanned according to the PICOS design.
(P: Patient): Pregnant women, puerperant women, and fathers
(I: Intervention): Breastfeeding education
(C: Comparison): No breastfeeding education
(O: Outcomes): Breastfeeding success, exclusive breastfeeding, breastfeeding, and self-efficacy
(S: Study design): Experimental, quasi-experimental, and intervention studies published in Turkish with available full texts
2.2. Ethical Aspect of Research
Ethical permission was not obtained because the master’s and doctoral theses that were open to access were used in this systematic review. The theses were selected by the researchers considering the PRISMA checklist.
2.3. Analysis of Data
The data were evaluated using a data summary form prepared by the researchers. The data summary form included author, advisor, year, department, graduate level, study purpose, sample size, research type/method, data collection tools, and results of the studies. The data summary forms were evaluated independently by the researchers and filled with consensus.
3. Results
The information of the theses made in Turkey between 2012 - 2022 on postgraduate level breastfeeding, breastfeeding education, breastfeeding success, nursing and midwifery is given in A total of 58% of the theses obtained using keywords were quasi-experimental (42%) studies performed in the postnatal period. Moreover, 79% of the theses were in the field of nursing, and 63% of them were master’s theses. Furthermore, 75% of these theses were written in 2018 and later (Table 1).
| Variables | No. (%) |
|---|---|
| Period | |
| Antenatal period (prenatal) | 10 (42) |
| Postnatal period (postnatal) | 14 (58) |
| Thesis type | |
| Master’s | 15 (63) |
| Doctorate | 9 (37) |
| Department | |
| Nursing | 19 (79) |
| Midwifery | 5 (21) |
| Research type | |
| Experimental | 9 (37) |
| Semi-experimental | 10 (42) |
| Intervention research | 5 (21) |
| Years | |
| 2012 - 2017 | 6 (25) |
| 2018 - 2022 | 18 (75) |
This systematic review investigated the effectiveness of 24 theses written in breastfeeding education in Turkey within 2012 - 2022. The theses included in the research were evaluated under three headings, namely prenatal breastfeeding education (Table 2), postpartum breastfeeding education (Table 3), and model/theory-based breastfeeding education (Table 4).
| Author, Consultant (Year) | Department; Postgraduate Level | Purpose of Research | Sample | Research Type/Method | Data Collection Tools | Conclusion |
|---|---|---|---|---|---|---|
| Başak Tatar, Nevin Hotun Şahin (2019) (20) | Nursing; Master’s degree | To evaluate the effect of breastfeeding education given to nulliparous pregnant women on postpartum breastfeeding status | Experiment: 50; control: 50 | Breastfeeding training was given to nulliparous pregnant women who were hospitalized in the experimental delivery room and who were not in the active phase, with the illustrated breastfeeding guide prepared by the Ministry of Health. No training was given to the control group. | Introductory information form; Breastfeeding Self-efficacy Scale-short Form (antenatal and postnatal form); LATCH Breastfeeding Diagnostic Scale | It was observed that providing breastfeeding education in the prenatal period positively affects breastfeeding success and breastfeeding self-efficacy of nulliparous pregnant women who have no breastfeeding experience. |
| Rukiye Öztürk, Nurcan Özyazicioğlu (2018) (18) | Nursing; Master’s degree | To determine the effect of prenatal breastfeeding and breastfeeding education on breastfeeding success and breastfeeding self-efficacy perception of mothers | Experiment: 40; control: 40 | Semi-experimental; A total of 4 hours (2 sessions) of breast milk and breastfeeding training was given to the pregnant women in the experimental group by the researcher in the pregnant training room of the hospital in groups of 4 - 5. Standard prenatal follow-up provided by the Ministry of Health was applied to the control group. At the end of the first week of DS, breastfeeding self-efficacy perception and breastfeeding success of the mothers in the experimental and control groups were evaluated. | Sociodemographic data form; Breastfeeding Self- efficacy Scale-Short form; LATCH Breastfeeding Diagnostic Scale | It was observed that mothers who received breastfeeding training in the last trimester of pregnancy had a higher perception of breastfeeding self-efficacy and breastfeeding success in the first week after delivery than mothers who did not. |
| Dilek Menekşe, Nursan Çinar (2018) (21) | Nursing; Doctorate | To evaluate the development of the breastfeeding intention scale in pregnant women with twins, test its validity and reliability, and assess the effect of breastfeeding education given in the antenatal period on the breastfeeding intention of pregnant women expecting twins | To develop scale: 105; experimental group: 38 | Methodological and experimental work is two-stage. First, the validity and reliability of the scale was determined. Then, 38 pregnant women in the experimental group were trained using visual education tools. | Introductory information form; breastfeeding intention scale in pregnant women expecting twins; fact sheet on breastfeeding of twin babies | It was determined that the developed scale is effective, and breastfeeding education given in the prenatal period affects breastfeeding intention. |
| Hamide Aygör, Emel Ege (2017) (22) | Nursing; Doctorate | Primiparous mothers, 36 - 40 days of pregnancy to determine the effect of breastfeeding counseling given from the gestational week until the first 6 months after birth on the duration of feeding with only breast milk, postpartum depression, and quality of life | Experiment: 32 pregnant; control: 32 pregnant | Semi-experimental; Pregnant women in the experimental group were given breastfeeding training and consultancy services, starting from the prenatal period. The control group received standard care. After the training given to the pregnant participants between 36 - 40 weeks, the first 24 hours of delivery and the first six months after delivery were evaluated. | Mother information form; baby information form; breastfeeding characteristics form; breastfeeding characteristics form II Edinburgh Postpartum Depression Scale; Postpartum Quality of Life Scale | 36 - 40 days of pregnancy to mothers. It has been determined that breastfeeding counseling given from the gestational week to the end of the sixth month after delivery prolongs the duration of feeding with only breast milk, reduces the risk of postpartum depression in mothers, and increases the quality of life. |
| Ayşe Güldür, Kerime Derya Beydağ (2016) (23) | Nursing; Master’s degree | To determine the postpartum breastfeeding behaviors and breastfeeding self-efficacy of pregnant women who received or did not receive breastfeeding education at the pregnant school during pregnancy | Experiment: 50; control: 50 | Cross-sectional quasi-experimental; The experimental group was given training on pregnancy, birth, breastfeeding, baby care, and puerperium during the pregnancy school for 5 weeks. No training was given to the control group. | Descriptive questionnaire on birth and breastfeeding; Postpartum Breastfeeding Self-efficacy Scale | Breastfeeding education given in pregnant schools was observed to be effective in breastfeeding behavior, breastfeeding practices, and breastfeeding self-efficacy in the postnatal period. It was observed that women who received the training were more willing to learn and practice. |
| Yeşim Yeşil, Hafize Öztürk Can (2015) (24) | Midwifery; Master’s degree | To evaluate the effect of individual and group breastfeeding education on breastfeeding self-efficacy and attitude in the postpartum period in mother and father candidates | Individual training: 30; group training: 30; control group: 30 | Educational intervention research; Research data were collected in four stages (after 37 weeks of pregnancy, in the first week after delivery, and in the sixth week and the fourth month after delivery). The data were collected by the face-to- face interview technique and telephone. Routine care services were given to the control group. | Introductory characteristics data form for mother and father candidates; Breastfeeding Self-efficacy Scale; Iowa Infant Feeding Attitude Scale | It was observed that breastfeeding education is not sufficient to develop self- efficacy and attitude, and it is necessary for mothers to be supported by health workers in the hospital after birth. In addition, it is recommended that fathers be included in breastfeeding education given during pregnancy. |
| Berrak Mizrak, Nebahat Özerdoğan (2013) (25) | Nursing; Master’s degree | To evaluate the effect of breastfeeding education given to primiparous pregnant women in the antenatal period on mothers’ perception of breastfeeding self-efficacy and success | Experiment: 45; control: 45 | Intervention research; The primiparous pregnant women in the study group were given interactive training by the researcher in groups of 5 - 6 individuals, lasting 120 - 150 minutes on average during the antenatal period. During the training, slides, models, and videos were used. The pregnant women in the control group were given standard breastfeeding training given by midwives/nurses in hospitals and family health centers. All participants were evaluated at 1, 4, and 8 weeks postpartum. | Antenatal period information form; postnatal period information form; Breastfeeding Self- efficacy-Short Form Scale (postnatal and antenatal form); LATCH Breastfeeding Diagnostic Measurement Tool | There was no difference in parameters such as height and weight in the babies of mothers in the experimental and control groups at the 1st, 4th and 8th weeks postpartum. There was no difference in parameters. However, it was determined that breastfeeding education given to pregnant women in the antenatal period to increase the perception of breastfeeding self-efficacy increases the perception of breastfeeding self-efficacy and breastfeeding success. |
| Fatma Gözükara, Lale Taşkin (2012) (26) | Nursing; Doctorate | To examine the effects of education and counseling services provided to parents on breastfeeding behavior | Intervention: 31 couples; control: 31 pairs | Intervention research. Prenatal breastfeeding training was given to the parents in the study group, and it was shown in practice on the model. In addition, counseling was provided within the first 48 hours after delivery. Evaluations were made at the 1st week, 2nd week, 1st month and 6th month. No training or counseling was given to the control group. | Introductory information form for expectant mothers; introductory information form for father candidates; postpartum information form; follow-up form to determine breastfeeding characteristics; Information form for mothers and fathers to determine the reasons for switching to complementary foods | In this study, it was determined that breastfeeding education and counseling provided to parents increased only breast milk (OBM) in the first 6 months. In addition, it was determined that the rate of giving SAS in the first 6 months increased as the frequency of follow-up increased during pregnancy. |
| Author, Consultant (Year) | Department; Postgraduate Level | Purpose of Research | Sample | Research Type/Method | Data Collection Tools | Conclusion |
|---|---|---|---|---|---|---|
| Yağmur Sezen Yilmaz, Nesrin Şen Celasin (2022) (27) | Nursing; Master’s degree | To examine the effect of breastfeeding education given in the mother-neonate adjustment room on breastfeeding self- efficacy of mothers with newborn babies | 101 mothers (whose neonates were in the neonatal intensive care unit) | Semi-experimental; The training on breast milk and breastfeeding was given one-on-one by the researcher for 45 - 60 minutes. Questionnaire forms were administered to the mothers 3 times (i.e., before education, after education, and 1 month after discharge). | Mother-baby information form; Postpartum Breastfeeding Self-efficacy Scale | It was determined that the mean scores of the mothers after discharge were higher than the mean scores after and before education. Therefore, it was observed that breastfeeding education given to mothers in the mother- neonate adjustment room was effective in breastfeeding self- efficacy levels. |
| Eda Özkan, Nevin Hotun Şahin (2022) (28) | Nursing; Master’s degree | To evaluate the effect of breastfeeding education given to fathers on the knowledge level and mothers on breastfeeding self-efficacy and breastfeeding attitude | Experiment: 80 families; control: 80 families | Semi-experimental; The “Breastfeeding Education for Fathers” initiative was applied to the fathers in the experimental group. The training was a 20-minute interactive training. A Breastfeeding Education Guide for Fathers was developed to be used in this training. The data were collected from all participants by face-to-face interviews. Participants were evaluated within the first 24 hours after birth and 1 month after birth. | Data collection form; The scale of fathers’ effect on breastfeeding; Fathers breastfeeding knowledge test; breastfeeding attitude rating scale; Postpartum Breastfeeding Self-efficacy Scale-short Form | It was determined that the breastfeeding knowledge test scores of the fathers in the experimental group were higher than those in the control group, and the fathers in the experimental group had a greater effect on breastfeeding. It can be concluded that the education given to fathers and the content of the education affect the breastfeeding process. |
| Gülsün Kocagöz Acar, Müge Seval (2021) (29) | Nursing; Master’s degree | To evaluate the effect of breastfeeding counseling given to mothers of preterm neonates in the postpartum period on breastfeeding perception and adequacy | Mothers with 100 preterm neonates | Single-group pretest- posttest design; In the mother-neonate adjustment room of the hospital, a training program was run by the researcher, including a slide show (30 minutes) and hands-on training (15 - 20 minutes). | Maternal information form; neonate information form; Postpartum Breastfeeding Self- efficacy Scale; adults’ perceptions of breast milk; LATCH Breastfeeding Diagnostic Measurement Tool; education evaluation form | As a result of the study, it was determined that education had a positive effect on the diagnosis of breastfeeding and breastfeeding self- efficacy, but negatively affected the perception of breast milk. |
| Sevda Korkut Öksüz, Sevil Inal (2021) (30) | Midwifery; Doctorate | To determine the effect of continuous breastfeeding support provided to mothers via the WhatsApp messaging application on breastfeeding | Experiment: 64; control: 65 | Experimental; In addition to routine breastfeeding training, mothers in the experimental group were given continuous breastfeeding training during the first 6 months of DS via WhatsApp messaging application after birth. Routine postpartum breastfeeding training was given to the control group. Follow-ups for both groups were carried out via telephone at postpartum 7th day, 15th day, 1st month, 2nd month, 4th month, and 6th month. | Mother and newborn data collection form; postpartum breastfeeding evaluation and follow-up form; breastfeeding problems rating scale; breastfeeding attitude rating scale; breastfeeding motivation scale; application satisfaction evaluation form | Continuous breastfeeding support given to mothers through WhatsApp messaging application increased the rate and duration of neonates receiving SAS, reduced the use of pacifiers and bottles, contributed to the mothers with fewer breastfeeding problems, and positively affected their breastfeeding attitudes and motivations. |
| Yeşim Yeşil, Hafize Öztürk Can (2020) (31) | Midwifery; Doctorate | Determining the validity and reliability of the Turkish version of the Postpartum Spousal Support Scale (PSSS) and Paternal Breastfeeding Self-Efficacy Scale, determining the effect of breastfeeding education given to parents in the early postpartum period on paternal breastfeeding self-efficacy and postpartum outcomes. | 200 mothers 200 fathers for the first stage; Second stage: Experiment: 76 Families; Control: 76 families for the second stage | It had 2 stages. First stage: Methodological type, second stage: Intervention research; In the first stage, the validity and reliability of Paternal Breastfeeding Self-efficacy Scale was evaluated. In the second stage, the parents in the experimental group were given theoretical and practical training in the hospital. The parents in the control group were not given breastfeeding education; they only benefited from routine hospital service. The scales were re- evaluated in both groups when they were followed up for 1 to 6 weeks. | Postpartum sociodemographic and breastfeeding status of the mothers questionnaire; postpartum spouse support scale; Parental Breastfeeding Self-efficacy Scale (1 to 6 weeks follow-up form for mothers); postpartum sociodemographic questionnaire for fathers; Paternal Breastfeeding Self-Efficacy Scale (PEAS); 1 week and 6 weeks follow-up form for fathers | It was determined that the education given to the parents in the early postpartum period increased the perception of postpartum spousal support in mothers and the perception of paternal breastfeeding self-efficacy in fathers. At the same time, it was also effective in mothers’ postpartum feeding behavior with only breast milk. |
| Zeliha Özge Özgüneş, Serap Balci (2019) (32) | Nursing; Master’s degree | To determine the effect of breastfeeding education given to mothers on successful breastfeeding | 33 newborns and their mothers | Single group pretest- posttest quasi- experimental; With the face-to-face interview technique, 30 - 45 minutes of training was given to the mothers by the researcher one-on-one. The scale was then evaluated, and re- evaluation was made on the 7th day after discharge. | Information form; LATCH Breastfeeding Diagnostic Scale | It was observed that the scores obtained by the mothers on the 7th postpartum day were higher than the scores they received on the 1st day. Therefore, it was determined that breastfeeding education given to mothers increases the success of breastfeeding. |
| Gülsoltan Aylyyeva, Serap Topatan (2019) (33) | Nursing; Master’s degree | To determine the effects of breastfeeding education and counseling given in the postpartum period on the knowledge levels of primiparous mothers about breast milk and the duration of feeding their neonates with only breast milk after birth | Experiment: 50; control: 50 | Pretest-posttest applied semi-experimental; The mothers in the experimental group were trained on breast milk and breastfeeding for 45 minutes (within postpartum 24 - 72 hours). After the first interview, all participants were re- evaluated at 1, 3, 4, and 6 months. | Survey form | It was determined that the breastfeeding knowledge scores of the mothers in the experimental group and the rates of giving SAS until the postpartum 6th month were higher than the control group. |
| Gülsün Ayran, Ayda Çelebioğlu (2018) (34) | Nursing; Doctorate | To determine the effect of breastfeeding education given to mothers and parents in the early postpartum period on mothers’ breastfeeding self- efficacy levels, the duration of feeding with exclusive breast milk in the first 6 months of neonates, and parent- neonate attachment | I. Experimental group: 49 (mother-father- neonate); II. Experimental group: 49 (mother-father- neonate); control group: 48 (mother-father- neonate) | Semi-experimental In the 1st experimental group, only the mothers and in the 2nd experimental group, the parents were trained together. Routine nursing services were provided to the families in the control group. The growth parameters of the neonates in all groups were evaluated up to the 6th month. | Mothers and fathers introductory information form; baby monitoring form; LATCH Breastfeeding Diagnostic and Evaluation Scale; Breastfeeding Self- efficacy Scale; father-neonate attachment scale; maternal attachment scale | It was determined that fathers’ participation in breastfeeding education affects the breastfeeding process, increases the breastfeeding self- efficacy level of mothers, and positively affects neonates’ feeding with SAS and father- neonate attachment. |
| Nazan Gürarslan Baş, Duygu Arikan (2014) (35) | Nursing; Doctorate | To determine the effect of breastfeeding counseling given to mothers who had cesarean section on the first breastfeeding time, body temperature, and sucking success of the newborn | Experiment: 45; control: 45 | Semi-experimental; A 1-hour breastfeeding counseling service was provided to the mothers in the experimental group before the cesarean section. Postpartum breastfeeding status and newborn body temperature were evaluated at 30 minutes, 4 hours, and 10 hours after birth. No attempt was made in the control group. | Personal information form; newborn evaluation form at birth; newborn evaluation form in the service; LATCH Breastfeeding Diagnostic Measurement Tool | It was determined that the breastfeeding consultancy service received shortens the time to start the first breastfeeding. As the first breastfeeding time gets shorter, the body temperature of the newborn increases and the sucking success of the newborn increases. |
| Emine Durmuş, Leman Kutlu (2019) (36) | Nursing; Master’s degree | To determine the effect of postpartum breastfeeding education on the mother’s attitude toward feeding her neonate, breastfeeding self-efficacy, and breastfeeding motivation | 80 puerperant women | Experimental; A 1-hour training program was applied to the participants by the researcher by performing the pretest and posttest. | Personal information form; Iowa Infant Feeding Attitude Scale; Breastfeeding Self-efficacy Scale; breastfeeding motivation scale | It was determined that breastfeeding education given to mothers in the first week after birth increases the perception of breastfeeding self-efficacy and breastfeeding motivation and affects neonates’ feeding behaviors. |
| Arzu Kul Uçtu, Nebahat Özerdoğan (2019) (37) | Midwifery; Doctorate | To evaluate the effect of breastfeeding education given using the teach-back method on breastfeeding success | Intervention group: 40; control group: 40 | Randomized-controlled experimental; The research consisted of 2 stages. The first stage was carried out in the hospital, and the second stage was carried out in the FHCs to which the women were affiliated. The mothers in the intervention group were given training and counseling services based on the teach- back method using the Breastfeeding Training Guide in 3 follow-ups at the FHCs they were affiliated with. The control group, on the other hand, was provided with standard education and counseling services on breastfeeding at the FHCs. | Introductory information collection form; LATCH Breastfeeding Diagnostic and Evaluation Scale; Breastfeeding Self-efficacy Scale-short Form; belief and confidence scale; Teach-Back Method Observation Tool | It was determined that breastfeeding education given using the Tell What You Have Learned method is more effective than the standard education technique that is routinely offered in increasing breastfeeding success and self-efficacy. |
Abbreviation: FHC, family health center
| Author, Consultant (Year) | Department Postgraduate Level | Purpose of Research | Sample | Research Type/Method | Data Collection Tools | Conclusion |
|---|---|---|---|---|---|---|
| Gamze Bayrak Başdağ, Engin Yurtçu (2021) (38) | Midwifery; Master’s degree | To evaluate breastfeeding self-efficacy and breastfeeding success of mothers who received breastfeeding training on the basis of the Health Belief Model in the postpartum period | 207 mothers | Educational intervention; Breastfeeding training was given to mothers during their stay in the hospital after delivery, and their breastfeeding was supported. The participants, whose information was obtained, were called again by the researcher one month later. | Survey form; Breastfeeding Self-efficacy Scale (postnatal version); LATCH Breastfeeding Diagnostic Scale | It was determined that breastfeeding education based on the Health Belief Model increases breastfeeding self-efficacy and breastfeeding success in mothers. |
| Gamze Durmazoğlu, Hülya Okumuş (2020) (39) | Nursing; Doctorate | To examine the effects of breastfeeding education based on Human Care Theory on mothers’ perception of breastfeeding self-efficacy, breastfeeding duration, breastfeeding style, and their satisfaction with this training process | Experiment: 50; control: 50 | Experimental study with education initiative; In the first stage of the study, pregnant women in the experimental group (n=50) were given Human Care Theory (HCT) based training, and those in the control group (n = 50) were given standard face-to-face training. In the second stage, based online training was given to the experimental group. The experimental group was given continuous telephone counseling, and the control group was given telephone counseling when they needed it. | Introductory features questionnaire; baby’s nutritional status evaluation form; Breastfeeding Self-efficacy Scale-short Form; satisfaction evaluation form for Human Care Theory’s improvement processes | It was concluded that the experimental group experienced fewer breastfeeding problems than the control group, and the neonates were breastfed more frequently during the day and night. It was determined that the breastfeeding education program based on HCT has a positive effect on breastfeeding outcomes. |
| Hamide Arslan, Gönül Kurt (2020) (40) | Nursing; Master’s degree | To determine the effect of applied breastfeeding education given in the antenatal period with the Lactation Simulation Model on breastfeeding success, breastfeeding self-efficacy perception and attitudes, and knowledge of women in the postnatal period | Experiment: 64; control: 64 | Experimental-applied; Breastfeeding training with the Lactation Simulation Model during the antenatal period (simulation training group) was given to pregnant women in the experimental group, and the standard video-educational demonstration (video training group) was provided for the pregnant women in the control group within the scope of hospital protocol. | Participant diagnosis form; LATCH Breastfeeding Diagnosis and Evaluation Scale; attitude and knowledge evaluation form regarding breastfeeding; Breastfeeding Self-efficacy Scale; postnatal period follow-up form | It was determined that women who were given simulation-based breastfeeding training after the training had higher breastfeeding success in both the first and second follow-ups than the women who were given video training. It was determined that women who received simulation-based training had higher breastfeeding self-efficacy and knowledge levels. |
| Pınar Akgün, Ayşe Koyun (2019)(41) | Nursing; Master’s degree | To examine the effects of knowledge, motivation, and behavioral skills on breastfeeding success in a hypothetical model | 229 breastfeeding women | Pretest-posttest semi-experimental; The study was performed in 2 stages. In the first stage, mothers’ knowledge, motivation, and behavioral skills were evaluated and tested with a hypothetical model. Breastfeeding education was given to the intervention group in 2 stages. The questionnaires were re-evaluated before the training and 4 weeks after the training. | Survey form; Breastfeeding Self-efficacy Scale; breastfeeding support scale; breastfeeding attitude assessment scale; breastfeeding success observation form | Education based on the Knowledge, Motivation and Behavioral Skills (KMB) model positively contributes to breastfeeding success by influencing mothers’ motivation for breastfeeding, behavioral skills, self-management behaviors, and health outcomes. |
| Rukiye Çelik, Ebru Kiliçarslan Törüner (2018) (42) | Nursing; Master’s degree | To examine the effect of technology-based breastfeeding program on the growth of neonates of adolescent mothers | Experiment: 16; control: 16 | Experimental; An 8-week program was applied to the adolescent mothers in the experimental group (face-to-face training in the first week, planned phone calls made about breastfeeding in the 2nd, 3rd, and 6th weeks, and text messages sent every week). The mothers in the control group were given routine care in the family health center. | Descriptive data form; baby’s physical development and breastfeeding follow-up form; Postpartum Breastfeeding Self-efficacy Scale; Spielberger State Anxiety Inventory; LATCH Tool; breastfeeding program evaluation form | LATCH, self-efficacy, and anxiety scores of the adolescent mothers in the experimental and control groups (1st follow-up) were observed to be similar. In the third follow-up, the adolescent mothers in the experimental group had higher self-efficacy scores and lower state anxiety scores than those in the control group. |
3.1. Breastfeeding Education in the Antenatal Period
There were 10 studies that met the inclusion criteria within 2012 - 2022 on breastfeeding education in the antenatal period. In the prenatal period, mothers and fathers can be provided individually or in groups at the hospital, home, and the pregnant school with breastfeeding education. It is stated that women who receive breastfeeding training at the pregnant school are more willing to learn and practice than those who do not (23), and those who receive the training in the last trimester of pregnancy have a higher perception of breastfeeding self-efficacy and breastfeeding success after delivery (18). It was determined that prenatal education given to primiparous and nulliparous pregnant women increases the perception of breastfeeding self-efficacy and positively affects breastfeeding success (20, 25). In the theses, it was determined that the individual education of the mothers was more effective. In general, mothers and fathers who received breastfeeding training were observed to have a higher perception of breastfeeding self-efficacy than those who did not (24, 26). In studies that base education on a model and theory, it is stated that the self-efficacy perception, knowledge, and breastfeeding success of postnatal breastfeeding is higher than the video group of pregnant women who received training with the lactation simulation model (40). The Human Care Theory emphasizes that pregnant women who receive training have fewer breastfeeding problems after birth, and mothers breastfeed their neonates more frequently (Tables 2 and 4) (39).
3.2. Breastfeeding Education in the Postnatal Period
According to the inclusion criteria of the systematic review within 2012 - 2022 on breastfeeding education in the postpartum period, 14 theses were obtained. Training in issues, such as breastfeeding, breast milk, and the postpartum period, both individually and in groups, was given to mothers and fathers in the postpartum period, and its effectiveness was evaluated in the prenatal period. It was shown that mothers whose neonates were in the intensive care unit and who received training in the mother-neonate adjustment room have a higher perception of breastfeeding self-efficacy (27). Breastfeeding education given to fathers affects their attitudes and knowledge toward breastfeeding, and their knowledge level is higher than those who do not receive education (28). It was determined that breastfeeding education, which is given using the tell me what you have learned method as a training technique, is more effective in breastfeeding success and self-efficacy than the standard education technique routinely offered (37).
There are also studies examining the time of giving postpartum education and its effectiveness. For example, it is stated that the education given to mothers and fathers in the early postpartum period increases mothers’ perception of breastfeeding self-efficacy. Fathers’ participation in education affects the breastfeeding process and neonates’ feeding with OBM and positively increases neonate-father attachment (34). It has been determined that the education given to the parents increases the perception of postpartum spousal support in mothers (31); nevertheless, the education given to mothers giving birth for the first time increases the rate of giving OBM to neonates in the first 6 months after birth (33). It was determined that mothers who received training in the first week after birth had better breastfeeding motivation and a higher perception of breastfeeding self-efficacy (36).
In studies examining the effect of the mode of delivery on the breastfeeding process, it was determined that the education given to mothers who gave birth by cesarean section shortens the time to start breastfeeding and increases the sucking success of the newborn (35). It was determined that continuous breastfeeding training and counseling given to mothers for the first 6 months after birth causes them to experience fewer breastfeeding problems than those who do not, reduce the use of pacifiers and bottles, increase the rate of breastfeeding, and positively affect mothers’ motivation to breastfeed (30). In studies that base education on a model and theory, according to the Health Belief Model, mothers who received breastfeeding training had higher breastfeeding success (38). In technology-based breastfeeding training, the adolescent mothers in the experimental group had higher breastfeeding self-efficacy scores and lower anxiety levels after the training (Tables 3 and 4) (42).
4. Discussion
In this systematic review, it was determined that breastfeeding education given to pregnant women, puerperant women, and fathers, 10 prenatal and 14 postnatal, increased breastfeeding success and breastfeeding self-efficacy. The training consists of subjects, such as pregnancy, birth, breastfeeding, neonatal care, and puerperium. Breastfeeding training is very effective in improving breastfeeding skills and increasing breastfeeding success (43, 44). In order to initiate and maintain effective breastfeeding, women should be supported by their spouses, families, health systems, and society, starting from the pregnancy period, and their motivation for breastfeeding should be increased (45, 46).
Numerous studies in the literature stated that providing education in the antenatal period increases breastfeeding self-efficacy (25, 47, 48). In studies conducted by many researchers such as Öztürk, Güldür and Mizrak, participants in the experimental group were given prenatal individual and group trainings and it was determined that those who participated in postnatal training had higher breastfeeding self-efficacy (Table 2) (18, 23, 25). However, there are also studies that state that postnatal education is more effective. For example, in a study by Abuidhail et al., it was shown that postnatal education increased breastfeeding self-efficacy more than prenatal education (49).
In this systematic review, brochures, training booklets, slides, videos, models, and simulation programs were used as training techniques. However, evidence-based guidelines state that practical training is more effective in supporting breastfeeding (50, 51). Arslan observed that women who were given simulation-based breastfeeding training had higher breastfeeding success than women who were given video training (Table 4) (40). In another study, one-on-one breastfeeding training was provided using a brochure; nevertheless, the other group was only given verbal training. As a result of the study, it was determined that the success of breastfeeding in the first 24 hours after birth was higher in those who received one-on-one training (52). In a study by Uçtu, it was determined that the education given using the tell me what you have learned method was more effective than the standard training technique routinely performed in increasing breastfeeding success and self-efficacy (37). The training was presented to the participants individually and in groups.
In Gözükara’s study, parents were given training together, and it was determined that the education increased the rate of giving OBM in the first 6 months (Table 2) (26). Özkan, on the other hand, provided training to fathers interactively and determined that those who received training had a greater effect on the breastfeeding process (Table 3) (28). In a study by Kim et al., individual and group breastfeeding education was given in the prenatal period, and no significant difference was noticed between the two groups that were tested before education; however, it was stated that those who received individual training after birth had better knowledge of breastfeeding (53).
In addition to mothers, fathers should be included in breastfeeding education. Because when mothers’ support systems are strong and their spouses exhibit positive behaviors toward breastfeeding, it was observed that mothers start breastfeeding earlier and continue for a longer period of time (54). In an educational randomized controlled intervention study by Sciacca et al., participants attended the classes with incentives (55). As a result of the study, it was determined that the incidence and duration of breastfeeding were higher and longer in women who participated in the training with their spouses than those who did not (55). In a study by Henshaw et al., it was determined that the transition to fatherhood became easier due to the increase in the knowledge level of the fathers who participated in the education, and it increased the adaptation (56). In a systematic review, Ayran showed that fathers’ participation in breastfeeding education affected the breastfeeding process and increased mothers’ perception of breastfeeding self-efficacy (Table 3) (34).
Successful breastfeeding experience in the postpartum period increases the quality of life by ensuring that mothers are healthy (57, 58). Therefore, mothers and their spouses should be supported in breastfeeding, starting from the prenatal period and continuing to the postpartum period. Pregnant women should be encouraged about the importance of prenatal follow-up and participation in the pregnant school.
4.1. Limitations of the Study
Theses that were not included in the YÖK database and were not registered in the system could not be obtained. The limitations of the study were that the search was only in the field of midwifery/nursing, the same theses were obtained with different keywords, and the number of the studied theses was low.
4.2. Conclusions
Breastfeeding education, breastfeeding success and breastfeeding self-efficacy is a method that ensures and supports the continuity of the physical, mental and psychological well-being of mothers by affecting the rate of breastfeeding in the first 6 months. It is a method that provides and supports the continuity of the physical, mental, and psychological well-being of mothers. Midwives and nurses, on the other hand, should support pregnant women and parents in breastfeeding using their many roles and functions, such as caregiver, decision-maker, and patient rights advocate, and provide training by following the algorithms in the light of up-to-date information according to the needs of the participants.