1. Background
In 2008, the world health organization (WHO) estimated that 35% of adults aged above 19 years were overweight and that 10% of males and 14% of females were obese (1). For the first time, Vague et al., reported that people with more fat accumulation in the upper body than the lower body were more likely to be disposed to metabolic syndrome. There are variations in body fat distribution on the basis of gender and age (2). In both females and males, aging is associated with somatic changes such as decrease in body stature and increase in fat tissue (3). Generally, males have greater total lean mass and bone mineral mass and females have more total adipose tissue and fat mass (4).
One of the popular indicators of developing serious health conditions in human is the waist-to-hip ratio (WHR) (2). The WHR is used to assess abdominal obesity (5), which is affected by gender, regardless of age and ethnicity (6-9). The WHR is simple, fast, and inexpensive (10).
The WHR is used in many studies to assess its relationship with different variables such as cholesterol, triglyceride, diabetes status, heart disease, mortality, and obesity; it owes its creation to American and European studies (7-9). According to the US Department of Health and Human Services (US-DHHS), the WHR cutoff points to detect obesity are ≥ 0.95 and ≥ 0.80 for males and females, respectively; ≥ 1.0 and ≥ 0.85, according to the WHO (8, 11-13). These cutoff points may not be appropriate for other nations (2, 6); for example, the suitable WHR cutoff point for American males is 0.95, for European males ≥ 1.00, and > 0.91 to < 0.92 in Arabian studies (13-15).
The current study aimed at determining the optimal WHR cutoff points for Iranian adults, and the secondary purpose was comparing the results with those of other Asian groups and 2 standard procedures. The WHO gold standard cutoff points were used to detect obesity. Body composition measures were determined by the bioelectrical impedance analysis method (BIA).
2. Methods
The current cross sectional study was approved by the ethical committee of the Vice Chancellor for research and technology at Hormozgan University of Medical Sciences, Hormozgan province, Bandar Abbas, Iran. The prevalence of obesity in Iran is 21.5% (16), which was used to estimate the minimum sample size as 6483 at the 0.05 level of significance to test non-directional hypotheses. The data were collected from 2009 to 2014. There were 23 300 individuals who voluntarily agreed to participate in the study. All subjects signed the written consent form. The data collection and the implementation of the BIA were explained to all participants by the research team. The subjects who were < 20 and > 70 years old, had pacemakers, were pregnant, had the history of hospitalization at least 3 months prior to data collection, and had a negative fat free mass (FFM) were excluded from the study. The 16 341 adults who met the inclusion criteria were classified on the basis of age into 4 groups: 20 to 29, 30 to 39, 40 to 49, 50 to 59, and 60 to 70 years old.
The BIA was performed, using the body composition analysis device, Plusavis 333 (JAWON Medical Company). This device uses the frequencies ranged from 50 to 250 kHz, is affordable, and is not invasive (17, 18). The comparison of this method with X-ray showed that it accurately assessed body composition (19-21). By this method, WHR, BMI, the percentage of body fat (PBF), total fat (TF), and FFM were measured, using the standard positions of outer and inner electrodes on the hand and foot (8 electrodes) (22, 23). Body height in centimeter (cm) was measured to the nearest 0.5 cm by a stadiometer. All measurements were done by professional technicians.
The WHO defines the gold standards of obesity as the PBF >25% in males and > 35% in females (24). The classification of the subjects based on WHR was < 0.90 (normal), 0.90 to 0.99 (overweight), and ≥ 1 (obese) for males; and < 0.80 (normal), 0.80 to 0.84 (overweight), and ≥ 0.85 (obese) for females (13). The subjects were classified as with obesity or without obesity.
The statistical package for the social sciences (SPSS) version 22 was used to manipulate and analyze data, which included contingency tables, and the statistical analyses of the data included the Pearson correlation coefficients to examine the relationship between PBF and various proxy measurements. Sensitivity, specificity, positive predictive power (PPV), and negative predictive power (NPV) were computed. Receiver-operating characteristic (ROC) curves were used to assess the diagnostic performance of the screening test and its accuracy, or the ability to correctly classify subjects into clinically relevant subgroups, as defined by a reference test (25). The areas under the curve (AUC) and associated 95% confidence intervals (CI) were compared. The larger the AUC, the more accurate was the test. A P value < 0.05 was considered statistically significant. To determine the best cutoff points for WHR based on the obesity in subjects, the shortest distance between any point on the ROC curve and the top left corner of the y-axis, except ROC curves for each variable, and the associated AUC (26) were plotted, and the James et al. formula (27) was employed to compare the 2 ROC curves.
3. Results
The study participants were 11 758 females and 4583 males. Females’ measures were lower than those of males in height, weight, WHR, and FFM, but higher in PBF and TF (P value < 0.01). Results are summarized in Table 1.
| Gender | Mean | SD | P Value | |
|---|---|---|---|---|
| Age | Female | 35.2 | 10.2 | < 0.01 |
| Male | 35.9 | 10.4 | ||
| Height | Female | 159. | 5.8 | < 0.01 |
| Male | 173. | 6.5 | ||
| Weight | Female | 75.7 | 14.1 | < 0.01 |
| Male | 90.9 | 17.9 | ||
| WHR | Female | 0.85 | .05 | < 0.01 |
| Male | 0.92 | .06 | ||
| PBF | Female | 36 | 4.5 | < 0.01 |
| Male | 27.5 | 5.1 | ||
| FFM | Female | 11.1 | 8 | < 0.01 |
| Male | 12.3 | 9 | ||
| TF | Female | 27.7 | 8.3 | < 0.01 |
| Male | 25.6 | 9.2 |
Abbreviations: FFM, fat free mass; PBF, percent body fat; TF, total fat; WHR, waist-to-hip ratio.
There were 12 297 participants with obesity based on the US-DHHS criteria. On the basis of WHR, there were 6705 persons with obesity. The WHO gold standards showed that 10 061 participants had obesity.
3.1. The US-DHHS Classifications; All Males
The sensitivity and NPV were 48.9% and 47.9%, respectively. By this classification, half of the subjects with obesity were wrongly classified as without obesity. The specificity and PPV indices were 99%.
3.2. The US-DHHS Classifications; Males by Age-Groups
In males younger than 40 years, the sensitivity and NPV were less than 40%. By this classification, nearly 80% of males with obesity within the age range of 20 to 39 years and 63% of males with obesity within the age range of 30 to 40 years were wrongly classified as without obesity. With increase in age after 39 years, both sensitivity and NPV increased. After the age of 49 years, this classification correctly identified more than 78% of the subjects with/without obesity. In the age range of 50 to 60 years, the accuracy of the classification was more than 96.8%.
3.3. WHO-WHR Classifications; All Males
The sensitivity was 21.3%. By this classification, more than 78% of the subjects with obesity were wrongly classified as without obesity. The specificity and PPV were 100%.
3.4. WHO-WHR Classifications; Males by Age-Groups
More than 63% of the subjects with obesity who were under 50 years were wrongly classified as without obesity. Increase in age was associated with increased accuracy, but not higher than 69%. In all age groups, the specificity and PPV were 100%.
3.5. The US-DHHS Classifications; All Females
The sensitivity and NPV were 100%, but specificity was 20.8%. By this classification, 3818 females without obesity were wrongly classified as with obesity.
3.6. The US-DHHS Classification; Females by the Age Group
The sensitivity and NPV were 100% in all age groups. With increase in age, the specificity and NPV decreased. All females above 59 years were classified as obese.
3.7. The WHO-WHR Classifications; All Females
On the basis of this indicator, more than 80% of the females with and without obesity were correctly classified.
3.8. The WHO-WHR Classifications; Females by Age Groups
With increase in age, the sensitivity and NPV increased in all age groups. In the subjects above 49 years, the sensitivity and NPV were 100%. After the age of 29 years, more than 81% of the subjects with and without obesity were correctly classified.
In summary, the sensitivity and NPV in both classifications were higher in females compared to males. For females and males in both classifications, increase in age was associated with increase in the sensitivity and NPV. Generally, the WHO classification was the worst indicator of obesity in males. The US-DHHC was the best to correctly classify the obesity or non-obesity in the subjects of various age groups (Table 2).
| Age Group | Overweight | Obese | Sensitivity | Specificity | PPV | NPV | ||
|---|---|---|---|---|---|---|---|---|
| N | N | % | % | N | % | N | % | |
| US Male | 3039 | 1544 | 48.9 | 99 | 1529 | 99 | 1442 | 47.4 |
| US: 20 - 30 | 1219 | 205 | 20.9 | 100 | 205 | 100 | 444 | 36.4 |
| US: 30 - 40 | 1256 | 432 | 36.8 | 100 | 432 | 100 | 513 | 40.8 |
| US:40 - 50 | 376 | 541 | 87.3 | 100 | 541 | 100 | 297 | 79 |
| US: 50 - 60 | 153 | 264 | 100 | 96.8 | 259 | 98.1 | 153 | 100 |
| US: 60 - 70 | 35 | 102 | 100 | 77.8 | 92 | 90.2 | 35 | 100 |
| WHO Male | 3916 | 667 | 21.3 | 100 | 667 | 100 | 1457 | 37.2 |
| WHO: 20 - 30 | 1338 | 86 | 8.8 | 100 | 86 | 100 | 444 | 33.2 |
| WHO: 30 - 40 | 1540 | 148 | 12.6 | 100 | 148 | 100 | 513 | 33.3 |
| WHO: 40 - 50 | 692 | 225 | 36.3 | 100 | 225 | 100 | 297 | 42.9 |
| WHO: 50 - 60 | 272 | 145 | 56 | 100 | 145 | 100 | 158 | 58.1 |
| WHO: 60 - 70 | 74 | 63 | 68.5 | 100 | 63 | 100 | 45 | 60.8 |
| US Female | 1005 | 10753 | 100 | 20.8 | 6935 | 64.5 | 1005 | 100 |
| US: 20 - 30 | 700 | 3376 | 100 | 34.7 | 2060 | 61 | 700 | 100 |
| US: 30 - 40 | 266 | 3884 | 100 | 15.3 | 2407 | 62 | 266 | 100 |
| US:40 - 50 | 32 | 2113 | 100 | 4.5 | 1434 | 67.9 | 32 | 100 |
| US: 50 - 60 | 6 | 1145 | 100 | 2 | 855 | 74.4 | 6 | 100 |
| US: 60 - 70 | 1 | 236 | 100 | 1.8 | 179 | 76.2 | 1 | 100 |
| WHO Female | 5720 | 6038 | 84.1 | 95.8 | 5835 | 96.6 | 4620 | 80.8 |
| WHO: 20 - 30 | 2705 | 1371 | 66.6 | 100 | 1371 | 100 | 2016 | 74.5 |
| WHO: 30 - 40 | 2142 | 2008 | 83.4 | 100 | 2008 | 100 | 1743 | 81.4 |
| WHO: 40 - 50 | 668 | 1477 | 99.2 | 92.3 | 1422 | 96.3 | 656 | 98.2 |
| WHO: 50 - 60 | 176 | 975 | 100 | 59.5 | 855 | 87.7 | 176 | 100 |
| WHO: 60 - 70 | 29 | 207 | 100 | 50.9 | 179 | 86.5 | 29 | 100 |
3.9. Suitable WHR Cutoff Points
The suitable cutoff points to detect obesity among Iranian males and females were 0.89 and 0.83, respectively. In Comparison with US-DHHS, the recommended WHR cutoff points were 0.95 and 0.80 for males and females, respectively; the indices for Iranians were 0.06 lower and 0.03 higher, respectively. In Comparison with the WHO’s estimations of 1.0 and 0.85 for males and females respectively, the current study results were 0.11 and 0.02 lower, respectively.
The suitable cutoff points for males in all age groups were lower compared to those of WHO. However, age group comparisons with US-DHHS showed that males under 49 years had lower cutoff points, but for the ones above 49 years the estimations were the same. In short, for the Iranian adult males, the US-DHHS cutoff points were better than those of WHO to detect obesity.
For the Iranian females of all age groups, the current study results were higher than those of US-DHHS. Among the subjects above 39 years, the results were similar to those of WHO. In all age groups, increase in age was associated with increase in cutoff points to detect obesity. In short, the WHO cutoff points were better than those of the US-DHHS to detect obesity in Iranian females.
Among all subjects, increase in age was associated with increase in the WHR cutoff points. In males, the estimates ranged from 0.84 to 0.95; however, it was 0.82 to 0.86 in females (Table 3).
| Age Group | AUCa | Cutoff | Sensitivity and Specificity | Difference with US-DHHS | Difference with WHO |
|---|---|---|---|---|---|
| 20 - 29 Male | 0.98 | 0.84 | 0.92, 0.99 | -0.11 | -0.16 |
| 30 - 39 Male | 0.91 | 0.90 | 0.68, 0.99 | -0.05 | -0.10 |
| 40 - 49 Male | 0.99 | 0.93 | 0.94, 0.96 | -0.02 | -0.07 |
| 50 - 59 Male | 0.99 | 0.95 | 0.95, 0.99 | 0.00 | -0.05 |
| 60 - 70 Male | 0.99 | 0.95 | 0.96, 0.91 | 0.00 | -0.05 |
| 20 - 29 Female | 0.98 | 0.82 | 0.86, 0.95 | + 0.02 | -0.03 |
| 30 - 39 Female | 0.99 | 0.83 | 0.92, 0.98 | +0.03 | -0.02 |
| 40 - 49 Female | 0.99 | 0.85 | 0.96, 0.99 | +0.05 | 0.001 |
| 50 - 59 Female | 0.99 | 0.86 | 0.97, 0.99 | +0.06 | +0.01 |
| 60 - 70 Female | 0.99 | 0.86 | 0.99, 0.99 | +0.06 | +0.01 |
aAUC, area under the curve.
3.10. Correlational Results
Analysis of the data showed positive correlation between age and WHR in females (r = 0.46, P value < 0.01) and in males (r = 0.55, P value < 0.01). Additionally, the association between WHR and PBF in females (r = 0.92, P value < 0.01) and males (r = 0.75, P value < 0.01) were statistically significant. None of the other associations were statistically significant.
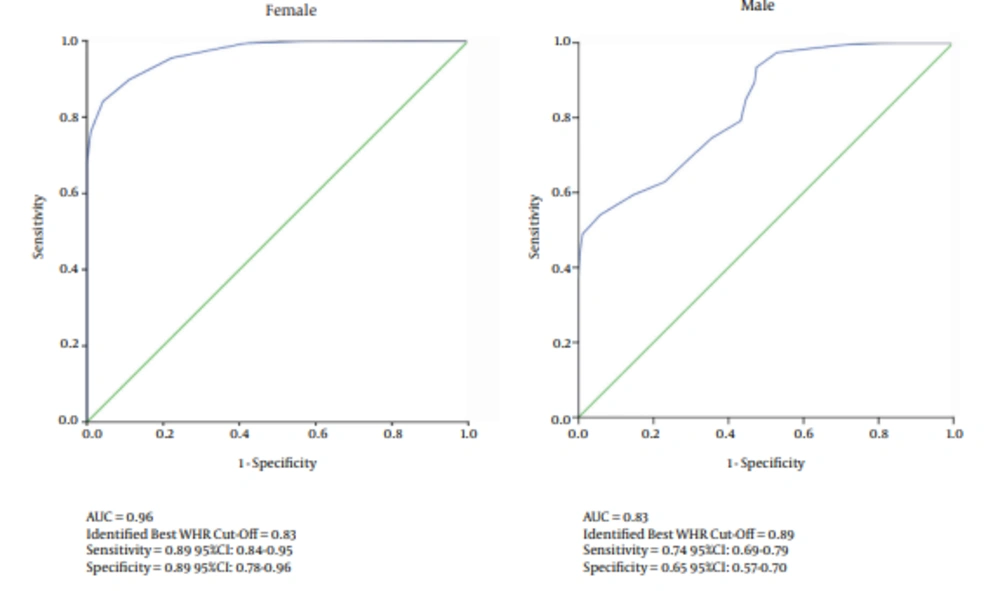
3.11. ROC Results
The ROC curves for obesity in females and males are shown in Figure 1. The area under the curve (AUC) reflects the probability that a random person with obesity has a higher value of the measurement than a random person without obesity (28). A total of 6935 females and 3126 males were classified as the positive group (with obesity); in addition, 4823 females and 1457 males were then classified as the negative group (without obesity). The probability to detect obesity by AUC was higher in females than males. The AUC for females and males were 0.97 and 0.83, respectively; and the difference was statistically significant (P value < 0.01) (Figure 1).
4. Discussion
The purpose of the study was 2-fold: 1) To obtain suitable WHR cutoff points for the Iranian adults, and 2) To compare the results with those derived on the basis of US-DHHC, WHO-WHR, and documented Asian studies. Results showed that WHR cutoff points for males were close to those obtained based on the US-DHHS; for females, they did not differ much from those obtained on the basis of WHO gold standards. Both standard cutoff points were weak to distinguish between males with and without obesity, especially among the ones under 40 years old.
Correlational analyses of the data showed that WHR had stronger correlations with PBF in females than males as well as stronger sensitivity and NPV in both classifications.
Aging is associated with somatic changes (9), and was considered in the formulation of WHR, US-DHHS, and WHO gold standards, which could make it a confounding variable by affecting the results (4). For example, in a study on weight-loss, the type of diet prior to the intervention can be a confounding variable by affecting the outcome. In the current study, the strong positive correlation between age and WHR were observed in both genders. On the other hand, in both classifications, increase in age was associated with increase in sensitivity and NPV in females and males.
In both classifications, WHR had a low rate of true negative among the males aged between 20 and 39 years. In this age group, the US-DHHS and WHO specifically missed nearly 60% and 66% of the subjects with obesity, respectively. These indicators could not distinguish between the young males with and without obesity. These findings were supported by Romero’s study (12). The sensitivity, specificity, NPV, and PPV, based on WHR in both classifications, were high among females, attesting to its classification power to diagnose obesity in females. Originally, both classifications were developed based on data from American and European populations (29), which may not be suitable for other populations (7). Thus, the results of the current study were compared with those of the Middle-East and Southeast Asia.
Mirmiran (30) estimated the range of the WHR cutoff points among Iranian adults in 3 age groups of 18 to 34, 35 to 54, and 55 to 74 years with at least 1 cardiovascular risk factor, as 0.86 to 0.94 and 0.78 to 0.90 for males and females, respectively. To compare the results with those of the current study, the participants were classified into the same age groups, and the obtained results were 0.84 to 0.95 and 0.82 to 0.86 for males and females, respectively. The findings showed the same range in males, but not females. The difference in females’ findings could have been due to the AUC difference. In Mirmiran’s study, the range of AUC for females was very low (0.59 to 0.65), but very high (0.98 to 0.99) in the current investigation. The larger AUC indicates higher accuracy (25); such results were not observed in males.
In another Iranian study, the suitable WHR cutoff point for the Iranian elderly males was reported 0.95 (31). On the basis of the current study data, the estimate of the index was 0.96. These findings suggested that the WHR cutoff point to detect obesity among elderly males in Iran was less than that of the Europeans (≥ 1.00).
In the current study, the suitable WHO cutoff points for menopausal females above 39 years were 0.85 to 0.86. A similar finding was reported in another Iranian study (32) (WHR = 0.84, 778 subjects). This finding was also similar to the US-DHHS cutoff points.
A comparison of the current study results with those of 2 Arabian studies, one in Oman (15) (WHR = 0.91 in both genders; 1421 subjects) and another in Iraq (33) (WHR = 0.92 in males and 0.91 in females; 12 986 subjects) showed that the estimated WHR cutoff points for males were similar in the 3 studies, but not those of females. Why? Because, obesity was more prevalent in Arab females compared with Iranian females. For example, the prevalence of obesity in females was 44% in Jordan, 41% in Kuwait, and 66% in Saudi Arabia (34); it was 25.2% in Iranian females (35). Additionally, obesity was more prevalent in Arab females under 40 years old (31). In the current study, females under 40 years old had lower WHR cutoff points and lower prevalence of obesity than the females in older age groups. These differences were not observed in males.
Studies investigating body composition in Asia focused on Chinese, Japanese, Korean, and Indian populations. A number of studies examined these ethnic groups as a homogeneous population, labelled Asians, and reported a higher percentage of body fat than Caucasians (36). Some of these studies in Southeast Asia reported suitable WHR cutoff points. Huxley et al., reported 0.90 in males and 0.80 in females (133 405 subjects with diabetes or taking anti-glycemic drugs) (37). Obesity in Asia is reported 0.92 and 0.84 in males and females, respectively (107 700 subjects) (38). Deurenberg-Yap et al., estimated 0.90 in males and 0.80 in females (4723 subjects) (39) and Ko et al., reported 0.88 in males and 0.80 in females (1513 subjects in Hong Kong) (40). In such Asian studies, the suggested range for the WHR cutoff points was 0.85 to 0.92 in males, and 0.76 to 0.84 in females. With the exception of the study by Lin et al., the current study results were similar to other findings.
In spite of the large sample size, it should be noted that the current study participants were recruited from South of Iran and could not be attributed to the total population of Iran. It is recommended to replicate the study in other regions of Iran to enhance the generalizability of the results.
4.1. Conclusions
Increase in age is associated with increase in correct detection of obesity. Both WHO-WHR and US-DHHS classifications effectively detected obesity among all females. Neither effectively detected obesity among males under 40 years old. Among males above 40 years old, the US-DHHS was effective to detect obesity. The suitable cutoff points for the Iranian males and females were 0.88 and 0.83, respectively; similar to the ones reported in Southeastern Asian studies. The recommended cutoff point for the Iranian males was similar to that of the Arab males; but the one for Iranian females was different from that of Arab females.