1. Background
The pulse oximeter is a standard monitoring device used by all patients in the operating room. However, changes in the position or movement of the patient can cause various errors in pulse oximetry, including decreased accuracy, signal loss, false alarms for desaturation levels, and delayed detection of hypoxia. Measuring devices made of commonly used plastic or rubber may have problems such as slipping off the finger or being pressed by the patient or surgical team, making it difficult to perform effective monitoring. Thus, motion artifacts create false positives and false negatives (1). Manufacturers are developing various products to address these problems, and devices that can simultaneously monitor various functions are being introduced. Recent reports have suggested that pulse oximeter performance during poor perfusion can vary among present-day device brands (2).
New versions of monitoring devices are being developed to improve oxygen saturation (SpO2) accuracy and monitor various parameters simultaneously. The analysis value is known to be useful for observing perfusion trends because it is calculated based on peripheral blood flow, and it is considered non-invasive for patients who need continuous management, such as those in the intensive care unit (3, 4).
The monitoring device used in this study was a tape-type device that wrapped around the entire fingertip and could monitor perfusion indices simultaneously, making it possible to identify and respond appropriately to postural changes. Additionally, this device can monitor not only the SpO2 but also the Perfusion Index (Pi).
2. Objectives
We aimed to analyze the peripheral Pi patterns according to postural changes during gynecological surgery. Additionally, we determined whether changes in lung mechanics affect oxygen content (SpOC) and SpO2.
3. Methods
3.1. Ethical Considerations
The study was performed in accordance with the principles of the 1975 Declaration of Helsinki (revised in 2018) and was approved by the Institutional Review Board of our hospital (IRB no. 2024-03-009-001), and registered in the Korean Clinical Trial Registry (KCT0010647).
3.2. Patient Population
Sixty-six patients participated in this study, and each provided informed consent. They were aged > 18 years and underwent gynecological surgery under general anesthesia between 2024 and 2025. Patients with respiratory diseases that affect respiratory mechanics, such as acute respiratory distress syndrome or chronic obstructive pulmonary disease; those with cognitive dysfunction that made it difficult to understand the study; those for whom it was difficult to obtain stable values for each index because the total duration of surgery was less than 30 min; and those with cancer undergoing complex surgery were excluded from this study.
Inclusion criteria: (1) > 18 years; (2) undergoing gynecological surgery with general anesthesia; (3) expected surgical duration ≥ 30 min; and (4) being able to provide informed consent.
3.3. Anesthetic Management
Noninvasive blood pressure, electrocardiography, pulse oximetry, and Masimo SET (RD rainbow SETTM-2 Neo) were used for patient monitoring. The SpO2 and Masimo were placed on the second and third fingers of the ipsilateral hand, respectively, where blood pressure was not measured. Hemodynamic parameters were recorded every 3 min until the end of surgery to monitor changes in vital signs. General anesthesia was induced with propofol 1.5 - 2.0 mg/kg, rocuronium 0.8 - 1.0 mg/kg, lidocaine 50 mg, and fentanyl 20 mcg intravenously. Initially, 100% oxygen and sevoflurane were administered by manual bagging. The ventilator was set to a pressure control-volume guaranteed mode with a tidal volume of 8 mL/kg, respiratory rate of 14 breaths/min, and positive end-expiratory pressure ventilation of 4 mmHg after intubation. Anesthesia was maintained by gas inhalation of desflurane 5 - 8 vol% at a minimum alveolar concentration (MAC) ≥ 1.0, and the fresh gas range was set to 40% inspired oxygen fraction using air. Additional fentanyl was administered as needed to maintain systolic blood pressure (SBP) within 20% of the baseline. If the duration of surgery lasted more than 1 h, an additional 10 mg of rocuronium was administered.
3.4. Data Parameters
The Masimo SET (RD rainbow SETTM-2 Neo, MDSS GMbH, Schiffgraben, Germany) used in this study is a device that can monitor total hemoglobin (SpHb®), carboxyhemoglobin (SpCO®), methemoglobin (SpMet®), and oxygen content (SpOCTM) in addition to SpO2, pulse rate (PR), Pi, and Pleth Variability Index (PVi®).
The SpOC is the amount of oxygen in the blood of a patient that is calculated by combining hemoglobin and SpO2, and it can help clinicians assess the oxygenation status. The Pi has been considered useful for accurately monitoring changes in peripheral perfusion caused by certain anesthetics in real time. The PVi is a dynamic index for monitoring fluid responsiveness using a single-pulse oximetry sensor. It can provide a continuous and noninvasive measure of the relative variability in photoplethysmography (pleth) during the respiratory cycle. The PVi is a dynamic index ranging from 0 to 100 that measures the relative variability of the pleth waveform noninvasively using a single-pulse oximetry sensor. Increased variability in the pleth waveform is associated with preload dependence and fluid responsiveness, making it a valuable parameter for monitoring acute care.
The pressure change according to posture was observed under the same ventilator setting mentioned under the anesthetic management. For the hemodynamic parameters, heart rate (HR), SBP, diastolic blood pressure (DBP), and SpO2 values are described in the study protocol.
3.5. Data Extraction
Anesthesia is usually administered in the supine position during gynecological surgery, and the patient is prepared for surgery in the lithotomy position. The patient assumes the Trendelenburg position during and is placed supine after surgery. These postural changes are concurrent with cardiovascular volume changes, and it is difficult to determine whether perfusion to peripheral tissues occurs efficiently. Therefore, parameters at four different time points according to postural changes were extracted and described in the study protocol.
- Initial position: Supine position immediately after induction of anesthesia, before lithotomy positioning.
- Supine (final) position: Supine after completion of surgery, following Trendelenburg and lithotomy.
3.6. Outcome Measures
The primary outcome was to observe and analyze changes in the Pi according to the four stages of postural change. Changes in hemodynamic variables may accompany this, and an additional analysis was conducted to determine whether there was a correlation. As a secondary outcome, we compared and analyzed the effects of respiratory dynamics on SpOC according to the four stages of postural changes.
3.7. Statistical Analysis
Statistical analysis was performed using SPSS statistical software (IBM SPSS Statistics 21; IBM Corp., USA). A t-test was performed for continuous variables, and a chi-square test was performed for categorical variables. Pearson’s correlation coefficient and paired t-tests were used to assess the correlations and compare the variables and initial values, respectively. Statistical significance was set at P < 0.05. The sample size was calculated using MedCalc software version 14 (MedCalc Software BVda, Ostend, Belgium) to detect an area under the curve of 0.8 using the null hypothesis that the AUROC curve was 0.5. A minimum of 60 patients were required based on a study power of 80% and a margin of error of 0.05. To compensate for missing data and other problems, an additional 10% of patients were recruited, and the study was conducted with a final sample size of 66 patients.
4. Results
Sixty-three patients were enrolled, excluding two patients who underwent surgery within 30 min and one who underwent complicated cancer surgery between 2024 and 2025 (Figure 1). All patients were classified as grades I - III based on their American Society of Anesthesiologists (ASA) physical status. The most common surgical procedure was ovarian cystectomy (29 patients, 46%), followed by total hysterectomy (23 patients, 36.5%), and myomectomy (10 patients, 15.9%; Table 1).
| Variables | Patients |
|---|---|
| Age (y) | 44.5 ± 10.9 |
| Height (cm) | 159.8 ± 6.7 |
| Weight (kg) | 62.2 ± 11.4 |
| BSA (m2) | 1.7 ± 0.2 |
| BMI (kg/m2) | 24.3 ± 4.1 |
| Past medical history | |
| Hypertension | 8 (12.7) |
| Diabetes mellitus | 5 (7.9) |
| Hyperlipidemia | 8 (12.7) |
| Thyroid disease | 4 (6.3) |
| Respiratory disease | 4 (6.3) |
| Gynecological surgery | |
| Total hysterectomy | 23 (36.5) |
| Ovarian cystectomy | 29 (46.0) |
| Myomectomy | 10 (15.9) |
| Endometriosis | 1 (1.6) |
| Operation time (min) | 80.0 [55.0 - 102.0] |
| Anesthetic time (min) | 107.0 [82.5 - 130.0] |
| Administration of fluid (mL) | 220.0 ± 112.0 |
| Estimated blood loss (mL) | 64.4 ± 82.7 |
Abbreviations: BSA, body surface area; BMI, Body Mass Index.
a Data are presented as mean ± SD, No. (%), or median [interquartile range].
Descriptive statistics of the major variables according to the changes in position during surgery showed notable changes in the Trendelenburg position, where most of the fluid changes occurred (Table 2). The SpOC values showed no significant changes. However, PVi and Pi were significantly different, whereas PVi did not differ significantly from the initial value in the Trendelenburg position (P = 0.202). The Pi showed significant differences for all posture changes (P < 0.001; Table 3).
| Variables | Mean ± SD | Median | IQR 25% | IQR 75% | SE |
|---|---|---|---|---|---|
| SBP (mmHg) | |||||
| Initial | 12.49 ± 1.16 | 12.5 | 10.5 | 16.3 | 0.15 |
| Lithotomy | 12.25 ± 1.35 | 12.5 | 9.5 | 15.4 | 0.17 |
| Trendelenburg | 12.89 ± 1.3 | 12.9 | 9.7 | 15.7 | 0.16 |
| Supine | 12.61 ± 1.37 | 12.8 | 9.5 | 15.6 | 0.17 |
| Ppeak (cmH2O) | |||||
| Initial | 14.75 ± 1.47 | 15 | 12 | 18 | 0.19 |
| Lithotomy | 14.1 ± 1.51 | 14 | 11 | 19 | 0.19 |
| Trendelenburg | 21.08 ± 3.01 | 20 | 16 | 28 | 0.38 |
| Supine | 15.41 ± 1.55 | 15 | 12 | 19 | 0.2 |
| SpHb (g/dL) | |||||
| Initial | 12.49 ± 1.16 | 12.5 | 11.65 | 13.2 | 0.15 |
| Lithotomy | 12.25 ± 1.35 | 12.5 | 11.2 | 13.1 | 0.17 |
| Trendelenburg | 12.89 ± 1.3 | 12.9 | 11.95 | 13.7 | 0.16 |
| Supine | 12.61 ± 1.37 | 12.8 | 11.5 | 13.55 | 0.17 |
| PVi (%) | |||||
| Initial | 17.9 ± 6.15 | 17 | 13 | 22 | 0.78 |
| Lithotomy | 12.7 ± 4.72 | 13 | 10 | 15 | 0.59 |
| Trendelenburg | 9.13 ± 4.74 | 8 | 6 | 11 | 0.6 |
| Supine | 15.83 ± 6.58 | 15 | 11.05 | 21 | 0.83 |
| Pi (%) | |||||
| Initial | 2.57 ± 1.79 | 2.1 | 1.3 | 3.35 | 0.23 |
| Lithotomy | 5.54 ± 1.97 | 5.2 | 4.1 | 6.9 | 0.25 |
| Trendelenburg | 5.82 ± 2.55 | 5.5 | 4 | 7 | 0.32 |
| Supine | 3.75 ± 2.37 | 3.3 | 1.75 | 5.4 | 0.3 |
| SpOC (mL O2/dL) | |||||
| Initial | 16.38 ± 1.41 | 17 | 15 | 17 | 0.18 |
| Lithotomy | 16.3 ± 1.72 | 17 | 15 | 17 | 0.22 |
| Trendelenburg | 16.73 ± 1.64 | 17 | 16 | 18 | 0.21 |
| Supine | 16.76 ± 1.64 | 17 | 16 | 18 | 0.21 |
Abbreviations: IQR, interquartile range; Ppeak, peak airway pressure; Pi, Perfusion Index; PVi, Pleth Variability Index; SpHb, total hemoglobin; SpOC, oxygen content; SD, standard deviation; SE, standard error; SBP, systolic blood pressure.
| Variables | Difference (%) | P-Value |
|---|---|---|
| PVi (%) | ||
| Lithotomy | 57.5 | 0.000 |
| Trendelenburg | 15.5 | 0.2022 |
| Supine | 97.0 | 0.000 |
| Pi (%) | ||
| Lithotomy | -101.5 | 0.000 |
| Trendelenburg | -47.0 | 0.000 |
| Supine | -111.5 | 0.000 |
| SpOC (mL O2/dL) | ||
| Lithotomy | 17 | 0.1517 |
| Trendelenburg | -26 | 0.289 |
| Supine | -25 | 0.356 |
Abbreviations: Pi, Perfusion Index; PVi, Pleth Variability Index; SpOC, oxygen content.
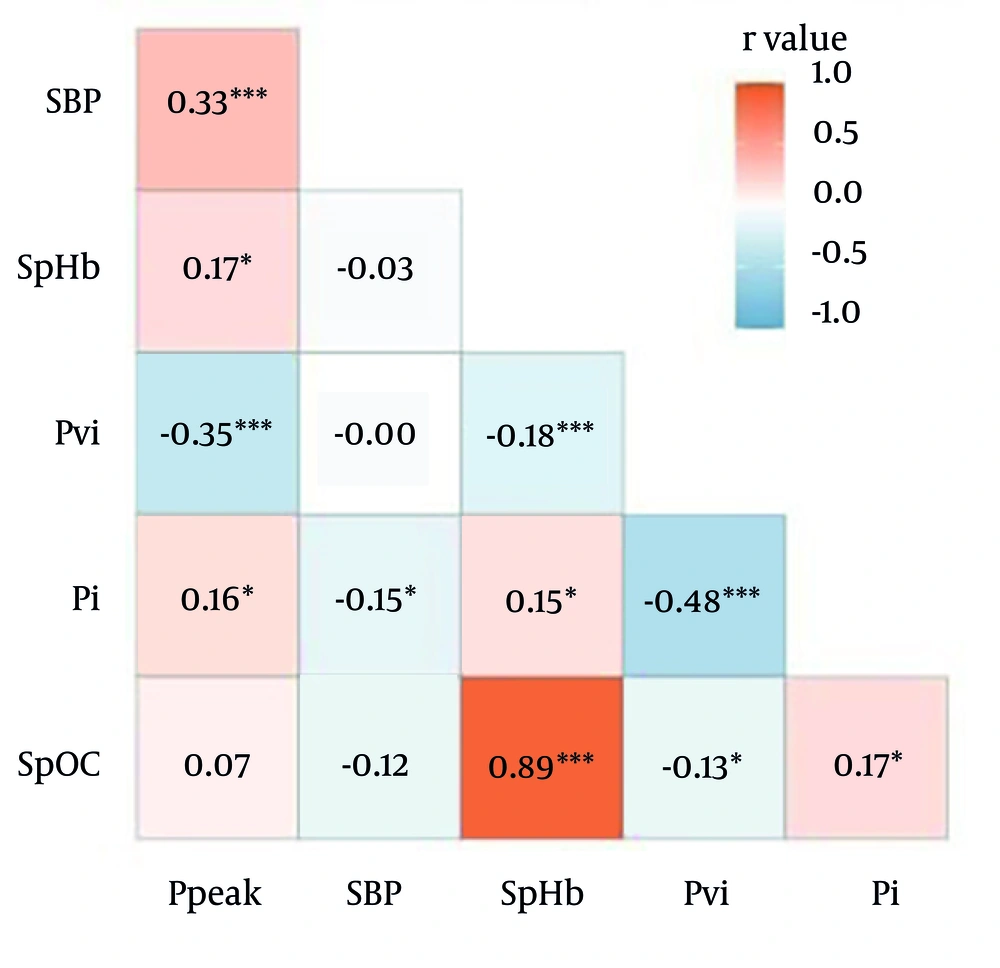
Pearson analysis performed to confirm the correlation between indicators showed that the correlation coefficient for Pi was less than 0.5, but it denoted a significant correlation for all indicators. The PVi showed a significant correlation with all other indicators except for SBP (Figure 2).
Associations of correlation coefficients by Pearson’s product-moment (abbreviations: Ppeak, peak airway pressure; MPi, Masimo Perfusion Index; MPVi, Masimo Pleth Variability Index; MSpHb, Masimo total hemoglobin; MSpOC, Masimo oxygen content; r, correlation coefficient; SBP, systolic blood pressure; * P < 0.01 and *** P < 0.0001).
5. Discussion
Anesthesia is usually induced in the supine position, and the patient is prepared for surgery in the lithotomy position. The patient assumed the Trendelenburg position during and placed in the supine position after the surgery. While such postural changes occur, cardiovascular volume changes also occur, and it is difficult to determine whether perfusion occurs efficiently in peripheral tissues. Among the various positions, the Trendelenburg position significantly increases stroke volume and improves multiple hemodynamic parameters in adult patients (5). Ultimately, these changes lead to improved perfusion. In this study, we aimed to confirm whether these changes were reflected in Pi using a noninvasive device.
In actual monitoring devices, PVi is automatically calculated based on the Pi value using the following formula (Equation 1):
The Pi is the measured ratio of pulsatile to non-pulsatile signals in the plethysmography waveform of an infrared light-emitting diode (LED).
However, the distribution of the PVi and Pi values shows an inverse relationship for each posture because the increase and decrease in the peripheral pulse waveform width affects the calculated value. Masimo devices support Pi ranging from 0.02 to 20% as a non-invasive measure of the pulse strength of the arteriolar blood volume interrogated by the pulse oximeter sensor. The Pi reflects the change in blood volume with each heartbeat in the fingers (6). The Pi is clearly related to peripheral tissue perfusion (7) but also depends on other variables that affect the local arteriolar volume, including vessel compliance (8). A Pi value of ≤ 1 is considered to denote low perfusion while that of > 1 is considered to denote normal perfusion. These values are comparable to the Pi thresholds for normal and low perfusion determined in previous studies (7-9). Most anesthetics induce vasodilation by increasing the vasoconstriction threshold. Anesthesia can also cause temperature redistribution, which further affects peripheral perfusion (10). The future value of considering perioperative changes in Pi during surgical procedures for monitoring temperature redistribution, vasodilatation, and efficacy of anesthesia has been suggested. Therefore, when our results showed the trend of the Pi while applying these conditions as equally as possible, we were.
The Pi can be used in various applications. In addition to studies based on the fluid volume of patients in critical care or surgery, studies using the Pi to assess the success or failure of patients who have undergone regional anesthesia have also been reported (11-13). Therefore, the Pi was found to be more sensitive to the condition of the patient than the other indices when the environmental conditions were applied equally and its trend was confirmed (Table 3 and Figure 2).
Although the trendelenburg position is expected to enhance venous return and potentially increase cardiac filling pressures, our findings did not show a significant change in PVi. This may be attributed to the compensatory mechanisms maintaining hemodynamic stability under anesthesia or to the limitations of PVi as a surrogate for dynamic changes in preload under these specific conditions. Trendelenburg position enhances venous return and stroke volume; however, PVi is a dynamic index reflecting respiratory-induced variation in pleth waveform amplitude, not absolute preload. Under controlled ventilation with constant tidal volume, respiratory-driven variability may not increase even if preload increases. Additionally, anesthesia-induced vasodilation and reduced sympathetic tone may blunt cyclic variation in peripheral vasculature. Therefore, even though preload increased, the PVi did not show significant change.
Also, SpOC did not show a significant difference when observed with this noninvasive device, even though lung mechanics changed with postural changes (14). Ppeak significantly increased in the Trendelenburg position when the same tidal volume was set due to an increase in abdominal pressure. This may be attributed to the maintenance of SpOC in a range that does not significantly affect hemoglobin concentrations or SpO2 when the respiratory mechanics of the patient do not show a significant enough difference to induce critical changes. Despite postural effects on lung mechanics (e.g., increased Ppeak), SpOC remained stable because hemoglobin concentration did not change significantly and SpO2 remained within a narrow range. The SpOC is relatively insensitive to short-term mechanical changes when ventilation remains controlled.
This study had some limitations. This study was limited to gynecological surgeries. This may be controversial; however, various types of routine postural changes are required in gynecological surgery. In addition, the study was limited to one patient group because only a few surgical factors affected the volume status of the patient, such as excessive bleeding. The parameters were measured using a single product, and differences by manufacturer could not be compared; however, it is meaningful for analyzing trends. Findings may not generalize to other manufacturers because only a Masimo device was used. Nevertheless, we found that continuous changes and peripheral perfusion maintenance could be effectively monitored according to the posture of the patient when monitoring patients using Pi. These results are useful for judging false-positive or negative values when recognizing abnormal indicators relative to other monitoring devices, and they can facilitate appropriate anesthetic management to patients. Furthermore, the index may be more useful not only for healthy patients, but also for patients with conditions that can be affected by even small volume changes.