1. Background
Nurse-physician collaboration is essential for providing effective patient care. Professional collaboration means that two or more individuals with specialized knowledge, and specific roles, perform interdependent tasks and share a common goal, such as safe care for patients (1). Intensive care units provide critical care services for patients, and effective collaboration between nurses and physicians is even more important in these specialized wards (2).
Many studies show teamwork improves patient safety and prevents medical errors (3, 4). Effective teamwork also decreases mortality, nosocomial infection, need for ventilators, re-admission, and length of stay in ICUs (3, 5, 6). Patients are not the only ones who benefit. Teamwork can increase occupational well-being and job satisfaction and decrease clinician burnout (7-9).
In spite of the importance of nurse-physician collaboration, this issue might not be satisfied all the time. A study in ICUs in Texas showed that only 33% of nurses rated the quality of collaboration and communication with the physicians as high or very high, but 73% of physicians reported the collaboration as high or very high that showing a great discrepant attitude (10). In Iran, the nurse-physician professional relationship was moderate from the nurses' point of view, and 66% noted that they were respected by physicians (11). According to the studies, some different barriers and challenges limit inter-professional collaboration. The inability to build a professional relationship, selfishness, lack of mutual respect, and job pressures are some barriers to effective collaboration (12-15). A study in Iran in 2010 showed that personal conflicts, an embarrassment in requesting help or asking questions and being unaware of other professional roles and capabilities could threaten teamwork (16). Another study in Iran in 2015 showed that inadequate support the hospital management and weak leadership could diminish teamwork (17). Several studies have reported different barriers to nurse-physician collaboration, but nurses' viewpoints as professionals have not been investigated. Understanding different perspectives are important because these perspectives shape behaviors (18). Nurse-physician collaboration is a social and professional phenomenon, so understanding the nurses' viewpoints might help illuminate this crucial subject.
2. Objectives
This research aimed to study different viewpoints of nurses working in ICUs about the barriers to nurse-physician collaboration with Q methodology.
3. Methods
3.1. Design and Setting of the Study
This cross-sectional study that employed a Q-methodology approach was carried out from April to November 2020 in the general hospital of Kashan city. This hospital has 4 ICUs with 48 beds and 113 nursing personnel. Fourteen specialists provide medical treatments in ICUs, including anesthetics, surgeons, internists, cardiologists, and intensivists.
Q-methodology was first introduced by William Stephenson in 1935 (19). It is an approach for identifying and comparing individuals' viewpoints. In the Q methodology, the participants (P-sample) sort their viewpoints (Q-sorting) by ranking a set of statements (Q-statements) about a particular issue (18). Once the sorting is completed, the factor analysis is performed (20). The analysis tries to identify patterns of similarity and differences in how participants have ranked the statements according to their perceived agreement or importance. The factors that emerge as the common viewpoints of participants are interpreted qualitatively (18). The Q methodology is a proper method for investigating the different opinions about a subject (21).
This study was conducted in 6 stages according to the Q methodology phases:
Stage 1- develop the Q-statements: This means collecting statements that cover discrete ideas and concepts of the topic (22). This step aimed to find the barriers to nurse-physician collaboration in the literature. All the published articles in English and Persian about the barriers to collaboration in different settings from 2000 until the end of 2020 were collected. The research type could be both descriptive and interventional. The keywords of nurse, physician, nurse-physician, barriers, and collaboration and their synonyms were searched in PubMed, Embase, Scopus, SID, Google scholar, and Magiran. One thousand three hundred thirty-eight articles were probed in the first search, and after excluding duplicate and unrelated articles, the abstract of 112 articles was reviewed, and the statements that could represent a barrier were written. The articles were managed by EndNote X8 software.
The 56 statements were extracted from the literature, then 25 statements were omitted by researchers because they had similar content. So 31 items were piloted.
Stage 2- piloting: The comprehensibility of the statements and instructions and how easily participants can sort the statements are ensured at this stage (18). In this study, ten nursing and intensive care experts evaluated the statements. In order to reduce the researcher bias in selecting the statements, the experts were requested to revise the statements or add new ones if they thought the statements could not cover the subject adequately. The qualitative content analysis and quantitative content analysis, including content validity index (CVI) and content validity ratio (CVR), also were calculated (23). After deleting and revising the statements according to the views of experts, 24 items remained as Q-statements. The CVR and CVI scores of the statements were calculated at 0.718 and 0.972, respectively, which showed acceptable content validity.
Stage 3- participant selection (P-sample): Use purposive sampling to recruit participants who can articulate viewpoints on the topic because their opinions are important (22). The 30 nurses and nursing faculty members working or providing education in ICUs were invited to sort the statements. The participants in the study were recruited to reflect the diversity of age, gender, education, and work experience and were willing to participate in the study to represent different viewpoints. The inclusion criteria were at least two years of work experience in ICUs, a bachelor's degree in nursing, and a willingness to participate in the study. It is suggested that a 2:1 ratio of statements to participants is needed in the Q-methodology at a minimum (19). So the 30 participants seem to be adequate in this study.
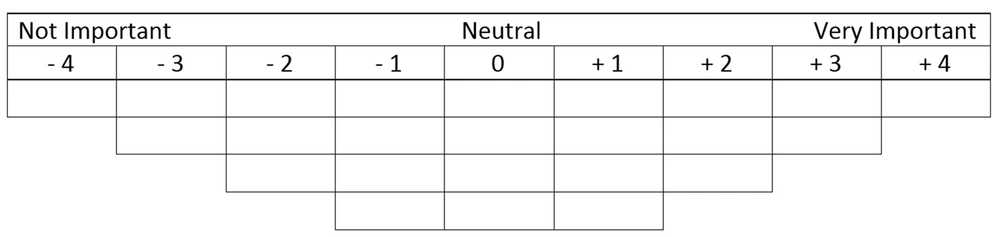
Stage 4- data collection: Statements were written on similar cards, and participants sorted them (Q-sorting) according to some level of judgment (18). For the Q-sorting process, a forced distribution was chosen on a scale from -4 to +4 (not important to most important), as seen in Figure 1. During sorting, the participants were questioned about why they think a statement is not important or it is very important, and their answers were recorded to help the researchers in the interpretation stage. The demographic variables of each respondent and the number of each statement according to his/her Q-sorting were recorded.
Stage 5- analysis: Factor analysis is a statistical method for classifying participants according to their views (22). The data were analyzed with PQMethod 2.35 software. The centroid factor analysis and varimax rotation were used for data analysis. Factors were extracted using the following criteria: The total amount of variability explained, at least two Q-sorts per factor, and the eigenvalues greater than 1. According to the analysis results, the corresponding people for each extraction factor in the Q methodology were grouped and classified. These people had similar views about the barriers to nurse-physician collaboration in ICUs. Since the number of statements was 24, a factor loading more than 0.4 was accepted.
Stage 6- interpretation: Qualitative interpretation of the viewpoints according to the most negative and positive statements in every factor and developing narratives for each factor representing a viewpoint (18). In this study, the participants with similar opinions were grouped as a factor. The most and less important and distinguishing statements for every factor were interpreted qualitatively, and narrative explanations were provided for every factor. Distinguishing statements are statements that rank in a position that significantly differs from the rank in other factors.
3.2. Ethical Considerations
The research protocol was independently reviewed and approved by the ethics committee of Kashan University of Medical Sciences with the ethical code of IR.KAUMS.NUHEPM.REC.1398.039. The research objectives were explained to all participants, and written informed consent was obtained. The confidentiality of the participants and their views were respected. The participants had the right to leave the study at any time. This research has been conducted following the Declaration of Helsinki's ethical principles.
4. Results
Table 1 summarizes the participants' characteristics. The data analysis resulted in four factors of opinion groups that could explain 52.95% of the variance. The categories of viewpoints were: (1) different professional interests and lack of trust between nurses and physicians; (2) goal confusion; (3) systemic barriers to collaboration; and (4) personal differences.
| Participants Characteristics | Mean ± SD | Minimum | Maximum |
|---|---|---|---|
| Age | 36.83 ± 6.85 | 25 | 50 |
| Work experience | 13.6 ± 6.88 | 3 | 28 |
| Sex, No. (%) | |||
| Male | 16 (53.3) | ||
| Female | 14 (46.7) |
The Characteristics of the Participants
The factor loadings for each participant are presented in Table 2. Five participants didn't classify to any viewpoints because of factor loading less than 0.4 or cross-loading between factors.
| Participant | Sex | Age | Viewpoint 1: Different Professional Interests | Viewpoint 2: Goal Confusion | Viewpoint 3: Systemic Barriers in Collaboration | Viewpoint 4: Personal Differences |
|---|---|---|---|---|---|---|
| 1 | Male | 25 | 0.21 | 0.17 | -0.03 | 0.74 a |
| 2 | Male | 33 | 0.10 | 0.18 | 0.8 a | 0.19 |
| 3 | Female | 38 | 0.28 | 0.34 | -0.07 | 0.62 a |
| 4 | Male | 30 | 0.66 a | 0.36 | 0.25 | -0.25 |
| 5 | Female | 30 | 0.40 | 0.37 | -0.01 | 0.59 |
| 6 | Male | 35 | 0.50 | 0.43 | 0.08 | 0.26 |
| 7 | Male | 40 | 0.09 | 0.10 | -0.03 | 0.62 a |
| 8 | Female | 26 | 0.46 a | 0.19 | 0.23 | 0.22 |
| 9 | Female | 35 | 0.27 | -0.13 | 0.22 | 0.57 a |
| 10 | Male | 40 | 0.02 | 0.76 a | 0.03 | 0.15 |
| 11 | Female | 45 | 0.43 a | 0.26 | 0.24 | 0.33 |
| 12 | Female | 38 | 0.17 | -0.15 | 0.66 a | 0.29 |
| 13 | Male | 28 | 0.27 | 0.38 | 0.51 a | 0.29 |
| 14 | Female | 48 | 0.13 | 0.67 a | 0.13 | 0.38 |
| 15 | Female | 35 | 0.72 a | 0.31 | -0.19 | 0.12 |
| 16 | Male | 32 | 0.69 a | -0.09 | 0.31 | 0.21 |
| 17 | Male | 39 | 0.75 a | -0.05 | -0.14 | 0.32 |
| 18 | Female | 30 | 0.63 a | 0.24 | 0.17 | 0.39 |
| 19 | Male | 45 | 0.72 a | 0.01 | -0.02 | 0.01 |
| 20 | Male | 38 | 0.13 | 0.05 | 0.26 | 0.65 a |
| 21 | Female | 29 | 0.41 a | -0.02 | 0.06 | 0.31 |
| 22 | Female | 50 | 0.56 a | -0.08 | -0.21 | 0.45 |
| 23 | Male | 40 | 0.11 | 0.37 | 0.00 | 0.30 |
| 24 | Male | 35 | -0.15 | 0.03 | -0.38 | 0.32 |
| 25 | Female | 44 | 0.21 | 0.44 a | -0.16 | -0.28 |
| 26 | Male | 30 | 0.26 | 0.06 | -0.66 a | 0.21 |
| 27 | Female | 43 | 0.17 | 0.34 | -0.27 | 0.06 |
| 28 | Male | 39 | 0.05 | 0.70 a | -0.10 | -0.02 |
| 29 | Male | 27 | -0.41 | 0.67 a | 0.08 | 0.28 |
| 30 | Female | 46 | 0.10 | 0.89 a | 0.17 | -0.05 |
Factor Loading and Characters of the Participants
There was no correlation between factors that shows each can represent a viewpoint. Q-statements and their corresponding rank values for four factors are presented in Table 3.
| No | Statements | Viewpoint 1: Different Professional Interests | Viewpoint 2: Goal Confusion | Viewpoint 3: Systemic Barriers in Collaboration | Viewpoint 4: Personal Differences |
|---|---|---|---|---|---|
| 1 | Nurses and physicians are not interested in collaborating with each other | +3 a | +2 a | 0 | +1 |
| 2 | Nurses and physicians are in different hierarchies, and they have different perspectives | +1 | +4 a | 0 | 0 |
| 3 | Nurses and physicians have different beliefs and religious attitudes | +1 | -1 | -3 a | +4 a |
| 4 | Nurses and physicians are not trusting each other | +2 a | -2 | +1 | +1 |
| 5 | There are cultural differences between physicians and nurses | -1 | 0 | -2 | -2 |
| 6 | Nurses are afraid that their honor might not be respected by physicians | 0 | -2 a | +1 | +2 |
| 7 | Nurses and physicians have little experience in collaboration | +2 | -1 | +2 | -4 a |
| 8 | There is a lack of planning and education for teamwork | -2 | +2 | +3 a | +2 |
| 9 | Physicians and nurses have different interests | +4 a | 0 | +1 | -3 a |
| 10 | Physicians don’t like to collaborate with nurses | 0 | +1 | -2 | +3 a |
| 11 | Physicians stay in ICU for the short time | +3 a | 0 | -1 | -1 |
| 12 | Physicians receive more support from management than nurses | -1 | +1 | +2 a | +1 |
| 13 | There are serious shortages in the number of nurses and physicians | +1 | +3 a | +1 | -2 |
| 14 | There are personal conflicts between nurses and physicians | -2 | -2 | -3 a | +3 a |
| 15 | Nurses and physicians have a huge difference in incomes | +1 | +1 | +2 | +2 a |
| 16 | Nurses and physicians don’t have shared goals | 0 | +3 a | -1 | 0 |
| 17 | There are rigid hierarchy in hospitals | -3 a | +2 | -2 | 0 |
| 18 | Physicians don't like to hear the comments of nurses, even if they are right | -4 a | -1 | +3 a | -1 |
| 19 | Physicians are afraid that nurses might make their decisions under question | -1 | -4 a | -1 | -2 |
| 20 | Nurses and physicians don’t respect each other | +2 | -3 a | 0 | -1 |
| 21 | Nurses and physicians don't have adequate self-esteem | -1 | +1 | -4 a | -3 a |
| 22 | There is a lack of collaborative culture in ICUs | -2 | -1 | +4 a | +1 |
| 23 | Teamwork is not considered important in ICUs | 0 | -3 a | -1 | -1 |
| 24 | The health care services are not patient-centered in ICUs | -3 a | 0 | 0 | 0 |
Q-Statements and Their Corresponding Rank Values for Four Factors About Different Viewpoints in Nurse-Physician Collaboration Barriers
Note: The number in the crusher represents the number of the statement in Table 3.
Viewpoint 1- different professional interests and lack of trust between nurses and physicians: Ten participants made this viewpoint (Table 4). The participants in this viewpoint believed that nurses and physicians have different professional interests [9]; for example, physicians like to discharge patients as soon as possible to have an empty bed for a new patient, but nurses prefer to discharge patients in more stable conditions. Besides, based on nurses' perceptions, both professions are not interested in collaboration [1] and do not trust each other [4]. Some believe doctors do not trust nurses and think they do not have enough education, and nurses do not trust physicians and think that physicians do not spend enough time assessing patients. These are the main barriers to nurse-physician collaboration. Nurses in this view also believed that physicians stay in ICUs for a very short time [11], and they hardly see each other, so this inadequate time does not provide a context for collaboration.
| Variables | Viewpoint 1: Different Professional Interests | Viewpoint 2: Goal Confusion | Viewpoint 3: Systemic Barriers in Collaboration | Viewpoint 4: Personal Differences |
|---|---|---|---|---|
| Number of participants | 10 | 6 | 4 | 5 |
| Age | 36.1 ± 8.2 | 40.6 ± 7.5 | 32.25 ± 4.3 | 35.2 ± 6 |
| Work experience | 13.2 ± 8.6 | 16.3 ± 7.5 | 9 ± 4.5 | 12.8 ± 5.9 |
| Sex | ||||
| Male | 4 | 3 | 3 | 3 |
| Female | 6 | 3 | 1 | 2 |
| Eigenvalue | 8.03 | 3.22 | 2.45 | 2.17 |
| Variance | 26.77 | 10.74 | 8.17 | 7.25 |
| Some key statements | Different interests [9]; not interested in collaboration [1]; not trusting each other [4] | Different perspectives [2]; don’t have shared goals [16] | Lack of collaborative culture [22]; inadequate education for teamwork [8] | Different beliefs and attitudes [3]; personal conflicts [14]; the difference in incomes [15] |
Viewpoints of Barriers in Nurse-Physician Collaboration
On the other hand, these participants believed that the hierarchical culture in hospitals that physicians are at the top of that hierarchy [2], and is not an important barrier to collaboration. They also believed the sentence that ICU health care services was not patient-centered [24] were unrelated to nurse-physician collaboration. They did not feel that physicians were reluctant to hear nurses' comments [18], and they thought this was not a barrier to collaboration.
Viewpoint 2- goal confusion: This viewpoint was made by 6 participants (Table 4). Participants in this viewpoint believed that there is a hierarchical culture in hospitals [2], that physicians are at the top, and hierarchy differences can diminish collaborative interactions. These two professions have goal confusion [16]. Nurses do not know the trend and objectives of the treatments by physicians, and physicians do not know the objectives of nursing care. Each profession does its tasks separately, so nurse-physician collaboration does not happen adequately. In some cases, this problem is reflected in medication errors, where nurses are using the wrong medication or the wrong dosage because they do not communicate adequately with physicians who have ordered the medication. Besides, there are shortages of nurses and physicians in ICUs [13], so they should provide services for numerous patients and do not have adequate time for communication. This is the reason that they prefer to follow their tasks separately.
Nurses in this viewpoint believe that physicians are not afraid that nurses will criticize their decisions [19], and these two professions have mutual respect for each other [20], and both believe that teamwork is important [23]. Therefore, these issues are not the main problems of collaboration.
Viewpoint 3- systemic barriers in collaboration: Four participants (3 males and one female) shared this viewpoint (Table 4). The participants in this viewpoint thought there was a lack of collaborative culture in ICUs [22], and the physicians and nurses didn't receive education for teamwork [8]. Teamwork doesn't have a place in planning. Besides, physicians receive more support from the system [12], which limits the context of collaboration, and this might make physicians not pay adequate attention to the nurses' comments even when they are right [18].
These nurses think that not having self-esteem [21] and personal conflicts between nurses and physicians [14], or different religious beliefs and attitudes [3] are not important barriers to nurse-physician collaboration.
Viewpoint 4- personal differences: This viewpoint shares the opinions of 5 participants (Table 4). The participants in this viewpoint thought there were personal differences between nurses and physicians [14]. Their income is considerably different [15], so their social class, hobbies, and living conditions are different, and this will separate their religious and social attitudes [3]. These differences lead to personal conflicts between these two professions [14], and most doctors dislike collaborating with nurses [10].
On the opposite side, the lack of experience in collaboration [7], not having adequate self-esteem [21], and having different interests [9] are not important issues in nurse-physician collaboration.
5. Discussion
The current study found that nurses working in ICUs have different viewpoints about barriers to nurse-physician collaboration. Some believe that these two professionals have different interests, and there is a lack of trust between them. Mutual trust is important for communication and collaboration (24). A study by Aghamohammadi et al. in 2018 in Iran showed that the dominance of physicians and considering nurses as their assistants and not their colleagues could negatively influence nurse-physician collaboration (25). Nurses and physicians often do not appreciate the role of each other; they view collaboration differently; doctors view collaboration as following their orders, while nurses seek a more active role (26).
Some participants noted that nurses and physicians have different hierarchies and different perspectives. They have different goals and prefer to do their tasks separately.
The flow of information is not usually effective between healthcare providers with different academic degrees and hierarchies, such as nurses and physicians. This might cause a problem with teamwork (27). Nurse-physician collaboration is not just working together in a common environment; effective teamwork needs shared goals (25). A qualitative content analysis done by Kvande et al. in intensive care units in Norway in 2013 showed that the establishment of shared goals and clinical understanding, open dialogue, and willingness to listen to each other were the main factors in nurse-physician communication (28). Nygren et al. in Sweden in 2018 showed that the vast majority of nurses reported that teamwork toward shared goals, equal relationships within the team, and efficient organization were the prerequisites for inter-professional teamwork (29).
The present study showed that some nurses prioritized systemic barriers, such as a lack of collaborative culture in ICUs and not paying attention to teamwork in planning and education. These nurses were younger and had less work experience. This might give them the benefit of looking at the issue deeper. A study showed a significant negative correlation between age and overall attitude in teamwork (30). Inadequate education was one of the barriers that were distinguished in this viewpoint. Critical care nurses and physicians may benefit from training in conflict resolution, listening skills, and conducting collaborative rounds (10). Ballangrud et al. in Norway in 2016 showed that team training programs affect the teamwork behavior and communication of nurses and physicians in the surgical ward (31). The imbalance between the willingness to collaborate versus the desire to maintain autonomy is another systemic barrier to effective inter-professional collaboration (32). These are important systemic factors that can influence teamwork culture.
Some nurses thought that personal differences such as differences in beliefs and religious attitudes, differences in income, and personal conflicts between professionals were the most important barriers to nurse-physician collaboration. In Ethiopia, religion could affect nurse-physician inter-professional collaboration (33). A study by Mazdaki et al. in Iran in 2016 showed that physician specialist income was ten times more than nurses. This ratio was 2.3 in England and 3.3 in Turkey (34). This huge difference in income in Iran compared to other countries might make some nurses skeptical about nurse-physician collaboration. A study by Hailu et al. in Ethiopia in 2014 reported that the salary of nurses was a significant predictor of perceived respect and satisfaction with nurse-physician communication in patient care (35). These differences might have a role in unproductive nurse-physician collaboration.
This study had some limitations. The statements about collaboration barriers could be expanded if a qualitative study had been done before this cross-sectional study. Therefore, we recommend this subject for further study. This research is limited to nurses' viewpoints about the barriers to nurse-physician collaboration. The views of physicians can complete the picture, so we suggest investigating the views of physicians in future studies using Q-methodology.
5.1. Conclusions
We concluded that there are different perspectives among nurses about this important issue that were named as different interests and lack of trust between nurses and physicians, goal confusion, systemic barriers to collaboration, and personal differences. These barriers need different strategies and solutions, such as education, defining shared goals, enhancing collaborative culture, and reaching mutual respect and understanding. Improving teamwork is essential for patient safety and providing a healthy work environment.