1. Context
The thyroid gland is the maestro of the endocrine system, orchestrating the body's metabolism through its hormonal "batons." Located at the front of the neck, this butterfly-shaped gland primarily produces triiodothyronine (T3) and thyroxine (T4), two hormones that impact all tissues. Additionally, it secretes calcitonin, a hormone responsible for maintaining calcium homeostasis. The thyroid's function is regulated by the hypothalamic-pituitary-thyroid axis, where the hypothalamus releases thyrotropin-releasing hormone (TRH), and the pituitary gland secretes thyroid-stimulating hormone (TSH) to stimulate thyroid activity (1). Disruptions in the regulation, production, or secretion of these hormones can lead to adverse physiological effects. The most common thyroid function disorders are hyperthyroidism and hypothyroidism. Hyperthyroidism is caused by the overproduction of thyroid hormones, while hypothyroidism results from insufficient hormone production. Numerous factors contribute to these conditions, affecting a significant proportion of the global population (2, 3).
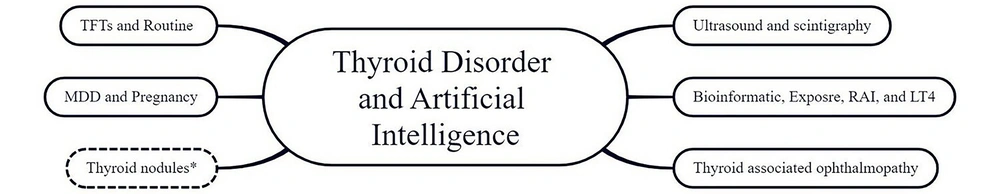
Integrating artificial intelligence (AI) into various medical fields holds the potential to revolutionize the diagnosis, monitoring, and management of thyroid function disorders (Figure 1). The initial attempts at computer-assisted diagnosis (CAD) in this domain date back to 1963, when probability matrices were employed to differentiate between the diverse etiologies of thyroid dysfunction using clinical and laboratory data (4). With the continuous evolution of AI technologies, there is an increasing capacity to improve healthcare resource efficiency, support clinical decision-making, provide personalized recommendations and treatments, and enhance understanding of complex thyroid pathologies by leveraging vast datasets (5). In this review, we aim to present a comprehensive overview of various AI applications in addressing thyroid function disorders, rather than focusing on a detailed examination of a single area.
2. Evidence Acquisition
We crafted search queries by combining a diverse array of MeSH terms: “artificial intelligence,” “machine learning,” “deep learning,” “thyroid gland,” “thyroid hormones,” “thyroid diseases,” “hyperthyroidism,” “hypothyroidism,” “thyroiditis,” “Graves’ disease,” “diagnosis,” and “thyroid function test.” These queries were used to conduct an extensive search in PubMed and Google Scholar online databases to collect full-text available human original studies, systematic reviews, and meta-analyses on the applications of AI in thyroid function disorders, published in English from January 2014 to May 2024. Various types of studies were included in this review to deepen the understanding of multiple aspects of the topic and study methodologies. Studies published in the last decade were included because the application of AI in the field of thyroid diseases has recently gained significant attention, and we aimed to gather the most up-to-date literature in this field. Our search covered titles and abstracts to ensure a broad exploration of relevant literature. After screening the titles and abstracts, a number of studies aligned with our research focus were selected to provide this narrative review.
Key artificial intelligence (AI)-powered applications in thyroid disorders. The “*” symbol indicates that the application of AI in the management of thyroid nodules is not explored in the current study, although it is addressed in a separate survey conducted by the authors (5).
3. Results
Physicians may utilize an approach involving patient history, physical examination, laboratory testing, imaging studies, and biopsies to diagnose thyroid disorders. Diagnosing thyroid function diseases is challenging due to the broad spectrum of non-specific clinical presentations, such as weight changes, exhaustion, memory and cognitive issues, muscular pain, etc. Furthermore, it is essential to note that some patients, for instance elderly people, may not always display evident clinical symptoms (6, 7).
Thyroid function tests (TFT) are frequently utilized to diagnose thyroid function disorders, comprising blood tests for TSH, total and free T3 and T4, and T3 resin uptake (T3RU). In certain instances, anti-thyroid antibodies like thyroid peroxidase antibodies (TPO-Ab) and TSH receptor antibodies (TR-Ab) may also be considered. Thyroid-stimulating hormone level assessment through immunoassay is the most prevalent initial screening method for thyroid dysfunction (8). However, it is susceptible to various confounding factors and may not always precisely reflect the actual thyroid gland function status (9). Artificial intelligence can offer new opportunities to enhance accuracy, efficiency, and patient care quality within thyroid laboratory testing.
3.1. Thyroid Function Test and Routine Clinical Laboratory Data
First, AI can improve TFT immunoassay designs and mitigate the impact of confounding variables through in-silico modeling (10). Utilizing machine learning (ML) technologies is promising for transforming molecular identification methods for diagnosing thyroid function disorders. For instance, the deployment of a least squares support vector machine (LS-SVM) trained by biomolecular features extracted from serum TSH infrared spectroscopy data demonstrated a resilient capability to accurately assess a broad spectrum of blood TSH levels (11). Furthermore, by analyzing medical records and clinical datasets, ML presents opportunities to customize reference ranges and diagnostic thresholds for TFTs according to physiological variations in hormone levels. A study has indicated that ML has the potential to enhance the automated verification process of TFT results (12).
Second, AI can aid in diagnosing thyroid function disorders by integrating overall health conditions, clinical evaluations, and the interpretation of TFT results. With advancements in natural language processing (NLP) technologies, a study assessed the proficiency of ChatGPT and Google Bard in interpreting TFT results. The findings revealed that the precision and reliability of these chatbots fall short of the standards required for clinical application, confirming that they are not yet suitable substitutes for professional medical consultation (13).
Numerous studies have investigated ML and deep learning (DL)-based predictive and interpretative models for classifying thyroid dysfunctions. These models have been trained on various exclusive or publicly available thyroid disease datasets, primarily those from the University of California Irvine (UCI) repository (14-20). Generally, ML models have demonstrated superior performance compared to DL models, primarily due to the limitations in the size and features of datasets used for training DL models (15). Conducting a comparative assessment of the performance of different ML models is challenging due to the significant heterogeneity in model frameworks and training/testing datasets. However, based on our review, decision trees, random forests, and artificial neural networks have shown higher effectiveness in interpreting and categorizing TFT. Table 1 provides the performance metrics of the best-performing models from the included studies.
| First Author, Year, Reference | Aim | Technique | Dataset | Sample Size | Performance Metrics |
|---|---|---|---|---|---|
| Cheng et al., 2022 (16) | Diagnosis of thyroid dysfunction from thyroid datasets (TFT) | DT, LR, XGB, and SVM | 21 features, including TFT | 11565 Nl and 1170 elevated TSH from 1 center | XGB: AUC 0.87, and ACC 0.86 |
| Islam et al., 2022 (17) | Same | CatB, Extra-Trees, ANN, LGBM, SVC, KNN, RF, XGB, DT, and GaussianNB | UCI sick-euthyroid dataset (25 features) | 2870 sick and 292 Nl | ANN: F1-score 0.957, precision 0.957, recall 0.959, and ACC 0.9587 |
| Abbad Ur Rehman et al. 2021 (19) | Same | KNN, NB, SVM, LR, and DT | DHQ Teaching Hospital thyroid dataset (10 features) | 170 Nl, 66 hyper, and 73 hypo | NB: ACC 100%, recall 100%, and F1-score 100% |
| Rasitha, 2016 (14) | Same | LDA | UCI hypothyroid dataset (29 features) | 3481 Nl, 194 compensated hypo, 95 primary hypo, and 2 secondary hypo | Precision 0.996, recall 0.996, ACC 99.62, and ROC 0.996 |
| Yadav and Pal, 2020 (20) | Same | DT, RF, CART, and bagging ensemble model | UCI thyroid disease dataset (30 features) | 3710 patients (2 classes) | Bagging ensemble model: ACC 100% |
| Chaganti et al., 2022 (15) | Same | RF, LR, SVM, ADA, GBM and CNN, LSTM, and CNN-LSTM | UCI thyroid disease dataset (30 features) | 233 primary hypo, 359 compensated hypo, 346 increasing binding proteins, 456 concurrent non-thyroidal illness, and 400 Nl | RF: F1-score 0.99, precision 0.99, recall 0.99, and ACC 0.99 |
| Mir and Mittal, 2020 (18) | Same | Boosting, bagging, NB, SVM, and J48 | 21 features, including TFT | 489 Nl, 488 hyper, and 487 hypo from 1 center | SVM: ACC 99.08, precision 0.991, recall 0.991, and ROC 0.994 |
| Yoshimura Noh et al., 2024 (21) | Diagnosis of thyroid dysfunctions from routines | ANN (Prediction one) and LR | JHEP (11 features), JND (9 features), and Ito (32 features) datasets including routine lab | 20653 GD, 3435 painless thyroiditis, 4266 Nl, and 18937 HT from 1 center | Thyrotoxicosis: AUC 0.977 Hypothyroidism: AUC 0.877 |
| Hu et al., 2022 (22) | Same | GBDT, SVM, LR, and ANN | EMRs (23 features, including routine lab) | 176727 patients from 4 centers | Hyperthyroidism: AUC 93.8% Hypothyroidism: AUC 90.9% |
| Ghali et al., 2020 (23) | Prediction of TSH by macroelements and vitamins | ANFIS, ANN, and MLR | 7 vitamins and macronutrients | Blood sample of 1 patient | ANFIS: R2 0.914 |
| Shin et al., 2023 (24) | Detection of hyperthyroidism | LGB | 662 pairs of TFT and HR | 175 patients (2 classes) from 1 center | Sensitivity 86.14%, specificity 98.28%, NPV 95.32, and PPV 94.57% |
| Choi et al, 2022 (25) | Same | DL | 174331 ECGs for training, 48648 for external validation | 146672 patients from 2 centers | AUC 0.926 for internal validation and AUC 0.883 for external validation |
Abbreviations: DT, decision tree; LR, logistic regression; XGB, X gradient boosting; SVM, support vector machine; CatB, CatBoost; ANN, artificial neural network; GaussianNB, Gaussian naive bayes; LGBM, light gradient-boosting machine; SVC, support vector classifier; KNN, K-nearest neighbors; RF, random forest; LDA, linear discriminant analysis; CART, classification and regression tree; BP-AdaBoost, back propagation-adaptive boosting; CNN, convolutional neural network; ANFIS, adaptive neuro-fuzzy inference system; MLR, multiple linear regression; ADA, AdaBoost; GBM, gradient boosting machine; LSTM, long short-term memory; DL, deep learning; NL, normal; AUC, area under curve; ACC, accuracy; TFT, thyroid function tests.
Most studies have concentrated on evaluating the performance of ML models in binary classification (e.g., illness versus normal) of thyroid function status. Multi-class categorization remains more challenging due to the limited data available for minority classes. To address this issue, researchers have employed two strategies to manage imbalanced datasets: Oversampling, which involves augmenting minority class instances by generating synthetic samples or duplicating existing ones (17), and under-sampling, which reduces the majority class instances to match the minority class size (15).
A promising future direction involves fostering collaborative efforts across multiple institutions to pool datasets, creating comprehensive and diverse datasets that ensure better model generalization and performance.
On the other hand, it is important to acknowledge that while extensive datasets provide a wealth of training data, they can potentially hinder model performance when dealing with low-quality or complex data. In such cases, data pre-processing techniques, such as data cleaning, normalization, and feature engineering, are commonly employed to enhance model efficacy (14). Mir and Mittal demonstrated that the accuracy of thyroid disease classifiers improved after excluding laboratory features from the training dataset (18). Specifically, a support vector machine (SVM) classifier achieved an accuracy of 99.08% in predicting thyroid disorders within testing cohorts using only patient history and physical evaluations, eliminating the need for laboratory-based tests. By contrast, a bagging classifier trained on the original dataset, including laboratory results, achieved an accuracy of 98.56%. Although feature selection through DL requires greater computational resources and is costlier, it holds significant promise for enhancing future model performance.
Research has also explored identifying the most valuable predictors and detectors of thyroid dysfunction, extending beyond traditional TFTs to include routine clinical laboratory data and supplementary diagnostic methods (21, 22, 24, 25). For example, an ML model was developed to analyze the effects of various micronutrients and vitamins on TSH hormone regulation. The study revealed a direct correlation between TSH concentration and vitamin B9 levels, along with a slightly negative association with magnesium levels (23). Future research should prioritize identifying potential molecules that contribute to the onset of thyroid dysfunction, enabling timely diagnosis and preventive measures, such as dietary iodine supplementation.
In another study, a DL algorithm was developed using diverse electrocardiograms (ECG) to detect subclinical and overt hyperthyroidism, achieving an area under the curve (AUC) of 0.926 for internal validation and 0.883 for external validation. However, the inherent complexity and lack of transparency in the decision-making processes of DL models—commonly referred to as the "black box" problem—may compromise the generalizability and reliability of their results (25). To enhance reliability and clinical applicability, future research should focus on developing explainable AI systems. These systems can provide greater insight into the decision-making processes of DL-based models, ensuring transparency. Additionally, validation using real-world patient cohorts and comparative studies with expert physicians are essential to establish trust and efficacy.
3.2. Ultrasound and Scintigraphy
In the diagnosis of thyroid function disorders, thyroid scintigraphy plays a pivotal role in providing valuable insights into the secretory activity of the thyroid gland. However, accurate interpretation of thyroid scintigraphy heavily relies on the expertise of nuclear medicine specialists and is notably time-consuming (26). Given the promising performance of DL in medical imaging analysis, several studies have integrated DL networks to diagnose and differentiate various thyroid functional states using scintigraphy (27-30) (Table 2).
| First Author, Year, Reference | Aim | Technique | Dataset | Sample Size | Performance Metrics |
|---|---|---|---|---|---|
| Acharya et al., 2014 (31) | Diagnosis of thyroid dysfunctions | SVM, DT, fuzzy classifier, and KNN | 7 features from US images | 232 Nl and 294 HT from 1 center | Fuzzy classifier: ACC 84.6% |
| Zhang et al., 2022 (32) | Same | DL | Features from US images, US videos, and 6 features of TFT | 37424 HT and 69089 Nl from 1 hospital | By US videos + TFT: AUC 0.949 and ACC 0.892 |
| Zhao et al., 2022 (33) | Same | DL | Features from US images | 20666 HT and 18613 non-HT from 2 centers | Acc 0.892, AUC 0.940, and F1-score 0.892 |
| Vasile et al., 2021 (34) | Same | DL | Features from US images | 767 autoimmune, 672 micro-nodular, 720 nodular, and 638 Nl from 4 centers | Acc 98.78, and AUC 0.98 |
| Qiao et al., 2021 (28) | Same | DL | 1430 thyroid scintigraphies | 175 NL, 834 GD, and 421 subacute thyroiditis from 1 center | Subacute thyroiditis: F1-score 84.98 %, precision 77.99%, recall 93.33%, and ACC 89.00% GD: F1-score 88.62 %, precision 93.36%, recall 84.33%, and ACC 92.78% |
| Yang et al., 2021 (30) | Same | DL | 3389 thyroid scintigraphies from 3 centers | 4 classes of scintigraphy pattern | Overall ACC 92.73%, |
| Zhao et al., 2023 (29) | Same | DL | 3194 thyroid SPECT | 742 Nl, 808 GD, 826 subacute thyroiditis, and 818 tumors from 3 centers | Subacute thyroiditis: F1-score 0.958, recall 93.9, precision 97.6, and AUC 0.992 GD: F1-score 0.981, recall 100.0, precision 96.3, and AUC 0.999 |
| Kikuchi et al., 2023 (27) | Same | LGBM | 7013 F-18 FDG PET/CT scans | 182 hypo, 265 hyper, and 6566 Nl from 1 center | Hypothyroidism: AUC 0.77 Hyperthyroidism: AUC 0.78 |
Abbreviations: SVM, support vector machine; DT, decision tree; DL, deep learning; KNN, K-nearest neighbors; US, ultrasound; HT, hypothyroidism; TFT, thyroid function tests; SPECT, single-photon emission computed tomography scan; GD, Graves' disease; LGBM, light gradient boosting machine; F-18 FDG PET/CT, fluorine-18 fluorodeoxyglucose positron emission tomography; NL, normal; AUC, area under curve; ACC, accuracy.
Kappa coefficient metrics for DL convolutional neural networks (DCNNs) have demonstrated a commendably high level of agreement (> 0.715) between DCNN-generated outputs and definitive diagnoses, highlighting the precision of these models. For example, the Residual Neural Network (ResNet) performed exceptionally well among various CNN frameworks in a study conducted by Zhao et al. This model achieved an F1-score of 0.981 and an AUC of 0.993 for diagnosing Graves’ disease based on SPECT images following 5-fold cross-validation (29).
DCNN-based models have also outperformed junior nuclear medicine residents, although findings have shown variability when compared to senior residents (28, 29). Integrating DL-assisted diagnostic systems holds promise for aiding less experienced physicians, who may sometimes overlook subtle features during scintigraphy assessments (28). Despite this potential, practical implementation of DL assistance in clinical settings may face challenges due to the "black box" problem, a lack of external multicentric validation, and limited training datasets, particularly since scintigraphy is an infrequent clinical procedure.
To address these issues, Zhao et al. utilized gradient-weighted class activation mapping (Grad-CAM) to generate attentional heat maps, highlighting regions of the original input image that the model focused on. This approach improved the interpretability of their proposed framework (29). Future research should prioritize incorporating such interpretative methodologies, like Grad-CAM, to enhance the transparency and understanding of DL networks, thereby increasing their trustworthiness and clinical applicability.
3.3. Thyroid Ultrasound Computer-Aided Diagnosis Systems
Thyroid ultrasound computer-aided diagnosis (CAD) systems have emerged as powerful tools for the accurate and efficient diagnosis of thyroid diseases, particularly thyroid nodules. Computer-aided diagnosis systems can also assist in detecting diffuse inflammatory changes in the gland. For instance, ThyroScan, an ML-based CAD system, extracts significant grayscale features from thyroid ultrasound images to detect Hashimoto’s thyroiditis with relatively high accuracy (84.6%) (31). By incorporating ultrasound videos rather than static images and generating synthetic, high-dimensional, detailed instances alongside clinical and serological data, DL-based models have demonstrated promising performance in diagnosing thyroid dysfunctions (32, 33).
Deep convolutional neural networks (DCNNs) have shown superior performance by leveraging transfer learning, which involves reusing a model trained for one task in another context. It is important to note that the framework of CNN layers significantly influences model performance. For example, adding a dropout layer effectively reduces the overfitting problem, improving model reliability (34). Detailed data from studies utilizing AI to identify thyroid dysfunctions via ultrasonography are presented in Table 2.
3.4. Pregnancy and Major Depressive Disorders
To this point, this review has focused on AI applications for diagnosing thyroid function disorders in the general population, without accounting for concurrent conditions or illnesses. Since the symptoms of thyroid dysfunction often develop gradually, individuals may remain asymptomatic for an extended period. Early diagnosis and intervention are therefore critical to preventing adverse outcomes, particularly in scenarios such as pregnancy and congenital hypothyroidism, where thyroid hormone levels are essential for fetal and neonatal brain development and pregnancy outcomes (35).
Moreover, untreated thyroid dysfunction can exacerbate coexisting conditions, such as cardiovascular, neurological, or psychological disorders (36, 37). For example, major depressive disorder (MDD) represents a significant public health concern due to its impact on quality of life and its association with a higher risk of suicide. Thyroid function status has shown a strong correlation with the development of MDD and response to treatment. Developing ML-based models to predict the risk of suicidal attempts and MDD improvement based on thyroid function data could provide valuable insights into this issue (38-40).
Consequently, the application of AI to address thyroid dysfunctions within specific subgroups has garnered increasing attention in the current literature. Detailed findings are summarized in Table 3.
| First Author, Year, Reference | Aim | Technique | Dataset | Sample Size | Performance Metrics |
|---|---|---|---|---|---|
| Stroek et al., 2023 (41) | Congenital hypothyroidism screening | RF | Features from the Deutch National database | 458 CH-T, 82 CH-C, 2332 false-positive referrals, and 1670 Nl | ACC 0.77 |
| Sun et al., 2021 (42) | Prediction of pregnancy outcome | LR, RF, XGB, and DL | Obstetrics and pre- and post-conception serum TSH features | 3428 delivery from 1 center | XGB: PRETERM BIRTH: AUC 0.812 LOW APGAR SCORE: AUC 0.987, RF: INDUCTION: AUC 0.650 |
| Araya et al., 2021 (43) | Prediction of GDM | PCA | 29 thyroidal and non-thyroidal features in 1 - 2 trimesters | 39 pregnancies from 1 center | NA |
| Mennickent et al., 2023 (44) | Same | LR, L-SVM, PLS-DA, CART, and XGB | 75 thyroidal and non-thyroidal features in 1-2 trimesters | 12 GDM and 54 NGT from 3 centers | PLS-DA: AUC 0.940 |
| Zhou et al., 2022 (45) | Prediction of preterm delivery | GAM | Features from routine prenatal examination | 3176 preterm birth, 2127 Spontaneous preterm birth, and 1049 Iatrogenic preterm birth from 1 center | NA |
| Zhang et al., 2021 (46) | Prediction of postpartum depression | RF, DT, XGB, LR, and MLP | EMRs (32 features) | 14187 non-PPD and 1010 PPD from 1 center for training, 50459 non-PPD and 3513 PPD from another center for validation | LR: AUC 0.937 training and 0.886 validation |
| Yuan et al., 2023 (47) | Prediction of abortion | LR and XGB | 48 features | 340 abortions and 677 IVF-treated delivery from 1 center | XGB: AUC 0.759 and F1-score 0.566 |
| Yang et al., 2023 (40) | Prediction of suicide attempt | LASSO | Hamilton depression and anxiety symptoms and biological features | 1372 non-attempts and 208 attempts from 1 center | AUC 0.72 |
| Li et al., 2021 (38) | Same | GBDT | Hamilton depression and anxiety symptoms and biological features | 1372 non-attempts, 235 recent attempts, and 111 late attempts from 1 center | RECENT: ACC 87% LATE : ACC 88% |
| Qiao et al., 2022 (39) | Prediction of MDD prognosis | SVM | Hamilton depression and anxiety symptoms and TFT features | 2086 MDD from 1 center | ROC-AUC 0.86 |
Abbreviations: GDM, gestational diabetes mellitus; NGT, normal glucose tolerance; LR, logistic regression; XGB, X gradient boosting; SVM, support vector machine; RF, Random forest; PCA, principal component analysis; L-SVM, linear support vector machine; MLP, multilayer perception; LASSO, least absolute shrinkage and selection operator; CART, classification and regression tree; GAM, generalized additive model; DT, decision tree; GBDT, gradient-boosting decision tree; DL, deep learning; PLS-DA, partial least-squares discriminant analysis; EMR, electronic medical record; NL, normal; AUC, area under curve; ACC, accuracy; MDD, major depressive disorder.
3.5. Bioinformatics, Exposure, Radioiodine Therapy, and Levothyroxine Dose Adjustment
Numerous factors contribute to the development of thyroid dysfunction conditions, including thyroid gland inflammation, autoimmune processes (e.g., Graves’ disease and Hashimoto’s thyroiditis), iodine intake, medications, thyroid surgery, radiation therapy, congenital developmental abnormalities (e.g., thyroid agenesis or dysplasia), pituitary disorders, and pituitary or thyroid tumors (6, 7).
Autoimmune thyroid disorders result from a complex interplay between genetic predisposition, dietary influences, coexisting disorders, and environmental triggers (48, 49). By leveraging ML techniques in bioinformatics—an interdisciplinary field combining computer science, mathematics, and statistics for biological data analysis—new insights can be gleaned from large-scale biological datasets such as genomic sequences, protein structures, gene expression profiles, and regulatory mechanisms. Several studies have explored the discovery of diagnostic genes associated with thyroid and related autoimmune disorders (50, 51) (Table 4). For example, Shen et al. identified 75 genes linked to hyperthyroidism using a random walk ML model for gene analysis, achieving an AUC of 0.90. This model also encoded gene interaction networks based on existing gene regulation data to clarify the pathological mechanisms of gene interactions (52).
In recent years, exposure to endocrine-disrupting chemicals (EDCs) has become an increasing public health concern. These chemicals, found in various environmental sources such as air, water, and food, disrupt the normal functioning of the endocrine system by mimicking or blocking the action of natural hormones in the body (53). Some studies have explored the development of predictive ML models to screen TSH receptor agonists and predict their inhibitory or non-inhibitory activity and mechanisms (54, 55) (Table 4).
Radioiodine therapy (RAI) is a widely used treatment for hyperthyroidism, particularly in Graves’ disease, as well as for removing residual thyroid tissue following thyroid cancer surgery (56). Hypothyroidism is a common early consequence of RAI, requiring lifelong thyroid hormone replacement therapy. To address this, researchers have developed ML models to identify risk factors associated with early hypothyroidism after RAI and to screen patients at higher risk. Findings suggest that male gender, older age, lower radioactive iodine uptake, smaller thyroid volume, and certain blood biochemical markers may contribute to an increased risk of hypothyroidism (57, 58). Additionally, ML models have been designed to predict the therapeutic dose of RAI. For instance, random forest (RF) models created for this purpose have demonstrated strong performance (58).
Moreover, patients who have undergone thyroidectomy require exogenous hormone replacement with levothyroxine (LT4). Adjusting the LT4 dose for these patients necessitates careful consideration of individual variability in thyroid hormone requirements, as well as factors influencing the absorption and metabolism of LT4, to achieve euthyroidism. Regression and classification models, such as fuzzy logistic systems and decision trees, have shown promise in providing personalized approaches to LT4 dose adjustment (59-61). Future research should aim to develop models with even higher performance for this purpose. Table 4 also summarizes investigations conducted on the performance of AI systems in predicting post-RAI treatment hypothyroidism and LT4 dose adjustments.
| First Author, Year, Reference | Aim | Technique | Dataset | Sample Size | Performance Metrics |
|---|---|---|---|---|---|
| Atas, 2023 (50) | Prediction of autoimmune concomitant dx with HT | SVM, RF, LR, KNN, MLP, and a ML hybrid model | OMIM, PUBMED, Entrez Gene on NCBI, NCBI dbSNP, and SWISS Prot database | 162 genes | ACC 0.815, precision 0.731, recall 1.0, and F1-score 0.800 |
| Li et al., 2024 (51) | HT diagnosis based on genes | LASSO | HRA001684, GSE29315 and GSE163203 datasets | 2000 highly variant genes | NA |
| Shen et al., 2021 (52) | Prediction of genes of hyperthyroidism | RW-RVM, RF, ANN, and NB | DisGeNET | 269 genes | AUC 0.90 |
| Liu et al., 2023 (54) | Screening Tshr agonists | RF, MLP, SVM, and GAT | Updated TSHR agonist dataset from PubChem fingerprints | 7 molecular representations | RF: AUC 0.984, and ACC 0.941 |
| Xu et al., 2022 (55) | Detection of TSHR inhibitory chemicals | RF, XGB, and LR | Tox21 database | 5952 compounds from a cAMP analysis | RF: ACC 0.85, recall 0.89, and AUC 0.92 |
| Gao et al., 2021 (58) | Prediction of 131i therapeutic dose | BPNN, RBFNN, SVM, BP-AdaBoost, and RF | EMRs (17 features) | 353 patients from several centers | RF: ACC 100% |
| Duan et al., 2022 (57) | Prediction of hypothyroidism after RAIT | ML | EMR (138 clinical and lab test features) | 471 GD patients from 1 center | AUC 0.74 and F1-score 0.74 |
| Chen et al., 2019 (59) | Levothyroxine dosage post-thyroidectomy | DT | LT4 doses and TSH levels | 320 patients from 1 center | Correctly predicted dose adjustment 75%, confidence interval = 65% - 82% |
| Barrio et al., 2023 (60) | Same | ANN, RF, 0LS, and LR | Demographic, clinical, and laboratory data | 951 patients from 1 center | Met postopTSH goal 45.3% |
| Hemmati et al., 2023 (61) | Same | Fuzzy logic | NA | Thyrosim application to simulate thyroid hormone courses of a virtual thyroidectomized patient | NA |
Abbreviations: HT, Hashimoto’s thyroiditis; GD, Graves’ disease; TSHR, thyroid stimulating hormone receptor; RAIT, radioactive iodine therapy; LT4, levothyroxine; LR, logistic regression; XGB, extreme gradient boosting; SVM, support vector machine; ANN, artificial neural network; KNN, K-nearest neighbors; RF, random forest; OLS, ordinary least squares; BP-AdaBoost, back propagation-adaptive boosting; RBFNN, radial basis functions neural Network; MLP, multilayer perceptron; LASSO, least absolute shrinkage and selection Operator; RW-RVM, random walk-relevance vector machine; GAT, graph attention network; BPNN, back propagation neural network; EMR, electronic medical record; NL, normal; AUC, area under curve; ACC, accuracy.
3.6. Thyroid-Associated Ophthalmopathy
Thyroid-associated ophthalmopathy (TAO), also known as Graves’ ophthalmopathy, is a potentially sight-threatening ocular condition characterized by upper lid retraction, lid lag, and eye protrusion. Numerous studies have evaluated the performance of AI in extracting eye parametric data from orbital imaging modalities, particularly computed tomography (CT) scans and magnetic resonance imaging (MRI), to detect this disorder and assess its severity (62-64) (Table 5). These investigations have primarily employed deep convolutional neural networks (DCNNs) with various architectures, such as Visual Geometry Group Network (VGG), Residual Neural Network (ResNet), and GoogleNet Inception (GoogLeNet). The performance of these models has been comparable to that of experienced ophthalmologists. For instance, Karlin et al. introduced an ensemble DL model that demonstrated greater accuracy than ophthalmologists in diagnosing TAO from external orbital images (65).
| First author, Reference, Number | Aim | Technique | Dataset | Sample Size | Performance Metrics |
|---|---|---|---|---|---|
| Lee et al., 2022 (62) | TAO diagnosis | DL | Orbital CT scans | 99 mild GO, 94 mod-to-severe, and 95 Nl from 1 center | AUC 0.895 - 0.979 |
| Lin et al., 2024 (63) | Same | DL | Orbital CT scans | 459 mild, 355 severe, and 373 Nl from 1 center | ACC 89.5% and AUC 0.96 - 0.99 |
| Lin et al., 2021 (64) | Same | DL | Orbital MRI | 50 active phase and 110 inactive phase from 1 center | ACC 0.863, precision 0.680, and F1-score 0.712 |
| Karlin et al., 2023 (65) | Same | DL | External orbital photographs | 2288 images from 1 clinical dataset | ACC 89.2%, recall 93.4%, precision 79.7%, and F1 score 86.0% |
| Yoo et al., 2020 (66) | Prediction of post-orbital decompression surgery appearance | Generative adversarial network (GAN) | Facial photographs | 109 pairs of matched pre- and postoperative facial images from amGoogle image search | ACC 90.9% and AUC 0.957 |
| Zhai et al., 2021 (67) | Prediction of the therapeutic efficacy of IV glucocorticoids | Binary LR | Orbital MRI and clinical characteristics | 35 responsive and 28 unresponsive orbit | AUC 0.844 |
Abbreviations: TAO: thyroid associated ophthalmopathy; LR: logistic regression; DL: deep learning; CT: computed tomograohy scan; MRI: magnetic resonance imaging; NL: normal; AUC: area under curve; ACC: accuracy.
Researchers have also developed predictive models for treatment response and post-decompression surgery outcomes in TAO patients (66, 67). For example, using dual facial photographs from 109 patients who had undergone orbital decompression surgery, a generative adversarial network (GAN) achieved an accuracy of 90.9% and an AUC of 0.957. This model demonstrated one of the highest performances among predictive models for surgical outcomes in TAO patients (66). In another study, Zhai et al. highlighted the potential utility of T2 mapping and T2 Iterative Decomposition of Water and Fat with Echo Asymmetry and Least-Squares Estimation (IDEAL) as predictors for response to glucocorticoid therapy in patients with active and moderate-to-severe TAO (67).
The limitations of the mentioned models primarily arise from the fact that they are mostly trained on abnormal medical imaging, as healthy individuals typically do not undergo orbital imaging. This reliance on abnormal cases can lead to sample bias, as the absence of normal control data may skew the results, thereby limiting the generalizability of the models. To overcome these challenges, future research should focus on training models using larger and more diverse datasets that include normal controls, as well as other differential diagnoses for TAO. These models should integrate both clinical and imaging data to identify correlations between imaging results and clinical presentations. Such an approach could expedite the diagnostic process and help prevent potential permanent eye damage or vision loss through earlier intervention.
4. Discussion and Conclusions
Applying AI to the diagnosis and treatment of thyroid disorders holds immense potential to revolutionize patient care. The AI-powered models can interpret TFT results and provide comprehensive diagnostic assessments based on clinical and laboratory data. Most studies have utilized the University of California, Irvine (UCI) ML repository to train their interpretive models. The UCI repository is a publicly available, prominent resource for researchers and practitioners, offering a diverse collection of datasets that span various domains, including thyroid disease datasets that incorporate various TFT components and clinical variables.
Research has also explored AI applications for detecting thyroid dysfunction, ranging from routine clinical laboratory data to other supplementary diagnostic methods. The training datasets in these studies mainly consist of laboratory results, alongside demographic and clinical variables acquired from electronic medical records of single or multiple centers. Feature selection engineering allows for identifying the most valuable variables for training improved models.
Deep learning-based models primarily hold the potential to enhance the diagnostic accuracy of medical imaging for thyroid dysfunctions, particularly by analyzing thyroid scintigraphies and ultrasound images. DL image processing has also performed excellently in diagnosing and evaluating the severity of TAO from orbital CT scans. However, since imaging modalities for assessing thyroid function disorders are relatively uncommon, the lack of large, diverse, and balanced datasets remains a significant challenge in training such models. Researchers should collaborate across institutions to pool datasets and ensure better generalization.
Artificial intelligence can also aid in predicting pregnancy complications, improving newborn screening programs, forecasting treatment responses, assessing the likelihood of suicidal attempts in patients with MDD, and optimizing levothyroxine dose adjustment. To train AI models for these purposes, it is essential to include not only features of concurrent conditions, but also TFT results, routine laboratory data, and demographic, biological, psychosocial, and clinical variables to create trustworthy models.
While AI technology holds significant potential to improve the management of thyroid disorders, challenges such as data quality, model interpretability, and the need for extensive validation have made it a long way from replacing specialists. By addressing these challenges, future research can develop models that provide a high level of reliability and advance the field of endocrinology.