1. Context
Traumatic brain injury (TBI) affects over 50 million people annually worldwide, with secondary ischemic injuries contributing significantly to poor outcomes. Monitoring cerebral oxygenation is crucial for preventing secondary damage. Jugular venous oxygen saturation (SjvO2), introduced in the 1980s, measures oxygen saturation in jugular bulb blood, reflecting global cerebral oxygen extraction (normal range 55 - 75%). In contrast, near-infrared spectroscopy (NIRS) uses near-infrared light (700 - 1000 nm) to non-invasively measure regional oxygen saturation (rSO2) in the frontal cortex microvasculature (normal range 60 - 80%, device-dependent) (1, 2).
While several reviews exist on neuromonitoring, a direct and systematic comparison focusing on the technical and clinical nuances of SjvO2 versus NIRS in TBI is lacking. Many studies compare SjvO2 to the invasive gold standard of brain tissue oxygen (PbtO2), leaving the role of non-invasive NIRS less clearly defined.
2. Objectives
This review aims to fill this gap by systematically synthesizing evidence on SjvO2 and NIRS, clarifying their respective roles, and exploring the potential for a combined monitoring approach to optimize patient care.
3. Methods
3.1. Study Design
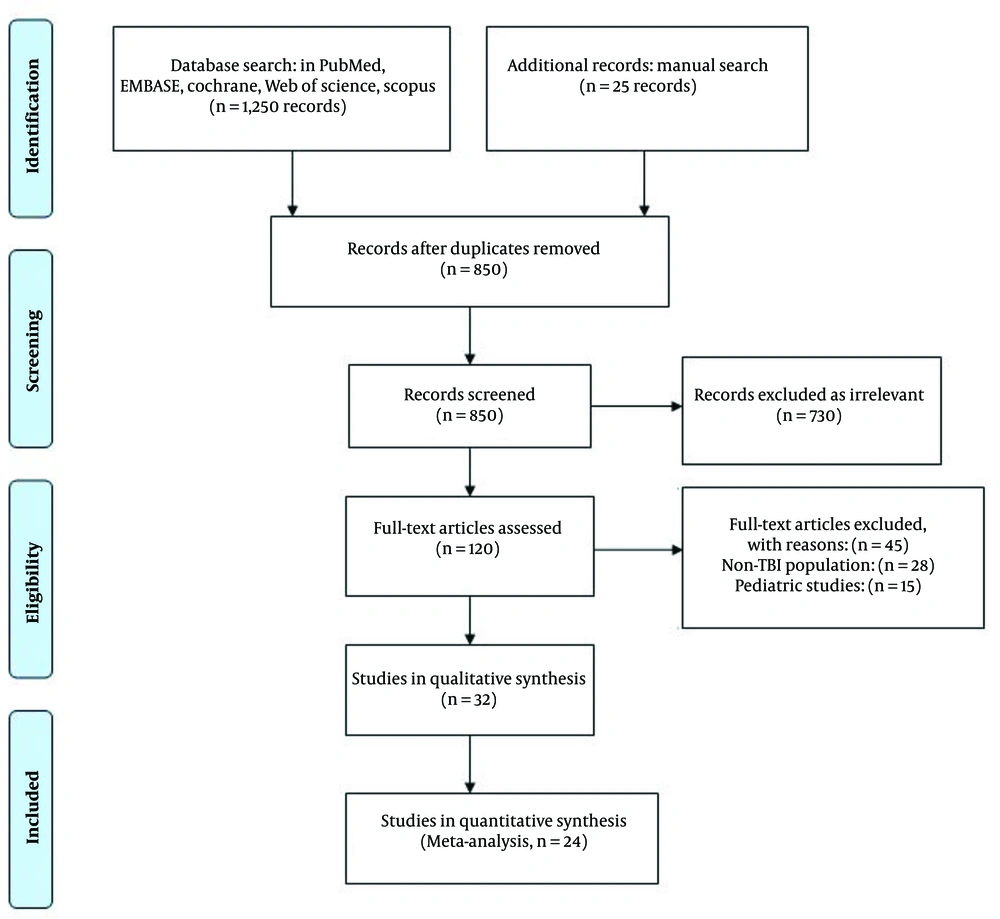
This systematic review was conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.
3.2. Search Strategy
We searched PubMed, EMBASE, Cochrane Library, Web of Science, and Scopus from January 1996 to August 2023. The search strategy used a combination of terms: (Jugular venous oxygen saturation OR SjvO2 OR SjO₂ OR jugular bulb oximetry) AND (near-infrared spectroscopy OR cerebral oximetry OR NIRS OR rSO2) AND (traumatic brain injury OR TBI OR head injury). Filters were applied to include only human studies published in English.
3.3. Study Selection
1. Inclusion criteria:
- Population: Adult (≥ 18 years) patients with TBI.
- Intervention/comparator: Studies directly comparing SjvO2 to NIRS, or studies comparing either SjvO2 or NIRS to PbtO2 were included to provide a comprehensive view of the monitoring landscape and inform the comparison.
- Outcomes: Reported data on correlation between modalities, sensitivity/specificity for detecting ischemia, association with clinical outcomes (e.g., Glasgow Outcome Scale, mortality), and/or complication rates.
2. Exclusion criteria:
- Pediatric studies.
- Non-TBI populations (e.g., stroke, cardiac surgery).
- Case reports, reviews, editorials, and conference abstracts.
3.4. Data Extraction and Quality Assessment
Two independent reviewers extracted data using a standardized form, capturing detailed study characteristics (e.g., design, sample size, patient demographics), monitoring details, thresholds, correlation metrics, outcomes, and complications. Any discrepancies were resolved by consensus or a third reviewer.
Study quality was assessed using the Newcastle-Ottawa Scale for observational studies. Key quality criteria included radiographic confirmation of SjvO2 catheter position, methods for NIRS signal quality control (e.g., excluding extracranial contamination), and blinding of outcome assessors where possible.
3.5. Data Synthesis
Due to significant heterogeneity in monitoring protocols, devices, and reported outcomes, a formal meta-analysis was not feasible. The results are presented as a narrative synthesis with summary statistics (e.g., pooled proportions, mean correlations) derived from the included studies where data were comparable. This approach provides a qualitative and descriptive summary of the evidence.
3.6. Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flow Diagram
The search and selection process are summarized in the PRISMA flow diagram below: Of the 32 studies included for qualitative synthesis, 24 studies provided sufficiently homogeneous data on clinical performance parameters (e.g., sensitivity, specificity) to be included in a quantitative summary (Figure 1).
4. Results
4.1. Physiological and Technical Comparison
1. The SjvO2 monitoring is invasive, requiring jugular bulb catheterization (3). It operates on the Fick principle, providing a global measure of cerebral oxygen extraction (4). Common thresholds are < 50% for ischemia and > 75% for hyperemia (5). A significant limitation is its susceptibility to artifacts from catheter malposition (6) and a relatively low data quality time (reported as 43 - 68%).
2. The NIRS monitoring is non-invasive, using forehead sensors to measure regional microvascular saturation (with approximately 70% venous weighting) (7, 8). Ischemia is typically defined as a > 20% decrease from baseline or an absolute value < 50% (9). Its primary limitations include susceptibility to extracranial contamination (10) and its regional focus, primarily assessing the frontal cortex (Table 1).
| Features | SjvO2 Monitoring | Cerebral Oximetry (NIRS) |
|---|---|---|
| Measurement type | Global venous saturation | Regional microvascular saturation |
| Invasiveness | Invasive (jugular catheter) | Non-invasive |
| Anatomical coverage | Whole-brain drainage | Frontal cortex (1 - 3 cm depth) |
| Normal values | 55 - 75% | 60 - 80% (device-dependent |
| Ischemia threshold | | < 50% | > 20% drop from baseline or < 50% |
| Response time | 30 - 60 s delay | Real-time (5 - 10 s delay) |
| Complication rate | 8 - 12% (infection, thrombosis) | None |
| Data quality time | 43 - 68% | 85 - 95% |
| Cost per use | High (catheter+monitoring) | Moderate (sensors only) |
Abbreviations: SjvO2, jugular venous oxygen saturation; NIRS, near-infrared spectroscopy.
4.2. Clinical Performance in Traumatic Brain Injury
A summary of pooled data from 24 comparable studies is presented in Table 2. The SjvO2 demonstrated higher sensitivity for detecting global ischemic events, while NIRS showed superior ability in identifying focal lesions. The correlation with patient outcomes was modest for both modalities but stronger for SjvO2.
| Parameters | SjvO2 (95% CI) | NIRS (95% CI) | P-Value |
|---|---|---|---|
| Sensitivity for ischemia | 72% (65 - 79) | 58% (49 - 67) | 0.003 |
| Specificity for ischemia | 84% (78 - 89) | 76% (68 - 83) | 0.12 |
| Correlation with outcome (R) | 0.41 (0.33 - 0.49) | 0.29 (0.21 - 0.37) | 0.02 |
| Detection of focal lesions | 12% (8 - 17) | 85% (79 - 90) | < 0.001 |
| Artifact susceptibility | High (catheter-related) | Moderate (movement) | - |
Abbreviations: SjvO2, jugular venous oxygen saturation; NIRS, near-infrared spectroscopy.
In focal injuries, SjvO2 often correlated poorly with regional hypoxia measured by PbtO2 (r2 = 0.07) (11), whereas NIRS was more effective in these scenarios. However, NIRS could miss severe global ischemia, such as in brain death cases where SjvO2 showed clear abnormalities (12). During challenges like hyperventilation, SjvO2 and NIRS correlations were stronger in uninjured brain regions (r2 = 0.69) than in injured areas (Table 2) (13, 14).
4.3. Prognostic Value
4.3.1. Jugular Venous Oxygen Saturation
Values below 55% sustained early after injury were predictive of poor outcome (odds ratio 3.2, 95% confidence interval 1.8 - 5.7) (15). Prolonged desaturation episodes (> 10 min) were associated with significantly increased mortality (up to 80%) (16). Elevated SjvO2 (> 75%), indicating possible hyperemia or loss of metabolic function, was also associated with worse outcomes (14, 17).
4.3.2. Near-Infrared Spectroscopy
A decrease in rSO2 (< 50% for > 15 minutes) was predictive of worse Glasgow Outcome Scale scores (P = 0.02) (18). The NIRS also showed high sensitivity (85%) in detecting evolving hematomas (19).
5. Discussion
This systematic review highlights the complementary roles of SjvO2 and NIRS in the neuromonitoring of TBI patients. The key finding is that the choice of monitor is not mutually exclusive but should be guided by the clinical context and the nature of the brain injury (Table 3).
| Author(s) | Year | Title and Journal | Type of Study | Study Community | Key Findings | Citation |
|---|---|---|---|---|---|---|
| Gopinath et al. | 1994 | Jugular venous desaturation and outcome after head injury (Journal of Neurology) | Prospective cohort study | 116 | Monitoring SvO2 might allow early identification and therefore treatment of many types of secondary injury to the brain. | (15) |
| Gupta et al. | 1999 | Measuring PbtO2 compared with SjvO2 for monitoring cerebral oxygenation after TBI (Anesthesia & Analgesia) | Interventional study | 13 | Measurement of local tissue oxygenation can highlight focal differences in regional cerebral oxygenation that are disguised when measuring SjvO2. | (11) |
| Vigue et al. | 1999 | Early SjvO2 monitoring in patients with severe brain trauma (Intensive Care Medicine) | Prospective, observational study | 27 | Early cerebral monitoring with SjvO2 is critical to assess cerebral ischemic risk and that MAP monitoring alone is not sensitive enough to determine the state of oxygenation of the brain. | (16) |
| Filippi et al. | 2000 | Brain tissue pO2 related to SjvO2, ICP, and CPP in severe brain injury (Neurosurgical Review) | Prospective, observational study | 27 | PtiO2 monitoring will be a very important and reliable tool in the treatment of brain injury in the future, especially in its correlation to ICP and CPP. | (20) |
| Ma et al. | 2022 | Comparing NIRS — measured cerebral oxygen saturation and corresponding venous oxygen saturations in children with congenital heart disease: A systematic review and meta-analysis (Translational Pediatrics) | A systematic review and meta-analysis | There was no significant difference in Cohen’s d between rScO2 and ScvO2 or between rScO2 and SjvO2 and notable heterogeneity existed. | (17) | |
| Chauhan et al. | 2020 | Comparison of propofol and sevoflurane on cerebral oxygenation using SjvO2 in patients undergoing surgery for TBI (Asian Journal of Neurosurgery) | Prospective randomized comparative study | 42 | The SjvO2 values were comparable and MAP was found to be significantly lower in group P as compared to those in group S (P < 0.05). | (18) |
| Bunya et al. | 2025 | Prognostic Significance of the difference between mixed and SjvO2 after severe TBI: A post-hoc analysis of the brain hypothermia study (World Neurosurgery) | A multicenter randomized controlled trial | The same tendencies were observed in the nonsurvivor group on day 1 and in the unfavorable neurologic outcome group on day 1 and day 3, but the difference was not significant. | (19) | |
| Alten and Mariscalco | 2005 | Critical appraisal of Perez et al.: The SjvO2 or arteriovenous difference of lactate content and outcome in children with severe TBI (Pediatric Critical Care Medicine) | Critical review article | Two episodes of jugular venous bulb desaturation and abnormal values of arteriovenous difference in lactate content are associated with poor neurologic outcome in children with severe TBI — risk ratio 6.6 and risk ratio 17.6, respectively. | (21) | |
| Oddo | 2014 | Monitoring of brain and systemic oxygenation in neurocritical care patients (Neurocritical Care) | A systematic review | 281 | It is recommended to titrate individual targets of CPP, ventilator parameters (PaCO2, PaO2), and transfusion, and to manage intracranial hypertension, in combination with ICP monitoring. | (22) |
| Zhong et al. | 2021 | A review of monitoring methods for cerebral blood oxygen saturation (Journal of Healthcare) | Descriptive review | The NIRS is undoubtedly a powerful tool for cerebral blood oxygen saturation monitoring and can be used for both clinical and research purposes. | (23) |
Abbreviations: SjvO2, jugular venous oxygen saturation; TBI, traumatic brain injury; MAP, mean arterial pressure; CPP, cerebral perfusion pressure; NIRS, near-infrared spectroscopy.
5.1. Clinical Implications of Monitoring Characteristics
The "poor correlation" between SjvO2 and regional monitors in focal injuries is not a failure of the technology but a reflection of physiology. In diffuse injuries, cerebral blood flow and metabolism are relatively uniformly affected; thus, SjvO2, representing the mixed venous outflow, is a good representative of the global cerebral status. However, in focal injuries (e.g., hematomas or contusions), ischemic areas may coexist with normal or hyperemic tissue. The jugular venous blood, being drained from the entire brain, "dilutes" these regional changes and thus may not reflect severe local hypoxia, whereas NIRS, monitoring a small area (primarily the frontal cortex), can directly detect these regional abnormalities, provided the injury is within its monitoring domain. This underscores that global monitoring alone is insufficient in patients with heterogeneous injuries. In such cases, a normal SjvO2 may provide false reassurance while a focal region is ischemic. The NIRS, or ideally PbtO2, is critical in this scenario. Conversely, in diffuse injury, SjvO2 is excellent for guiding systemic therapies aimed at maintaining global oxygen delivery, such as optimizing cerebral perfusion pressure.
5.2. Towards a Practical Combined Protocol
Based on the evidence, a practical monitoring protocol could be:
1. All severe TBI patients: Consider initiating non-invasive NIRS for continuous trend monitoring and early warning of regional changes.
2. Patients with diffuse injury and high intracranial pressure: Add SjvO2 monitoring to guide global cerebral perfusion pressure management and detect global ischemia or hyperemia.
3. Patients with significant focal contusions or penumbra: If resources allow, PbtO2 monitoring for the at-risk tissue. The NIRS can serve as a non-invasive surrogate, though its values must be interpreted with caution relative to the specific lesion location.
4. Intraoperative monitoring: The NIRS is highly practical for continuous trend monitoring during anesthesia. The SjvO2 may be reserved for cases where significant blood loss or major shifts in cerebral perfusion pressure are anticipated.
The combined use of these modalities allows clinicians to triangulate the state of cerebral oxygenation, mitigating the weaknesses of each individual tool. However, implementing this combined protocol faces practical challenges, including higher costs (additional devices, consumables), the need for specialized training for staff for proper placement, maintenance, and interpretation of data, and the potential for conflicting data from multiple monitors. Interpreting such conflicting data requires a deep understanding of cerebral physiology and the inherent limitations of each technique. For instance, a drop in rSO2 on NIRS with a stable SjvO2 could indicate a true regional ischemic event or an artifact from extracranial contamination, necessitating further investigation.
5.3. Conclusions
The SjvO2 and NIRS are valuable yet distinct tools for monitoring cerebral oxygenation in TBI. The SjvO2 remains the gold standard for assessing global cerebral oxygen balance but is invasive and blind to regional changes. The NIRS provides a continuous, non-invasive window into regional oxygenation, primarily of the frontal cortex, but is less reliable for global assessment. Rather than viewing them as competitors, they should be seen as complementary components of a multimodal monitoring strategy. The optimal approach involves selecting and interpreting these tools based on the individual patient's injury pattern to guide targeted therapies and prevent secondary brain injury.
5.4. Limitations
This review has several limitations. Significant heterogeneity in definitions, thresholds, and devices across studies prevented a formal meta-analysis. Many included studies used PbtO2 as a reference standard rather than a direct SjvO2-NIRS comparison, which was necessary to comprehensively address the review question but introduces indirectness. Publication bias and the observational nature of most studies also limit the strength of the conclusions. Additionally, formatting and header hierarchy throughout the manuscript were revised to ensure consistency.
5.5. Complications
The invasive nature of SjvO2 carried associated risks, with reported infection rates of approximately 8% and thrombosis in approximately 3% of cases. The NIRS, being non-invasive, had no reported serious complications.