1. Context
Pregnancy causes anatomic and physiologic changes in the lower extremity, resulting in a variety of symptoms (1, 2). Edema is the accumulation of fluid in intercellular tissue. The interstitial and intravascular fluid are controlled by hydrostatic and the colloid oncotic pressure (COP). Fluid accumulation occurs when local or systemic conditions disrupt the balance (3).
The pressure on the pelvic vein and the inferior vena increases as the uterus grows in size. This causes venous insufficiency and leg edema by raising blood pressure in leg veins (4). Lower extremity edema occurs as a result of increased venous pressure in the legs, lymphatic blockage, and decreased plasma COP (5).
Varney defines gestational edema as the buildup of extra fluid in the tissues without the presence of hypertension or proteinuria (6). The mechanical pressure of gravid uterus on the inferior vena cava and iliac veins might create physiological lower leg edema, which inhibits venous return and also increased body fluids to accumulate in the tissues. Prostaglandin also induces vascular relaxation and reduces plasma COP, that endorses fluid movement from the vascular to extravascular space (1).
Leg edema is a common condition during pregnancy, limiting pregnant women’s activities (1). It can impact about 80% of pregnant women and should not be misinterpreted as an indication of pregnancy-related hypertension or preeclampsia (4). Swelling of lower extremities occurs in 35 to 80% of all normal pregnancies in late pregnancy (7). The study in Lahore, Pakistan (2015) reported a 67% prevalence of edema in pregnant women, with 49% of leg swelling, 33% of sacral edema, and 14% of edema in both areas (8). After long durations of standing and with each subsequent pregnancy, symptoms tend to intensify (9).
Differential diagnoses of physiological lower extremity edema from pathological edema include systemic diseases such as heart failure, liver disease, malnutrition, thyroid disease, localized conditions such as pelvic tumors, infection, trauma and venous thrombosis, and a variety of drugs, all of which increase the risk of lower extremity edema (10). The most common symptoms of dependent physiological lower leg edema include pain, night cramps, numbness, heaviness, and tingling (1). Pain can increase the secretion of stress hormones and stimulate the adrenal glands and sympathetic nervous system, which leads to increased blood pressure, irregular breathing, shortness of breath, as well as increased respiration rate and heart rate (11). During pregnancy, changes in blood flow might contribute to vascular insufficiency and thromboembolic event. Vascular insufficiency is observed in 43% and vascular diseases in 72% of pregnant women in late pregnancy. In addition, 50% of pregnant women experience complicated lower limb edema (9). Possible side effects of vascular insufficiency include infection, foot ulcers, stasis changes, and thrombosis (12).
Non-pharmacological methods for treating leg and foot edema in women include leg elevation, resting, water immersion, bandage, compression stocking, foot massage, intermittent pneumatic compression, reflexology, and monitoring the interstitial fluid movement (4, 9, 13). A common non-pharmacological intervention among health-care practitioners is foot massage (14). This technique in leg and foot edema increases peripheral blood flow by transferring extravascular fluid without disturbing intravascular (13), boosting oxygen, and therefore reducing edema (15). Ankle swelling appears to be reduced by external pneumatic compression and stocking and water immersion at 32°C for 50 minutes; these techniques can increase diuresis and decrease blood pressure (7, 16). However, the benefits and duration of changes are unclear (17). The most common treatments for venous insufficiency during pregnancy are compression stockings and leg elevation (4). Recently, there has been a rise in the acceptability of complementary therapies in the healthcare system (18). In clinical practice, the use of non-pharmacological therapies to supplement modern technical medicine is gaining popularity among nurses and midwives (19). Treatments for normal pregnancy aches and pains, such as edema should not endanger the mother and/or the fetus (20).
It is important to note that in pregnant women, the use of any treatment methods to reduce the symptoms associated with lower extremity edema requires careful examination and knowledge of the indications and contraindications related to the particular method. Considering the high frequency of lower extremity edema and its consequences in late pregnancy, different treatment approaches (drugs, supportive, invasive, and surgical methods), as well as lack of a review study to present all different methods affecting limb edema, the present study was carried out to review the interventions applied in reducing the symptoms of lower extremity edema during pregnancy. We also aimed to evaluate the effects of non-pharmacological treatments on relieving the symptoms associated with lower extremities in pregnancy.
2. Evidence Acquisition
2.1. Information Sources
Nine databases including MEDLINE, Cochrane Central Register of Controlled Trials, EMBASE, Web of Science, Scopus, Science Direct, Magiran, SID, and Google Scholar were searched for English and Persian articles published on the topic.
2.2. Search Strategy
Articles with the randomized controlled trial design were searched. We excluded the duplicated articles. Our search terms were as follows: “pregnancy” OR “late pregnancy” OR “obstetric” AND “oedema” OR “edema” AND “pharmacological treatment” OR “non-pharmacological treatment” OR, “management” OR “intervention” OR “complementary therapy” AND “lower-extremity” AND “leg edema in pregnancy” AND “limb edema in late pregnancy” AND “foot edema in pregnancy”, “water immersion”, “bandage”, “compression”, and “foot massage”.
2.3. Eligibility Criteria
All randomized controlled trials evaluating the interventions utilized to alleviate the symptoms of lower extremity edema during pregnancy published in English and Persian languages from January 1, 2011, to October 30, 2021, were included. We also included all studies investigating the non-pharmacological methods of lower extremity edema in pregnant women and clinical human studies. Unrelated and repetitive studies were excluded from analysis.
2.4. Study Population
The study population was pregnant women with lower extremity edema at any gestation period.
2.5. Types of Interventions
We included all non-pharmacological methods used to treat the symptoms of lower extremity edema during pregnancy.
2.6. Types of Outcome Measures
2.6.1. Primary Outcomes
The primary outcomes included the following: pain relief and the variables of physiological indicators, including circumference measurements of ankles, insteps, and foot/toe junctions (cm), foot volumetry (ML), peak systolic blood flow velocity (cm/s), and diameters of the great saphenous vein (DSV) and small saphenous vein (SSV) in the lower limbs (mm).
2.7. Selection Process
The screening process was performed by two authors. The full texts of the selected studies were reviewed, and finally, the relevant studies were included.
2.8. Quality Assessment and Risk of Bias
The Cochrane risk-of-bias tool for randomized trials version 2 (RoB 2) was used to evaluate the quality of the selected studies.
2.9. Data Collection Process
We extracted the following information from the included papers: (1) author(s), (2) title, (3) journal, (4) year, (5) volume, (6) issue, (7) pages of the article, (8) age, (9) gestational age, (10) number of pregnancies and deliveries of the participants, (11) design, the aim of study, (12) setting, (13) outcomes measured, (14) method(s) of analysis, and (15) results.
2.10. Narrative Synthesis of Data
Since meta-analysis was not possible due to the quality differences and high heterogeneity of studies, narrative synthesis was chosen as the best method to describe, compare, and combine the study findings.
3. Results
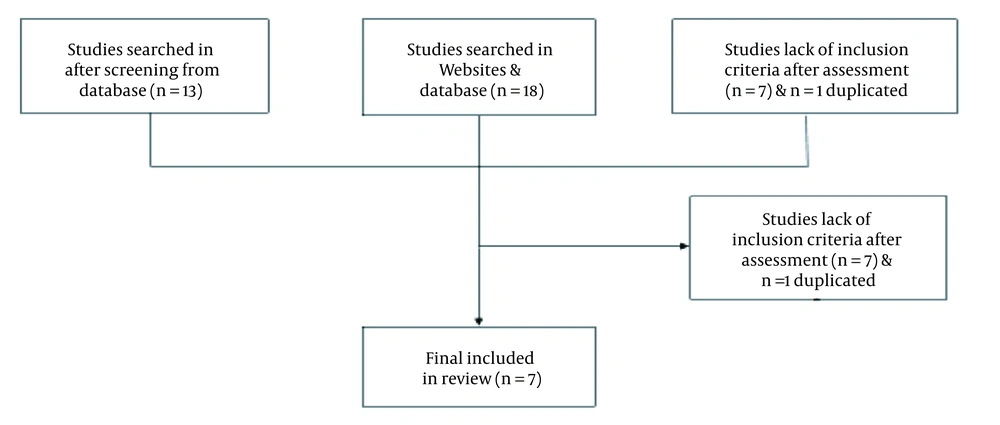
A total of 23 potentially relevant papers were identified by the systematic search in electronic database. Two papers were found from a reference list of other studies. Seven papers met our selection criteria and were included in the final review (Figure 1).
All the included studies had two intervention and control groups (Table 1). Out of seven studies, three studies assessed the benefit of massage compared with usual care, feet elevation, and water immersion. Also, one study compared the effects of massage with grape seed oil with sweet almond oil. In terms of analyzed outcomes, there were substantial differences between the assessed trials (9, 21-26). The trials had a high risk of performance and detection bias and were essentially unclear for selection bias.
Table 1 shows the review of seven randomized clinical trials.
| References | Country | Study Design | Number of Participants | Age Gestational Age | Number of Pregnancies | Aim of Study, Setting | Outcomes Measured | Result |
|---|---|---|---|---|---|---|---|---|
| Hassan Ahmed et al. (21) | Egypt | RCT | N = 90 | 18 - 35 years, pregnancy greater than 30 weeks gestation | Primigravida | Effect of effleurage massage versus water immersion with exercise on physiological foot edema among primigravida | Circumference measurements of ankles, insteps, and foot/toe junctions | The effleurage foot massage was more effective than water immersion exercise |
| Irion and Irion (22) | Alabama | RCT | N = 32 | 20 - 35; At least 34th weeks of a normally progressing pregnancy | Not given | Determine the effectiveness of water immersion as a means of reducing peripheral edema during the last six weeks of pregnancy | Foot volumetry (ML) | Significant reduction between groups |
| Gimunova et al. (23) | Czech Republic | RCT | N = 30 | 30 - 35 years; 25, 30, and 35 weeks of gestation | 1 - 3 | During the late stages of pregnancy, special footwear is designed to promote blood circulation in the feet and monitor venous blood flow variations | Doppler measurements (pulsed-wave) of the right popliteal vein were performed at three pregnancy phases, peak systolic blood flow velocity (cm/s) | CG: ↑ PSV EG: ↓ PSV |
| Foroozanfard et al. (24) | Iran | RCT | N = 120 | 20 - 35 years; 30 - 40 weeks | Primigravida | The effect of foot massage on the physiological edema of pregnancy | Circumference measurements of ankles, insteps and MP joints (cm) | Statistically significant difference between the mean of the measured environments in the feet (showed in both GC and CG (P < 0.00) |
| Rahimikian et al. (25) | Iran | RCT | N = 180 | 20 - 35 years; 30 - 40 weeks | Primigravida | Effectiveness of foot massage and feet elevation on physiological leg edema | Circumference measurements of ankles, insteps and MP joints (cm) | Massage therapy has a greater effect on reducing leg edema than legs elevation |
| Navaee and Rakhshkhorshid (26) | Iran | RCT | N = 90 | 18 - 35 year; 30 - 40 week | Primigravida | Physiological leg edema and the effect of foot massage with grape seed oil and sweet almond oil in primigravida | Circumference measurements of ankle, instep & MP joint (cm) | Decrease of the sizes in the two intervention groups and their increase in the CG |
| Saliba Junior et al. (9) | Brazil | RCT | N = 60 | 18 - 35 years; 32 - 40 weeks | 1 - 4 | To assess the effectiveness of compression stockings in controlling the varicose veins in pregnant women | Diameters of the GSV and SSV in the lower extremities of pregnant women in an orthostatic position | Intervention group showed a significant reduction in the final diameter of the GSV compared to the initial diameter in the distal and proximal leg of both sides (P < 0.0001) |
| Total | 7 | |||||||
Abbreviations: MPJ, metatarsal phalangeal joint; PSV, peak systolic velocity; GSV, great saphenous vein; SSV, small saphenous vein; EG, experimental group; CG, control group; NS, not significant.
The non-pharmacological therapies that we investigated in this study included foot massage, wearing compression stocking and special footwear, immersion in water, feet elevation and resting. Various studies have shown the effective role of foot massage in reducing lower extremity edema in pregnant women (4, 25, 26).
Khedr and Hemida compared the effect of leg elevation versus water immersion on leg edema in the third trimester of pregnancy. The findings revealed that there were no significant variations between pre- and post-interventions. The results also showed that leg elevation and water immersion could alleviate edema in lower extremities during pregnancy (27).
Gimunova et al. studied the effect using of special footwear to promote blood circulation in the legs by observing venous blood flow variations during late phases of pregnancy; with advancing phases of pregnancy, the peak systolic velocity in the popliteal vein significantly decreased in the control group, whereas it increased significantly in the experimental group. No significant change in cross-sectional area was observed in any of the groups. The results of the experimental study showed that wearing the tested footwear could prevent venous blood velocity from lowering during the later stages of pregnancy. Nonetheless, more research is required on the beneficial effects of using the footwear on venous flow and its application (23).
Irion and Irion evaluated the effect of water immersion on reducing peripheral edema in the last six weeks of pregnancy. The results showed that water immersion for 20 minutes in a swimming pool at 80 to 95 Fahrenheit was an effective method for reducing leg edema during pregnancy. This may be because water pressure enters from all sides and pushes extracellular fluid into the intravascular chamber, resulting in increased central blood volume, which can lead to increased uterine blood flow and reduced edema of legs (22).
Rahimikian et al. compared the effects of feet elevation versus massage in lower extremity edema in pregnant women. The results indicated that massage therapy was more effective than keeping the legs high in reducing physiological edema of the lower extremities. Probably, massage helps restore venous blood flow through the pumping effect of muscle contraction (25).
Navaee and Rakhshkhorshid (2019) compared the effect of massage with sweet almond oil with grape seed in nulliparous pregnant women. According to their results, there were no significant differences between the two groups in reducing the physiological edema of the legs (26).
4. Discussion
Currently, there is not enough evidence for the management of physiological lower extremity edema during pregnancy. The efficacy of these interventions is unknown, although they appear to be mostly safe. Several studies with different designs and criteria have examined different types of non-pharmacological treatments and complementary therapy for lower extremity edema in pregnancy.
The findings of this study showed that the effectiveness and efficacy of different non-pharmacological supportive treatment methods varied from each other. Physiological changes occur throughout the body during pregnancy, especially in the heart function and arteries, leading to the onset and exacerbation of vascular disease, the possibility of regression, and improvement of symptoms through this period to the postpartum period spontaneously. Therefore, the adoption of various treatment methods in this period should be recommended regarding the detailed characteristics of symptoms, their severity, as well as the hierarchy of their use based on the types of more effective supportive treatment methods.
The oldest and newest methods proposed in these studies consist of the use of foot massage. The effectiveness of this method is in accord with the study done by Rahimikian et al. (25), as well as the study conducted by Foroozanfard et al. (24), and Navaee and Rakhshkhorshid (26).
Due to the absence of relevant and important information from available trials, no reliable conclusions can be made to guide clinical practice regarding the management of pregnant women with leg edema. Also, there is the possibility of adverse effects, and the safety of non-pharmacological interventions cannot be verified from the available data.
Regarding the importance of pregnancy, health and quality of life in pregnant women, as well as the high prevalence of leg edema at the end of this period, further studies are required for safe therapies.
We cannot provide any specific guidance regarding the type of intervention utilized to reduce the symptoms of pregnancy-related leg edema. Further large, well-designed multi-center randomized controlled trials with clear allocation concealment are required to allow for robust conclusions to be drawn. It should also be noted that the largest trial included in this review involved only 180 women. Limiting the findings to the results of studies published only in English and Persian languages and confining the results to the short range of study time were among the limitations of this study. Due to the limited clinical research conducted on the population of pregnant women and the importance of the subject, it is suggested that more clinical studies with newer topics for the treatment of lower extremity edema during pregnancy be conducted. Among the other limitations, we might mention that massage was performed by the researcher herself, the study period was relatively short, and we did not include the follow-up phase.
4.1. Conclusion
There is not enough evidence on treatments for physiological lower extremity edema during pregnancy. It is suggested that the effectiveness of these methods, especially supportive treatment and complementary medicine in pregnant women, be further investigated. Also, it is possible to evaluate the persistence of the massage treatment sessions, as well as educating pregnant women to perform massages on themselves.