1. Background
Cancer is an uncontrolled proliferation of cells that can lead to the formation of malignant neoplasm. Despite numerous advances in medical science to control and treat chronic diseases, unfortunately, cancer is still life-threatening for many societies (1). Regarding the effectiveness of psychological interventions on parents of children with cancer, the study by Zinivand et al. (2) showed that teaching positive thinking and optimism had a significant effect on reducing the anxiety level of parents of children with cancer aged 3 to 7 years (2-4).
Owing to the prevalence of cancer at different ages, it is the second leading cause of child death in developing countries, among which leukemia is the most common type in them (5). However, owing to the dramatic growth in the treatment of childhood cancers, the survival rate of all types of child cancers such as leukemia, brain, and nervous system tumors has increased by 79% (6). Cancer in children is different from adults, so that it has a better prognosis with timely diagnosis. The related effects on the psychological status of caregivers are not less than the effect it has on children.
In addition to physical stress, the caregiver endures severe psychological distress, including anger, depression, fatigue, withdrawal and social isolation, depression, and lack of self-control (7). The role of mothers as the primary caregiver is of great importance since they face many problems due to the change in the role of parents.
Increased remission, the tendency for short-term hospitalization, and outpatient treatment, as well as home care treatments, put a lot of pressure on mothers so that caregivers are referred to as secret patients (8). Experiencing negative emotions such as depression, anxiety, stress, anger, hatred, jealousy, etc., has always been a problem for humans. These negative styles of emotion (e.g., anxiety, depression, and hostility) have long been considered acceptable predictors of increased risk of morbidity and mortality, and cognitive-emotional interventions empower individuals against the mental stresses they may encounter (9).
Previously, most studies such as those conducted in Iran, e.g., the studies of Lotfi Kashani et al. (1, 7) and Baratian et al. (10), have focused on reducing negative psychological reactions and enhancing the quality of life of parents of children with cancer. However, according to the results of various studies such as Roepka (11), Ramos et al. (12), and Hamidian et al. (13), not only designing and applying interventions can reduce negative psychological consequences such as stress and depression but also it can promote post-traumatic growth in cancer patients and other traumas.
The ability of parents to provide care and support for children depends on their ability to cope with the stresses associated with the diagnosis and therapeutic consequences of this severe illness. Since parents are one of the primary sources of emotional and caring support for children with cancer, providing effective psychological care to parents of children with cancer can help them maintain and enhance their physical and psychological health by making the right and quick decisions in the face of child illness, and this leads to the provision of more psychological support (14, 15).
Because mothers are more involved in the process of their children’s illness than fathers, they are more likely to be exposed to the consequences of the noted problem.
2. Objectives
Therefore, the present study aimed to determine the effect of cognitive-emotional intervention on the psychological distress of mothers of children with cancer referred to the chemotherapy ward.
3. Methods
The current research is a clinical trial to determine the effect of cognitive-emotional intervention on the psychological distress of mothers of children with cancer, which has been registered with the code number IRCT20160924029954N12. The studied population consisted of all mothers of children with cancer who were referred to the chemotherapy ward of Imam Ali Hospital in Zahedan in 2018.
Inclusion criteria for mothers consisted of having at least 20 years of age, minimum literacy, lack of cognitive impairments and psychiatric disorders, and no crisis occurring in the last six months except for child cancer. Inclusion criteria for children with cancer were age up to 12 years, receiving at least one course of chemotherapy, and no metastasis, according to records. More than one missing session in the Cognitive-Emotional Training Program, increasing severity of disease or critical patient status during the study due to metastasis, or any traumatic event affecting the mother’s psychological status were the most important exclusion criteria.
The sample size was estimated at 42 cases according to the mean and standard deviation of psychological status of mothers of children with leukemia in the study by Zafrian Moghaddam et al. (16) with a 95% confidence interval and 80% statistical test power. To ensure the adequacy of sample size and to consider probable loss, 50 individuals in each group and 100 subjects in total were determined (16).
Z1-α/2 = 1.96; S1 = 17.4;
The data collection tool was a two-part questionnaire. The first section contained the mother and child demographic information as well as disease information. The second part was Kessler’s psychological distress scale. The Kessler Psychological Distress scale (K-10) was developed in 1992 by Kessler et al. (17) to screen the general population. It was specified in subsequent studies that its 10-item form was more effective than other 6-item formats for identifying mood and anxiety disorders. It is also useful for monitoring and measuring the impact of psychological interventions and treatments. This tool has ten items that examines a person’s mental state over the past few weeks. The questions on this form are based on a Likert scale from “never” to “always” and are scored from 0 to 4. Therefore, the maximum score at K-10 is 40, and minimum is 0. A higher score indicates higher psychological distress. This tool does not target a specific psychological disorder, but it generally identifies the level of anxiety and depressive symptoms that a person has experienced over the past few weeks (17). The validity and reliability of this tool were verified by Yaghubi (18) in Iran. Based on his factor analysis, the questionnaire was confirmed to be single-factor, which had a positive and significant relationship with the score of general health. Its best cut-off point was obtained 8. Cronbach’s alpha and its reliability coefficients were 0.93 and 0.91, respectively (18). This tool has been used to measure psychological distress in mothers of children with cancer in Iran by Lotfi Kashani et al. (7). In this study, the reliability of this instrument was confirmed by Cronbach’s alpha (0.82).
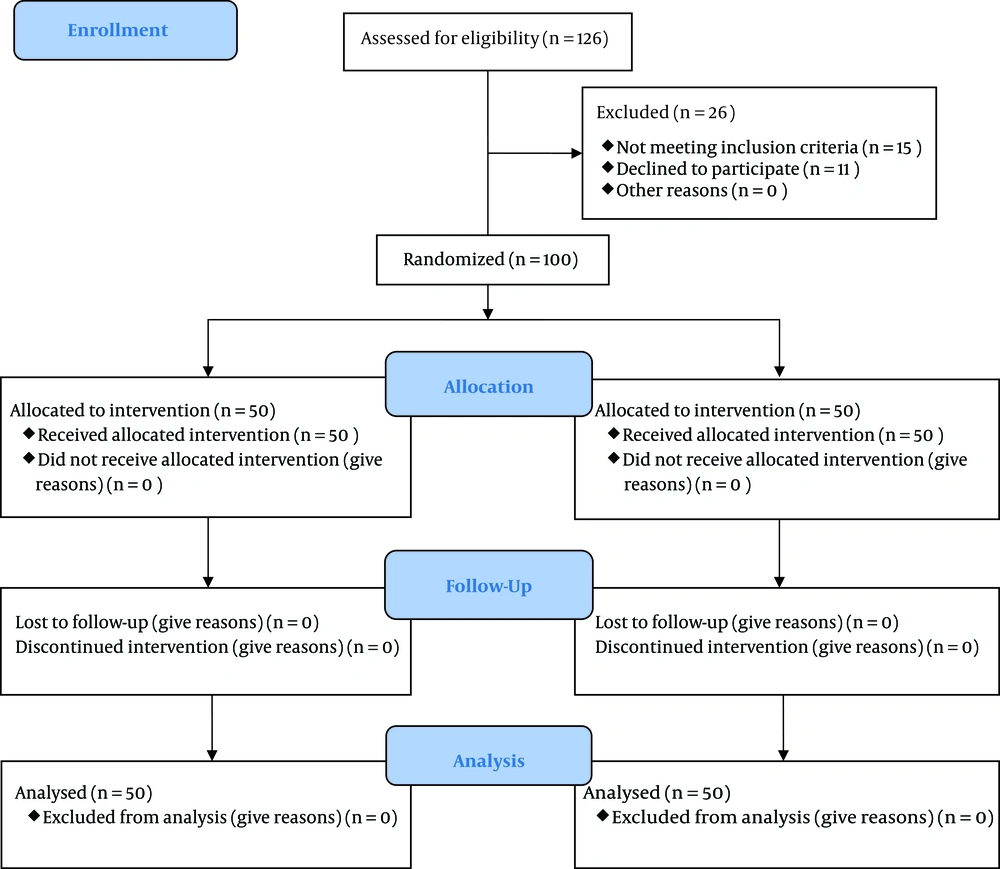
It was referred to the university-related hospital after approving the design and obtaining licenses, the Vice-Chancellor of research and technology. First, eligible participants were selected by identifying children with cancer referred to the chemotherapy department and mothers with the desired characteristics of the target population, using convenient sampling. Informed consent was obtained from mothers to participate in the study. A total of 126 individuals were examined, 26 individuals (15 due to not meeting inclusion criteria, 11 due to decline to participate) were excluded. As a result, the study was conducted and followed up on 100 samples (Figure 1). Then, the selected mothers were randomly assigned to the intervention and control groups. First, a total of 100 colored balls, identifying the study groups (red ball = intervention, white ball = control), were first prepared (Random allocation rule). Then, the group to which each woman belonged was determined based on the color of the ball picked out of the vase. As the eligible subjects were determined gradually, one of the extracted list numbers was allocated to the selected mothers. The mothers of both groups received pre-test by completing the Kessler scale questionnaire. In case the mothers were assigned to the intervention group, they would receive a 5-session emotional, cognitive training program (two sessions per week) in the form of small groups based on the content specified in Table 1.
| Session | Educational content |
|---|---|
| First | Getting familiar, introducing and expressing group rules, disease overview, psychosocial consequences and treatment process, normalizing emotional reactions to cancers. |
| Second | Training and practicing techniques of emotional disclosure, emotion drain, and self-regulation of emotions. |
| Third | Fears and concerns related to cancer, facilitating and practicing cognitive processing and conscious rumination. |
| Fourth | Reviewing the positive achievements and dimensions as well as the negative aspects of cancer diagnosis, the development of values and the prioritization of new values, and the redefinition of goals and the creation of a new philosophy of life. |
| Fifth | Spirituality, patience training, and positive thinking. Conclusion. |
Overall, 16 weeks after the end of the training sessions, the research questionnaires were completed again as a post-test by referring to the home or making an appointment in the ward. If the mothers were assigned to the control group, they would receive no intervention other than routine chemotherapy care, and the necessary coordination (address and telephone) would be provided to the mothers for the post-test. At the same 16-week interval, a post-test from the control group was also performed. However, after the end of the study, recommendations were offered from the educational content to the control group.
The principles of Cognitive Emotional Intervention used in this study were previously studied and used in a study by Hamidian et al. (13, 19, 20). The content of the intervention was provided and designed Primarily after studying the books and articles related to the subject and focusing on the Psychotherapy program by Ramos et al. (12). Then, five experts from the academic field of clinical psychology, health psychology, counseling, nursing, and oncology were consulted to increase the functional aspect. Their opinions were collected and reviewed by the research team, and the last educational content was finalized. Intervention was performed by a nurse with M.A in psychiatric nursing with clinical experience in oncology and cancer wards under the supervision of a person with a PhD in counseling. Data were analyzed after being collected by descriptive and inferential statistics using SPSS-22 software. The significance level in this study was considered (P = 0.05).
Data normality was assessed by the Shapiro-Wilk test. A chi-square test was used to compare the qualitative variables of the two groups. An Independent t-test was used to compare the quantitative variables of the two groups, and paired t-test was implemented for comparisons before and after applying intervention in each group.
The present study was approved by the Ethics Committee of Zahedan University of Medical Sciences (code: IR.ZAUMS.REC.1397.193). The most important ethical considerations in this study consisted of providing information about the study, obtaining written consent, being free to withdraw at any stage of the research, answering potential questions over the phone, and ensuring the confidentiality of the obtained information.
4. Results
Shapiro-Wilk test showed that mother’s psychological distress scores have a normal distribution in pre-test and post-test. According to Table 2, the demographic characteristics of the children with cancer and their mothers, it was shown that the mean age of the children in the intervention and control groups were 5.85 ± 2.75 and 5.00 ± 3.03 years, respectively, while the mean age of their mothers were 33.32 ± 6.76 and 35.34 ± 6.08 in the intervention and control groups, respectively.
| Group | Chi-Square Test | Independent t-test | ||
|---|---|---|---|---|
| Variable | Intervention, | Control | ||
| Sex | 0.55b | |||
| Girl | 23 (46) | 21 (42) | ||
| Boy | 27 (54) | 29 (58) | ||
| Total | 50 (100) | 50 (100) | ||
| Occupation | 0.72c | |||
| Employed | 3 (6) | 1 (2) | ||
| Unemployed | 47 (94) | 49 (98) | ||
| Total | 50 (100) | 50 (100) | ||
| Mothers’ education | ||||
| Under diploma | 32 (64) | 34 (68) | 0.67b | |
| Diploma and higher | 18 (36) | 16 (32) | ||
| Total | 50 (100) | 50 (100) | ||
| Family history of cancer | 0.22b | |||
| Yes | 8 (16) | 13 (26) | ||
| No | 42 (84) | 37 (74) | ||
| Total | 50 (100) | 50 (100) | ||
| Age of mothers, y | 33.32 ± 6.76 | 35.345 ± 6.08 | 0.12d | |
| Age of children, y | 5.85 ± 2.75 | 5.00 ± 3.03 | 0.37d | |
| Duration of cancer, y | 2.54 ± 0.83 | 76.2 ± 1.3 | 0.1d | |
aValues are expressed as No. (%) or mean ± SD.
bChi-square.
cFisher exact test.
dIndependent t-test.
The mean duration of developing cancer in children was 2.54 ± 0.83 and 2.76 ± 1.3 years for the intervention and control groups, respectively. Moreover, 54% of the children with cancer in the intervention group and 58% of the children in the control group were boys. In addition, 64% of the mothers in the intervention group and 68% of them in the control group were undergraduate. The majority of mothers in the intervention and control groups (94% and 98%, respectively) were housewives. Also, 16% of the mothers in the intervention group and 26% in the control group had a history of cancer in their families.
According to Table 3, regarding the effect of cognitive-emotional intervention on mothers’ psychological distress score, it was shown that the mean score of psychological distress of mothers of children with cancer in the intervention group before emotional, cognitive intervention decreased from 15.94 ± 8.88 to 6.16 ± 3.40 afterward. They noticed that the score in the control group changed from 17.00 ± 6.65 before emotional, cognitive intervention to 16.84 ± 6.67. Also, the mean changes in mothers’ psychological distress score in the intervention group was -9.78 ± 6.38, while it was specified to be -0.16 ± 0.73 in the control group. Independent t-test showed that the mean score of mothers’ psychological distress after cognitive-emotional intervention was significantly different between the intervention and control groups (P = 0.001). In addition, the mean of score changes in the two groups was shown to be significant (P = 0.001).
| Group | Numbers | Time, Mean ± SD | Changes, Mean ± SD | Paired t-test | |
|---|---|---|---|---|---|
| Before | After | ||||
| Intervention | 50 | 15.94 ± 8.88 | 6.16 ± 3.40 | -9.78 ± 6.38 | 0.001 |
| Control | 50 | 17.00 ± 6.65 | 16.84 ± 6.67 | -0.16 ± 0.73 | 0.13 |
| Independent t-test | 0.5 | 0.001 | 0.001 | ||
5. Discussion
The purpose of the present study was to determine the effect of cognitive-emotional intervention on the psychological distress of mothers of children with cancer referred to the chemotherapy ward. The main findings of the present study indicated that the mean score of mothers’ psychological distress after the cognitive-emotional intervention was significantly different between the intervention and control groups, and a significant reduction was observed. The results of the present study are in line with the quasi-experimental study of Sheikhsajadieh and Atashpour (21), in which the efficacy of dialectical behavioral group therapy on the psychological distress of infertile women was investigated.
Spirituality and positive thinking as part of the intervention which was implemented in this study can help reduce the severity of mothers’ stress symptoms. In this regard, a quasi-experimental study by Lotfi Kashani et al. indicated the effectiveness of spiritual intervention on decreasing the psychological distress of mothers of children with cancer in Tehran. The intervention group was exposed to eight sessions of acceptance and commitment-based group therapy. The results showed that the psychological dimension of quality of life in mothers of children with cancer was significantly higher in the intervention group than in the control group (10). It seems valuable to design multidimensional interventions in terms of education, cognition, emotion, and behavior that reduce the severity of psychological distress (22). Given the effectiveness of psychological interventions on parents of children with cancer, the study conducted by Zinivand et al. (2) showed that teaching positive thinking and optimism had a significant effect on reducing the anxiety level of parents of children with cancer aged 3 to 7 years. Therefore, this method can be an effective way to reduce psychological distress.
Since many parents of children with cancer experience stress, anxiety, and psychological distress in the form of post-traumatic stress symptoms, it can be stated that one of the therapeutic components in this intervention was enabling deep cognitive processing and encouraging conscious rumination in order to explain the effectiveness of cognitive-emotional intervention and its positive impact on decreasing the severity of post-traumatic stress symptoms. Encouraging and assisting mothers to consciously recall and process incident-related thoughts was crucial in this intervention as there is a significant relationship between subjective rumination and the severity of stress symptoms (23). In this regard, Oginska-Bulik and Ciechomska (19) believe that intrusive and unwanted rumination is destructive in nature. This process happens automatically, and no one can control it.
These thoughts are responsible for causing and sustaining the symptoms of stress. Conversely, mental rumination is conscious with a constructive nature and involves analysis of the position in order to search various solutions of problem as well as trauma processing. Conscious rumination contributes to regain control of the situation and finding ways to deal with problems. This process, on the one hand, is a facilitator of positive traumatic changes and, on the other hand, is a factor to end the continuation of the symptoms of stress (19). Cognitive processing-based therapy focuses on modifying and reconstructing distorted cognitions of incident-causing situations and unrealistic exposure to stress-causing events and enhances semantic and conceptual processing and encoding of situations. This process can contribute to post-traumatic improvement in addition to reducing the symptoms of stress (24). The limitations of this study included the short interval of 16 weeks for post-test and the inability of fathers to participate in the study. According to the present study, cognitive-emotional intervention reduced the mean score of mothers’ psychological distress.
5.1. Conclusions
Reducing the psychological distress of mothers as the primary caregivers of children with cancer can help improve the level of their mental health and quality of their life. Moreover, it can contribute to more participation and higher quality of care for children with cancer. Therefore, it is recommended in line with family-centered care to consider emotional and cognitive interventions for parents, especially mothers, during the chemotherapy of their children. Based on the positive results of the current study, the therapeutic elements of the cognitive-emotional intervention used in this research can also be used in other refractory diseases.