1. Background
Cerebral palsy (CP) is one of the most common causes of disability among children, and most of children with this disability would depend on their care provider or parents for the rest of their lives (1). Cerebral palsy is defined as "a group of persistent disorders in the development and movement of individuals". According to available statistics, it is one of the most common chronic disabilities in childhood, with an annual prevalence rate of 1.5%, which is more than 4% per 1000 live births (2-4). Despite the advances in CP diagnosis and treatment during recent decades, its incidence remains high due to the poor knowledge of risk factors and how to care for the affected child and the lack of long-term care facilities (5).
Children with CP experience frequent hospitalization throughout their lives. Childhood illness and hospitalization is a crisis and can cause anxiety for parents and children (6-8). Parents of these children face numerous difficulties while taking care of their children, which would have a great impact on their health (1, 9). One of the main causes of parents' anxiety that affects their mental health is inadequate parental knowledge of how to care for a hospitalized child. This would lead to the inability of parents, especially the mother, to take care of the child (10). Child care is one of the primary duties of a parent, but this role varies widely in children with chronic illnesses and long-term dependencies (11). Therefore, a child's disability not only would affect his/her own life but due to the extra burden, it imposes on the family, especially the mother, it is also associated with multiple problems (12, 13). This especially happens in developing countries where families have limited resources, which makes parents, especially mothers, unable to adequately address other aspects of their lives (13).
Long-term care of a child with CP causes anxiety, fatigue, and deterioration of mothers' mental health, which in turn, would decrease their ability for providing long-term care for their children (14-17). One of the ways that nurses could continue their care and education even after the discharge of the child from hospital is to use the continuous care model (CCM) (18). Using this model, nurses would be able to care for both the patient and their family (19). The main purpose of this model is to design a program that promotes knowledge, acceptance, appropriate behaviors, and control over the disease and its complications (20).
2. Objectives
Given the significance of caring for children with CP and the need to pay attention to the mental health of these children, this study was designed to investigate the impact of the CCM on the mental health of mothers with children suffering from CP admitted to 17-shahrivar Hospital of Rasht during 2019.
3. Methods
3.1. Participants and Study Plan
The present study was a two-group, parallel design clinical trial performed among 80 mothers of children with CP. The sample size was calculated based on a related article with the confidence interval of 95% and power of 80% (18); the samples were recruited from the Neurology Department of 17-Shahrivar Teaching Hospital of Rasht, Iran, from January to July 2019. In this study, the participants were assigned to the intervention and control groups using random block allocation.
The inclusion criteria included: Being mother of a child aged from 4 to 12 years hospitalized due to CP, not being an employee of the health care system, and not having experienced any specific accidents affecting the mental health of mothers, such as death of a loved one, divorce or financial crisis. One of the main reasons for not involving the fathers in the present study was that in 17-Shahrivar Children Hospital, only mothers are allowed to stay with and care for their children during the hospitalization period; thus, nurses are mostly in contact with mothers.
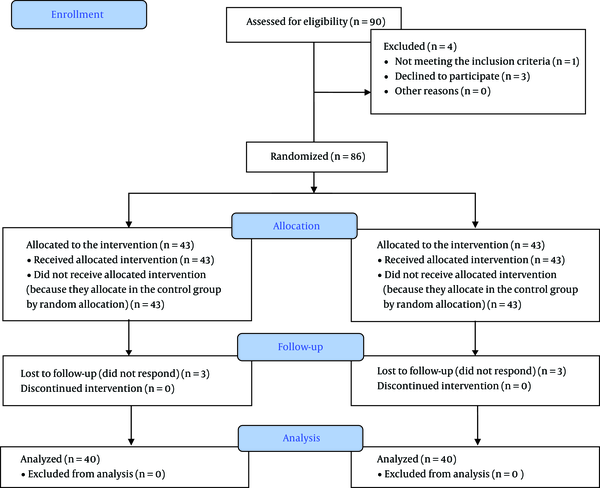
The exclusion criterion at the beginning of the study was being on the list of educational follow-up of nursing after hospital discharge. The exclusion criteria during the study included failure to participate in all the training courses and unwillingness to continue participation during the intervention period (Figure 1).
3.2. Instrument
3.2.1. Demographic Characteristics
For the present study, demographic characteristics included age (year), education (under diploma, diploma, bachelor’s degree, and higher educational degrees), participation in any child caring programs (yes, no), having anxiety (yes, no), having another children with CP (yes, no) and experiencing depression due to having a child with CP (yes, no).
3.2.2. General Health Questionnaire
The General Health Questionnaire (GHQ) is a screening device for identifying minor psychiatric disorders in the general population and within community or non-psychiatric clinical settings, such as primary care or general medical outpatients. Suitable for all ages from adolescence upwards – not children, it assesses the respondent’s current state and asks if that differs from his or her usual state. It is, therefore, sensitive to short-term psychiatric disorders but not long-standing attributes of the respondent. The self-administered questionnaire focuses on two major areas: The inability to carry out normal functions and the appearance of new and distressing phenomena. This questionnaire consists of 28 items and has four sub-scales, including somatic symptoms (items 1 - 7), anxiety/insomnia (items 8 - 14), social dysfunction (items 15 - 21), and severe depression (items 22 - 28) (21). Its validity and reliability have been confirmed in various studies in 38 different languages, including Farsi (22, 23). Each item has four possible answers (including 'better/healthier than normal', 'same as usual', 'worse/more than usual', and 'much worse/more than usual'). The exact wording will depend upon the particular nature of each item. There are two methods of scoring for this questionnaire: (1) one is the traditional way in which the options are scored as (0 - 0 - 1 - 1); and (2) the maximum score on the questionnaire will be 28. Another method of scoring is the Likert scoring method where the options are 0, 1, 2, and 3. The maximum score for this method will be 84. Lower scores show better mental health. The cut-off point of this test was considered at 23; a score above 23 indicates a mental disorder, and a score below 23 indicates no mental disorders (22, 24).
3.3. Study Procedure
After obtaining informed consent from the participants, they were randomly divided into the two groups of intervention and control. In the random block allocation method, since there were two groups, four blocks were used, which were named A, B, C, and D, and the sequence of each group in each block was determined according to the related website (https://www.sealedenvelope.com/). Since the researcher explained the purpose of the study to all the participants and explained that they might be allocated into either the intervention or control group, blinding was not applicable.
In the intervention group, mothers completed the Mental Health Questionnaire before the intervention, and then CCM was applied for them. In this regard, they were followed up for one and eight weeks after discharge from the hospital. The CCM consists of four stages, including orientation, sensitization, control, and evaluation. Description and goals of each stage are presented in Table 1.
| Stage | Description |
|---|---|
| Orientation | This stage is designed to create the appropriate sensitivities about the disease of children, proper recognition of the problem, motivation, and sense of need, and sensitivity to the necessity of follow-up. The researcher and the mothers who were involved in child care discussed and justified the goals and identified the possibilities, limitations, and expectations in ten sessions that lasted for fifteen minutes in the waiting room of the Neurology Department. |
| Sensitization | The sensitization phase was aimed at involving the patient and their family in the development of ongoing care behaviors. This phase was initiated at the same time as the orientation phase, and the most important part of this stage was counseling for mothers. It was implemented during 4-6 meetings that lasted 30-45 minutes each based on the acceptance and tolerance of the mothers. At this stage, the researcher discussed the following topics with the mothers: Features of CP, its diagnosis, treatment and prognosis, the importance of following good diet and healthy habits for the child, attention to physical activity, prevention of bed sore, weight control, regular visits to the physician and occupational therapist and following the given instructions, training to reduce the mother’s stress and anxiety, the significance of exercising and visiting a psychologist if necessary, and signs and symptoms of infection including fever, cough, shivering, anorexia, nausea, and vomiting. Individual sessions were held for mothers during or at the end of the children's hospitalizations. |
| Control | In the control phase, consultation was continued to survey and evaluate new care problems (the patient’s behavior and their use of training sessions) and care process (successes and failures) through phone calls or face-to-face meetings. This stage lasted for one week. |
| Evaluation | At the final stage, the mothers' mental health was evaluated in two phases, including immediately and one month after the intervention. |
Stages of the Continuous Care Model Was Used in the Study
The control group received the Mental Health Questionnaire before the intervention, and mothers only received the routine education about their child's illness and other cares provided by the nurses in the Neurology Department of the hospital at discharge. Mental health of both groups was measured again at the end of the first and eighth weeks after discharge from hospital.
3.4. Ethical Approval
This study has ethical approval from the Ethics Committee of Guilan University of Medical Sciences (IR. GUMS. REC.1397.526). Participation in this study was completely voluntary, and parents were fully informed about the benefits of this study, and informed consent was obtained. Parents were also informed that the results of the study would be provided to them if they desired. In order to adhere to the ethical principles of this study, after completing the interventions and sampling, follow-up care was also provided by the project researchers for the control group. Also, this study had been approved by the Iranian Registry of Clinical Trials (IRCT20200112046102N1).
3.5. Statistical Analysis
Data were analyzed using SPSS version 16 through descriptive statistics (i.e., mean, standard deviation, and frequency) and inferential statistics (i.e., Wilcoxon, Repeated Measure ANOVA, and independent t-test). According to Kolmogorov-Smirnov (KS) test, we used parametric tests. Mann-Whitney test was used to compare the mean scores of pre-intervention and post-intervention mental health. Repeated measure analysis of variance (ANOVA) was used to assess the changes in mental health scores in each group. MANCOVA was also used to compare changes in mental health score before the intervention with one week and eight weeks after the discharge. Significance level of the tests was considered at P < 0.05.
4. Results
Overall, 80 mothers of children with CP were enrolled, who were divided into two groups of 40. The mean age of the mothers was 33.2 ± 2.1 years and 34.3 ± 2.2 years in the intervention and control groups, respectively, with a minimum age of 19 and a maximum age of 42 years. The majority of the mothers had an under diploma educational degree (the intervention group: 18 [45%]; the control group: 30 [75%]), and most of them had not participate in any child care educational programs (the intervention group: 32 [65%]; the control group: 30 [75%]). Other demographic characteristics of the mothers are presented in Table 2.
| Variables | Intervention | Control | P-Value |
|---|---|---|---|
| Age (y), mean ± SD | 33.2 ± 2.1 | 34.3 ± 2.2 | 0.09 |
| Participation in any child caring programs | 0.08 | ||
| Yes | 8 (35) | 10 (40) | |
| No | 32 (65) | 30 (60) | |
| Educational degree | 0.34 | ||
| Under Diploma | 18 (45) | 30 (75) | |
| Diploma | 12 (30) | 5 (12.5) | |
| Bachelor | 5 (12.5) | 5 (12.5) | |
| Higher educational degrees | 5 (12.5) | 0 | |
| Experiencing depression due to having a child with CP | 0.09 | ||
| Yes | 22 (46) | 20 (42) | |
| No | 28 (54) | 20 (58) | |
| Status of caring for the child | 0.33 | ||
| Providing care for the child by both parents | 35 (68) | 40 (100) | |
| Providing care for the child by one of parents | 5 (32) | 0 | |
| Having another child with CP | 0.55 | ||
| Yes | 10 (42) | 5 (28) | |
| No | 30 (58) | 35 (72) |
Demographic Characteristics of the Mothers a
Findings showed no significant relationship between demographic characteristics of the mothers and their mental health status. Based on Table 3, there was a significant difference in mental health score between before the intervention and one and eight weeks after discharge from the hospital in the intervention group (11.27 ± 11.84, 15.21 ± 10.63) and in the scores of the control group one and eight weeks after discharge (4.94 ± 9.25, 4.58 ± 10.84), respectively. These findings indicated that mothers' mental health score was changed in the intervention group at all stages significantly more than in the control group.
| Group/Data | Intervention Group, Mean ± SD | Control Group, Mean ± SD | P-Value | Statistical Test |
|---|---|---|---|---|
| Mental health (Pretest) | 56.52 ± 13.21 | 56.14 ± 10.44 | 0.664 | Mann-Whitney |
| Mental health (one week) | 44.95 ± 13.40 | 51.46 ± 11.39 | 0.034 | Mann-Whitney |
| Mental health (8 weeks) | 41.85 ± 12.01 | 51.45 ± 13.02 | 0.002 | Mann-Whitney |
| Difference between pre-intervention and 1-week posttest | 11.27 ± 11.84 | 4.94 ± 9.25 | 0.04 | Mann-Whitney |
| Difference between pre-intervention and 8-week posttest | 15.21 ± 10.63 | 4.58 ± 10.84 | 0.02 | Mann-Whitney |
| Difference between 1-week posttest and 8-week posttest | 4.35 ± 6.80 | 0.01 ± 6.28 | 0.014 | Mann-Whitney |
| P-value of the effect of time | 0.001 | 0.11 | Repeated measure ANOVA | |
| P-value of the effect of group | 0.09 | Repeated measure ANOVA | ||
| P-value of the interaction between time and group | 0.001 | Repeated measure ANOVA | ||
Comparison of the Mean Scores of Mental Health by Group and Time
In general, Repeated Measure ANOVA and ANCOVA showed that the mean scores of mothers' mental health at all stages of the intervention were significantly higher than those of the control group (P < 0.05; Table 4).
| Dependent Variables | Mean Difference | Std. Error | 95% Confidence Intermission | P-Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Difference between mental health scores of pre-intervention and 1-week posttest a | 4.629 | 2.130 | 0.376 | 8.883 | 0.033 |
| Difference between mental health scores of pre-intervention and 8-week posttest a | 7.538 | 1.979 | 3.578 | 11.494 | 0.001 |
| Difference between mental health scores of 1-week posttest and 8-week posttest a | 3.670 | 1.648 | 0.373 | 6.967 | 0.03 |
Difference in Mental Health Scores by Group and Time
5. Discussion
This is the first study in Iran to investigate the impact of the CCM on the mental health of mothers with children suffering from CP admitted to hospital. The results of this study showed that the use of CCM had a positive effect on the mental health of the samples. In this regard, we present the results of various studies that have been carried out on the use of the CCM. Based on a study by Otaghi et al. that was aimed at investigating the effect of continuous care model on the sleep quality of hemodialysis patients, it was found that using this method had a positive effect on the sleep quality of these patients undergoing hemodialysis (18).
According to a study by NasrAbadi et al., that was aimed at assessing the impact of CCM on the social health status of the families of patients undergoing coronary artery bypass graft surgery, it was found that the means of burden scores for the social domain were 3.86 before the intervention and 1.81 after the intervention. Also, in the five dimensions of care burden, the pattern of the CCM affected all dimensions of care burden and reduced the burden of care across all dimensions, with a significant decrease in the social domain (25). Based on a study by Kamali et al., it was found that the use of the CCM had a positive effect on the sleep quality of the elderly and recommended the widespread use of this intervention (26). Another study by Okhovat et al. was aimed to investigate the impact of using the CCM on the anxiety of mothers with children undergoing surgery. It was found that the CCM had positive effects in reducing the anxiety of mothers of hospitalized children (8). Based on the results of the present study, the use of CCM does not require a great amount of time for nurses, and they could easily use this care method to provide and follow-up effective training for mothers of children with CP. Since mothers of children with CP play the most central role in providing care for them and can be affected by long-term mental and physical burnout, the present study introduced the use of the CCM as a convenient and accessible method that nurses could apply. It could be used to enhance the quality of mental health in mothers of these children. Also, CP is a chronic and debilitating disease for children and families. Due to the main role of mothers in providing care for their children, in the long-term, they would be subjected to a great deal of physical and psychological stress that requires special attention. In this regard, nurses could use the CCM to reduce the mental stress of mothers of these children. In order to make the idea of using the CCM more applicable, we suggest to train nurses about the CCM so that this program could be provided to parents through booklets or as mobile messenger applications. In this study, due to the lack of facilities, the follow-up period for the care program was up to eight weeks after discharge from the hospital; it is recommended that long-term follow-ups be designed and implemented in future studies to ensure the long-term effects of this program.
5.1. Limitations
One of the limitations of the present study was the mental state of the mothers when completing the questionnaire, which might affect the results of the research and cannot be controlled. Also, the long intervention period and lack of cooperation from some of the mothers were other limitations of the present study. Thus, in order to encourage more mothers during this two-month period and reduce the loss of samples in the follow-up period, at the end of each session, a gift was given to the children of the participants to increase their desire to participate in the study. Also, during the two-month period, counseling and follow-up were performed repeatedly through WhatsApp messaging and phone calls.