1. Background
Labor pain has been one of the most common pains since the dawn of time. Pain is an inevitable phenomenon in the labor process (1). Continued pain and fear of pain during labor can have adverse effects on the respiratory, circulatory, and endocrine systems, as well as other body functions (2). Fear of labor pain occurs in more than 6% of pregnancies and its prevalence is ever-increasing such that today it accounts for about 8% - 22% of cesarean sections, which are associated with increased surgical complications and risks for mothers. This type of fear is more common in primiparous women (3, 4). Managing labor pain is one of the key features of midwifery care and is the primary goal of delivery care (5).
Many pharmaceutical methods are now used to relieve labor pain. Meanwhile, these methods should not be the first choice to control pain due to the potential side effects of analgesic and anesthetic agents such as hypoxia, hypotension, and cardiac arrhythmia on the mother and the occurrence of respiratory problems for the fetus (6, 7).
On the other hand, non-pharmaceutical methods of pain relief have many advantages, including no side effects for the mother and fetus, no interference with the delivery route, and even feeling of comfort for the mother and fetus (8). Some of these methods include muscle relaxation, breathing techniques, hydrotherapy, music therapy, touch and massage therapy, supportive techniques, heat and cold therapy, essential oil therapy, acupuncture, herbal medicine, exercise, and acupressure (8, 9).
In recent years, more attention has been paid to such approaches as acupressure for pain management. Basically, acupressure resembles acupuncture (9). There are numerous acupressure points in the body for reducing labor pain, and it is believed that stimulating these points, in addition to providing energy balance and mitigating labor pain, can release oxytocin from the pituitary gland, trigger uterine contractions and consequently, facilitate the labor (7).
According to traditional Chinese beliefs, the vital energy of the body (chi) flows in channels called meridians and regulates body functions. The blockage of meridians leads to negative outcomes including pain stimulation. By applying pressure on some parts of the body, one can access these channels and balance the energy between Yang and Yin (two expressions of vital energy in the body) and thus, promote health and relieve pain (10). One of the points that is useful for mitigating labor pain is Sanyinjiao. This is the spleen 6 acupoint, which is four finger-breadths above the inner ankle behind the posterior tibial plateau (11).
In addition to acupressure, another non-pharmaceutical method for pain relief is the use of different modes of heat and cold therapy. Cold therapy can alleviate pain through various mechanisms including the induction of anesthesia, prevention of pain perception by stimulating peripheral nerve receptors, facilitating energy flow in acupuncture points, reduction of muscle tension, slowing down the transmission of pain signals to the central nervous system, and distraction (12, 13). In addition to the mechanisms described for cold therapy, heat therapy may stimulate the skin and deep tissue receptors to suppress pain (11). In fact, according to the gate control theory, the passage of pain signals is blocked by closing the valve system in the spinal cord (14).
Studies have shown that the ice massage on acupuncture points reduces labor pain (9, 15, 16). A study by Ganji et al. suggested that hot and cold compresses could reduce the overall pain of labor (13). Although no study has directly examined the effect of hot and cold massage at spleen 6, several lines of evidence imply that applying hot and cold compresses relieves labor pain even when they are not administered at acupressure points (13, 14, 17). Furthermore, Sirati Nir et al. observed that applying ice massage on the Hegu point decreases pain intensity immediately and 30 and 60 minutes after the intervention (16).
2. Objectives
In this context, the present study aimed at comparing the impact of hot and cold massage at spleen 6 on pain relief during active labor. The results could be used by treatment teams, especially midwives, to relieve mothers’ pain and suffering and prevent unnecessary cesarean sections.
3. Methods
This double-blind clinical trial was approved by the Deputy of Research and the Ethics Committee of Zabol University of Medical Sciences (ZBMU.1.REC.1396.117). A total of 80 pregnant women admitted in 2017 to the Maternity Ward of Amir Al-Momenin Hospital in Zabol, Iran, participated in the study. The eligibility criteria included singleton pregnancy, primiparity, age of 18 - 35 years, gestational age of 37 - 41 weeks, fetal cephalic presentation, active labor phase (cervical dilation > 4 cm) (18), no chronic diseases (heart disease, pulmonary disease, hypertension, and diabetes), absence of high-risk pregnancy (gestational hypertension, decreased fetal movements, intrauterine growth restriction, fetal death, polyhydramnios, and oligohydramnios diagnosed by ultrasound, premature rupture of the membranes (PROM) for more than 12 hours, history of infertility, placental abruption, and fetal abnormal heart rate at the outset of the study), no medical record of depression, minimum reading and writing literacy, no skin disorders such as eczema and superficial skin infections (which are of acupuncture limitations), no use of oxytocin for labor induction, and using no other methods of anesthesia before entering the study. On the other hand, the exclusion criteria were the failure of the client to continue the intervention, withdrawal from the normal course of labor, and emergency cesarean section. All qualified mothers were informed of the purpose of the study and their informed consent was obtained. The subjects were chosen using convenience purposive sampling and were randomized into two groups.
Assuming α = 0.05 and β = 20% and considering a similar previous study (19), as well as a 10% attrition, the sample size in the present study was estimated at 40 individuals for each group (n = 80 in total). At the time of mothers’ admission to the maternity ward, after checking the medical history and performing required examinations, the researcher invited eligible willing subjects to enter the study. Sampling continued until the target sample size reached. In order to prevent the two groups from any contact with each other that might lead them to know about their type of intervention, the sampling days were divided into two sets using a random number table. Thus, cold massage was scheduled for even days and hot massage was applied on odd days.
Data collection tools included a demographic and midwifery questionnaire (age, job, education, number of abortions, gestational age, and delivery information) and McGill Pain Questionnaire. Studies have shown that numerical rating scales have good validity for measuring pain severity, and they have been frequently adopted by many researchers (5, 20). In the present study, necessary instructions on how to find the pressure point, how to apply pressure, the amount of pressure, and other relevant issues were acquired from an acupuncturist.
The objectives and procedure of the study, as well as the way of using the medical pain ruler, were explained to the subjects. At all stages of the study, we maintained emotional, verbal, and non-verbal communication with the mother and provided psychological support. Before any intervention, the pain intensity was measured at 4-cm cervical dilation (the beginning of active labor phase) in both groups. For this purpose, after two uterine contractions and experiencing labor pain, the mother was asked to score pain on a 10-cm medical ruler. The indicated number was recorded in the questionnaire, and then the intervention began.
In the Sanginjiao point group, the Sanginjiao point (SP-6 located four finger-breadths above the ankle behind the posterior tibial plateau) was marked and the pressure was applied by the thumb on the Sanginjiao point. In the cold massage group, 2-cm ice molds were used. An ice mold was put in a nylon bag and wrapped in a thin gauze to prevent moisture transfer and direct contact with the skin. A hot water bag (38 to 40°C) was used for hot massage. The temperature of the water bag was controlled using a mercury thermometer. It should be noted that the thermometer remained along with the bag until the temperature of water was stabilized and reached 38 - 40°C while it was put at the mother’s bed. To prevent the direct contact of heat with the skin, a protective layer (gauze) was placed on the site between the skin and the bag.
The regular and rotational massage was given for 30 minutes. Initially, 60-seconds massage (30 seconds clockwise and 30 seconds counterclockwise) was administered without regard to contractions. Then, the patient rested for one minute. This process continued until the 30-minute massage time completed. Prior to the intervention, the pressure applied by the research assistant’s fingers was measured 20 times using a digital weighing scale (Sergio) with an accuracy of 1 g. The mean pressure applied to the SP-6 point was between 1.5 and 3.5 kg, and it took one hour to complete the procedure. The 30-minute massage was selected in order to ensure that the energy cycle was complete. The pain was measured before and 5 minutes after the start of the intervention, 30 minutes after the start of the massage, and 30 minutes after the end of the intervention. In order to prevent hypotension during the massage, patients were asked to lie down on the left side.
Data were analyzed by SPSS V. 21 using the Independent t-test, one-way ANOVA, and repeated measures ANOVA at a significance level of 0.05.
4. Results
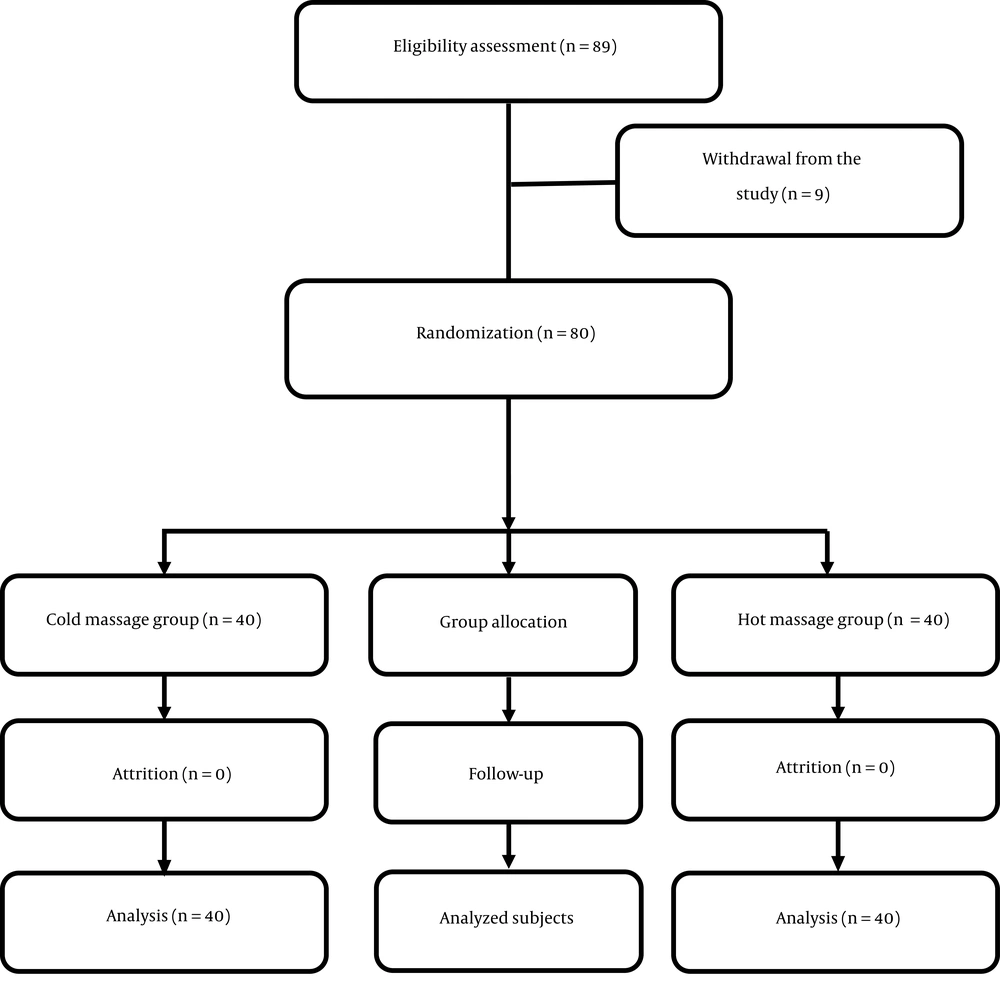
Finally, 80 patients completed the study and there was no attrition in the sample (Figure 1). The mean age of the subjects was 24.80 ± 5.98 years in the hot massage group and 23.98 ± 4.57 years in the cold massage group. The Independent t-test indicated no significant difference between the two groups (P = 0.491).
The mean age of the spouse was 28.75 ± 6.62 years in the hot massage group and 26.93 ± 5.24 years in the cold massage group (P = 0.176). The mean neonatal weight was 2903.75 ± 476.14 g in the hot massage group and 3133.37 ± 287.48 g in the cold massage group (P = 0.011). The results suggested that the two groups were matched in terms of demographic and midwifery characteristics (occupation, residence, infant’s gender, and type of delivery) (Table 1).
| Variable | Hot Massage | Cold Massage | P Valueb |
|---|---|---|---|
| Occupation | 0.370 | ||
| Housewife | 36 (90) | 35 (87.5) | |
| Employee | 4 (10) | 5 (12.5) | |
| Total | 40 (100) | 40 (100) | |
| Residence | 0.723 | ||
| Urban | 19 (47.5) | 23.5 (57.5) | |
| Rural | 21 (52.5) | 17 (42.5) | |
| Total | 40 (100) | 40 (100) | |
| Infant’s gender | 0.501 | ||
| Female | 23 (57.5) | 20 (50) | |
| Male | 17 (42.5) | 20 (50) | |
| Total | 40 (100) | 40 (100) | |
| Mother’s education | 0.20 | ||
| Primary school | 9 (22.5) | 10 (25) | |
| Secondary school | 17 (42.5) | 7 (17.5) | |
| High school diploma | 11 (27.5) | 11 (27.5) | |
| Academic degree | 3 (7.5) | 12 (30) | |
| Total | 40 (100) | 40 (100) | |
| Type of delivery | 0.644 | ||
| Intended | 38 (95) | 37 (92.5) | |
| Unintended | 2 (5) | 3 (7.5) | |
| Total | 40 (100) | 40 (100) |
Comparison of Demographic and Midwifery Characteristics of Primiparous Women in Hot and Cold Massage Therapy Groupsa
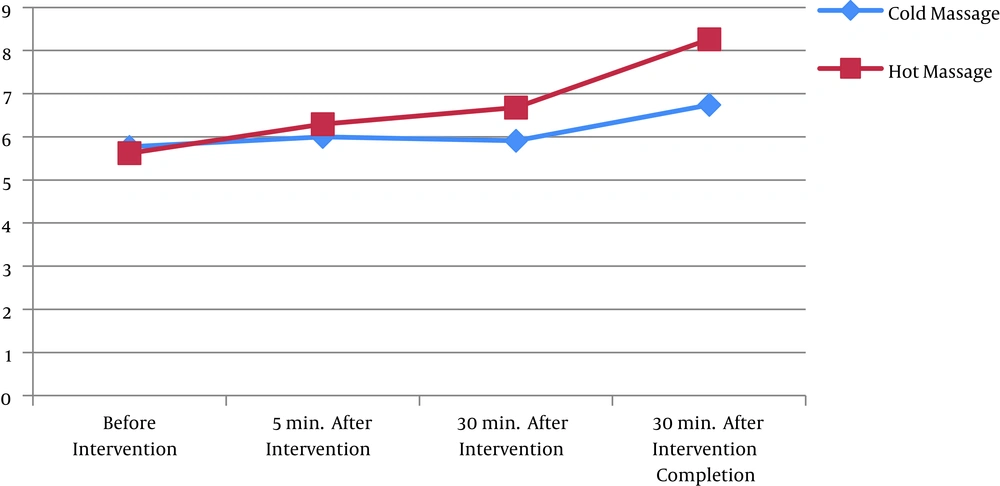
The results of repeated measures ANOVA showed that the mean changes in pain intensity at different stages were not similar in mothers receiving hot and cold massage (P = 0.0001). In the hot massage group, the results showed no significant difference in the pain score before the intervention, 5 and 30 minutes after the start of the intervention, and 30 minutes after the end of the intervention (P = 0.62 and P = 0.07). However, significant differences in the pain score were observed between the following stages: before the intervention and 30 minutes after the start of the intervention, before the intervention and 30 minutes after the end of the intervention, 5 minutes after the start of the intervention and 30 minutes after the end of the intervention, and 30 minutes after the start of the intervention and 30 minutes after the end of the intervention (P = 0.002; P = 0.0001; P = 0.0001; and P = 0.0001, respectively). On the other hand, no significant change was seen in the pain score of mothers in the cold massage group before and 5 minutes after the start of the intervention, before the intervention and 30 minutes after the start of the intervention, 5 minutes after the start of the intervention and 30 minutes after the start of the intervention (P = 0.99, P = 0.99, and P = 0.99, respectively). Nevertheless, pain intensity in the cold massage group differed significantly between the following stages: before the intervention and 30 minutes after the end of the intervention, 5 minutes after the start of the intervention and 30 minutes after the start of the intervention, and 30 minutes after the start of the intervention and 30 minutes after the end of the intervention (P = 0.05, P = 0.001, and P = 0.001, respectively), indicating the positive effect of cold massage on pain intensity (Figure 2).
The results of pairwise comparisons using Bonferroni test revealed no significant difference in the mean pain intensity of mothers receiving cold and hot massage before and 5 minutes after the start of the intervention (P = 0.65 and P = 0.11); but the two groups showed a statistically significant difference in the mean scores of pain measured 30 minutes after the start of hot and cold massage and 30 minutes after the end of the intervention (P = 0.0001 and P = 0.0001, respectively) (Table 2).
| Source of Variable | Sum of Squares | Degree of Freedom | Mean | t-Test | Significance Level | Effect | Power |
|---|---|---|---|---|---|---|---|
| Stage | 111.25 | 3 | 37.08 | 34.22 | 0.0001 | 0.3 | 1 |
| Stage and group interaction | 23.93 | 3 | 7.97 | 7.36 | 0.0001 | 0.08 | 0.98 |
| Error | 253.55 | 234 | 1.08 | ||||
| Group | 34.45 | 1 | 34.45 | 13.24 | 0.0001 | 0.14 | 0.94 |
| Error | 202.96 | 78 | 2.60 |
Results of Repeated Measures ANOVA Concerning the Mean Score of Pain Intensity Before and After the Intervention in the Two Study Groups
5. Discussion
The results of the study established that the cold massage at SP-6 was more effective in reducing labor pain than was the hot massage. Inasmuch as previous studies have not compared the effect of hot and cold massage at SP-6 on the relief of active labor pain, comparing the results of this study with those of previous studies may be impossible in some cases. Nevertheless, the findings of the current study are consistent with those reported by Ganji et al. in terms of decreasing labor pain intensity through hot and cold massage therapy. In the mentioned study, the procedure involved using a warm water bag (38 - 40°C) wrapped in a towel and placing it on the upper abdomen, lower abdomen, and the back for 30 minutes during contractions; then, an ice bag was put in the same positions for 10 minutes during the first stage of labor. In the second phase, the hot water bag was placed on the perineum for 15 minutes; then, the ice bag was placed in the same position for 5 minutes. The results suggested that during the first and second stages, pain intensity was significantly lower in the intervention group receiving intermittent cold/hot massage than in the control group (13). In the present study, although hot/cold massage was not used on the same subjects alternately and the effect of cold and hot massage at SP-6 was investigated separately, the two studies are consistent insofar as the impact of hot and cold massage on alleviating pain during active labor is concerned. Moghimi Hanjani et al. explored the effect of local heat therapy on labor pain, labor outcomes, and satisfaction of primiparous women. They observed no significant difference between the two study groups with regard to pain intensity before the intervention; however, in the first and second stages of labor, the two groups experienced significantly different degrees of pain. The mentioned study matches the present study concerning that both studies inquired into the impact of heat on pain intensity, but it is not useful to compare the two studies due to differences in the type of intervention each used (14). Heat therapy may be effective in reducing pain through various mechanisms. It stimulates heat receptors on the skin and deeper tissues, which may lower pain due to operating in accordance with the gate control theory (11).
In a clinical trial assessing the impact of acupressure at SP-6 on labor pain and length of delivery, Lee et al. showed that the stimulation of SP-6 significantly reduced pain at all stages in the intervention group. This study is similar to the present study in terms of the effect of acupressure on labor pain (6). As stated above, in the present study, there was a significant difference in pain intensity between the two groups 30 minutes after the start of the intervention and 30 minutes after the end of the intervention (6). It should be specified that Lee et al. applied pressure during labor contractions, which naturally caused the duration of pressure administration to vary across participants. However, the duration of pressure or touch was the same for all subjects in the present study. Moreover, Lee et al. did not administer cold and hot massage. Heidari et al. considered the influence of acupressure on pain intensity before and after the intervention and then every hour until the end of the first stage of labor. However, they reported no decline in pain following acupressure (21), which is not in agreement with the present study. Kaviani et al. compared the effect of two methods of acupressure and ice massage at the LI-4 point and observed reductions in pain intensity, anxiety, and labor length among subjects receiving these two interventions when compared to the control group (22), which is in line with the present study. Although we had no control group, cold massage at SP-6 led to better pain relief than hot massage. Some researchers maintain that ice massage, like acupuncture and transcutaneous electrical nerve stimulation (TENS), functions based on the gate control theory of pain. On the other hand, there is compelling evidence that cold-induced nerve messages transmitted exclusively by A-delta fibers are sufficient to activate descending pain pathways. Since there are several descending pain inhibitory systems, each system may be triggered by different types of severe sensory impulses (9, 23). In line with the present study, Strati Nir et al. confirmed the positive effect of ice massage on mitigating labor pain; in the mentioned study, the maximum duration of each round of ice massage was 2 minutes, followed by a 15-second rest, for a total duration of 10 minutes. However, in the present study, the intervention was conducted for 30 minutes during uterine contractions. Given the more effectiveness of ice massage than hot massage in reducing the intensity of labor pain without side effects, it is strongly suggested that this effective intervention be repeatedly administered during the active labor process that is accompanied by prolonged pain (16).
The results propose that ice massage and acupressure, after completing the intervention, exerted different effects on reducing pain intensity and duration of labor, with ice massage causing a higher reduction in this regard. The reason may be that ice massage is better in stimulating thin-fiber receptors than acupressure. Therefore, it is possible to strengthen the effect of acupressure on labor pain by increasing the number of episodes and duration of applied pressure. Sustained stimulation of acupuncture points may amplify the flow of vital energy in the meridians and thus yield more notable therapeutic effects. Further studies need to be undertaken to substantiate this suggestion.
Various factors including individual differences concerning pain severity threshold, cultural and social factors, and psychological characteristics could influence the experience of labor pain. As the main limitation of the present study, these factors were not taken into account.
5.1. Conclusions
Considering changes in population control policies and the adoption of pro-natalist policies with an emphasis on natural childbirth in Iran and other countries with population decline rates, it seems that employing safe, non-invasive, simple, inexpensive, and low-risk approaches such as acupressure, thermotherapy, and cryotherapy to relieve pain and reduce the duration of labor is rewarding and could lead to mothers’ active participation in the labor process and enhancing their satisfaction with vaginal delivery.