1. Background
The Indian government implemented a range of preventive and restrictive strategies to stop the spread of the COVID-19 pandemic, including a nationwide lockdown (1, 2). Activities involving gatherings, such as outdoor activities, travel, face-to-face classroom teaching, and family reunions, were prohibited during the COVID-19 pandemic, and people were confined to their homes (3). Travel and outdoor activity restrictions had an unavoidable impact on everyone’s lifestyle, including medical students.
Regular physical activity is essential to maintain optimum physical, mental, and psychological health (4, 5). Physical activity is defined by the World Health Organization as “any bodily movement produced by skeletal muscles that need energy expenditure including activities undertaken while working, playing, completing household chores, travelling, and engaging in recreational pursuits”. Previous research has linked the physical activity levels to the self-reported levels of depression, anxiety, headaches, feeling low, irritability, and anxiousness (6) and also to self-esteem, life happiness (7), pleasure, endurance, and attainment (i.e., perceived academic and behavioural effectiveness with peers) (8), all of which are closely related to the state of wellbeing. Several studies have examined the influence of increasing screen usage on health for all age groups throughout the pandemic period (9-11). Seguin et al., in their research conducted on Canadian children aged 6 - 12 years, found that during pandemic-related school closures, screen time rose considerably from 2.6 to 5.9 hours per day (12). Screen time is defined as the amount of time spent on various online activities using digital devices such as computers, laptops, palmtops, smartphones, tablets or any other similar devices with a screen (13).
According to various studies, lockdown has also been linked to changes in behaviour and emotional wellbeing among many populations worldwide (14-16). Alterations in everyday routine activities during COVID-19 affected people’s mental and emotional wellbeing (i.e. happiness). Students’ were also affected due to less social contact and insufficient physical activity. The switch from traditional face-to-face teaching to online also increased daily screen time, resulting in physical and emotional health consequences (17, 18). The lower physical activity and emotional disorders in medical students are expected and deserve special attention (19-21). According to a previous study, medical students had much greater rates of identified mood disorders, suicide thoughts, and psychological distress (22). Therefore, the present research aimed to determine the effect of lockdown imposed by the COVID-19 pandemic on physical activity, screen time, and emotional wellbeing among young medical students from North India.
2. Objectives
Data is limited on medical students’ lifestyle changes regarding physical and emotional health during the COVID pandemic in North India. Thus, the present study aimed to determine the effect of lockdown on physical activity, screen time, and emotional wellbeing and specify the association of physical activity and screen time with the emotional status of medical students during the COVID-19 pandemic lockdown period.
3. Methods
3.1. Study Design
A cross-sectional survey was conducted on 250 medical students of phase-I MBBS (Pre-Clinical) during the lockdown period during October to December 2020 (In India, MBBS is divided into three phases: Pre-clinical, para-clinical, and clinical). The study population was all male and female medical students of Phase-I MBBS.
3.2. Sampling Method
Every student of Phase-I of the same institute who fulfilled inclusion criteria was selected for the study purpose.
3.3. Inclusion and Exclusion Criteria
A total of 246 out of 250 students who responded to the lifestyle questionnaire regarding physical activity, screen time, and the emotional status during the home quarantine period of lockdown were included in the study after meeting the following inclusion criteria: Phase-I MBBS students of the same institute who were present on the day of data collection and had given written informed consent.
Exclusion criteria: A total of 72 students were excluded from the study due to an incomplete filled questionnaire regarding physical activity and other details.
3.4. Questionnaires
The data was collected using pre-organised structured pro-forma and questionnaires, which comprised the following parts:
(1) The General Information Schedule
(2) The International Physical Activity Questionnaire (IPAQ)
(3) The Positive and Negative Affect Schedule (PANAS) Questionnaire
A general information schedule included personal socio-demographic details (age, gender, and residence). The International Physical Activity Questionnaire (IPAQ)-short form (23) was used to assess students’ physical activity. According to the WHO guidelines (24) and the IPAQ guidelines for data processing and analyses (25), three different levels of activity (vigorous, moderate, and low) were recorded. Daily total physical activity was calculated using metabolic equivalent (MET) scores. MET scores were divided into three groups: Inactive/low (< 600 met-minutes), active (600 - 1200 met-minutes), and highly active (> 1200 met-minutes).
3.4.1. Psychometrics of the Tools (IPAQ)
According to Misra et al., IPAQ shows good reliability and validity against an objective measure of physical activity (i.e., using pedometers) in rural and peri-urban areas of North India (26). The observed concurrent validity coefficients suggested that both questionnaires had reasonable agreement (Spearman Rho of > 0.90; P < 0.0001; ICC: 0.76 - 0.91, P < 0.05) for measuring physical activity in the Indian community setting of North India (26).
The emotional status was assessed using the PANAS Questionnaire with two 10-item scales (27). One scale measures positive affect (e.g., being excited and inspired), and the other scale measures negative affect (e.g., being upset and afraid). Each item in the questionnaire was scored based on a five-point Likert scale, ranging from 1 (very slightly or not at all) to 5 (extremely), to assess the extent to which the participant felt the listed positive or negative emotions over the past week during the lockdown period. Scores for the positive affect (PA) and negative affect (NA) scales were summed (ranging between 10 - 50), with higher scores on the PA and NA subscales representing more significant positive or negative mood, respectively.
3.4.2. Psychometrics of the Tools (PANAS)
The PANAS reliability and validity of the whole positive affect (PA) and negative affect (NA) scale and subscale were found to be highly satisfactory (0.804 for PA, 0.776 for NA, and 0.658 for the full scale) among the Indian population (28).
The pre-organised structured pro-forma and questionnaire was sent via a Google Forms link to every medical student through contactless distribution on a WhatsApp group of the students. First, the study’s purpose and general instructions were explained to the students, and confidentiality was assured to them. Filled Google Forms by the students were considered willingness to participate in the study. The participants were asked to recall their physical activity, screen time (min/day), and emotional state over the past seven days.
3.5. Statistical Analysis
The dependent variables were physical activity, screen time, and emotional status (PA and NA), and the independent variables were gender, residency, and the body mass index (BMI). Quantitative variables were reported as mean and standard deviation, while qualitative variables were represented as percentages and proportions. The data were normally distributed per histogram; thus, we used a parametric test. A chi-square test was employed for qualitative variables to determine any statistical significance, while an independent Student’s t-test and the analysis of variance were used for quantitative variables. Tukey’s HSD test was used for multiple comparisons between the three groups (inactive, active, and highly active). A two-tailed Pearson bivariate correlation analysis determined the correlation between the study variables. The Statistical Software Package for Social Sciences (version 20.0) was used to analyze the data. P-value < 0.05 was considered statistically significant.
3.6. Ethics Approval
The study received approval from the Institutional Ethics Committee (No. 630/MC/EC/2020) and was registered on the Clinical Trial of India (CTRI) (No. CTRI/2020/10/028744).
4. Results
A total of 174 participants were included in the final analysis after removing duplicate responses and incomplete information regarding the participants’ physical activity and other outcome variables. The mean age of phase-I medical students was 19.56 years, ranging from 18 to 24 years, with approximately equal representation from urban (49.4%) and rural (50.57%) demographic regions. Students of both genders were included in the study with a 2: 1 response ratio of male and female participants.
The physical inactivity of the medical students during the COVID-19 pandemic was 24.7%, with a 13% difference between genders (33.3% female versus 20.2% male) during the lockdown phase, although statistically insignificant. Physical inactivity was more common in urban students (33%) than in rural students (17%), with a statistically significant difference (χ2 = 10.025, P = 0.007) (Table 1).
| Study Variables | MET Categories | P-Value | ||
|---|---|---|---|---|
| Vigorous PA | Moderate PA | Low PA | ||
| Gender | 0.138 | |||
| Male (n = 114) | 39 (34.2) | 52 (45.6) | 23 (20.2) | |
| Female (n = 60) | 15 (25.0) | 25 (41.7) | 20 (33.3) | |
| Total (n = 174) | 54 (31.0) | 77 (44.3) | 43 (24.7) | |
| Residence | 0.007 b | |||
| Urban (n = 86) | 18 (20.9) | 40 (46.5) | 28 (32.6) | |
| Rural (n = 88) | 36 (40.9) | 37 (42.0) | 15 (17.0) | |
| Total (n = 174) | 54 (31.0) | 77 (44.3) | 43 (24.7) | |
Intensity Levels of Physical Activity Stratified by Gender and Residence During Lockdown Induced by COVID-19 a
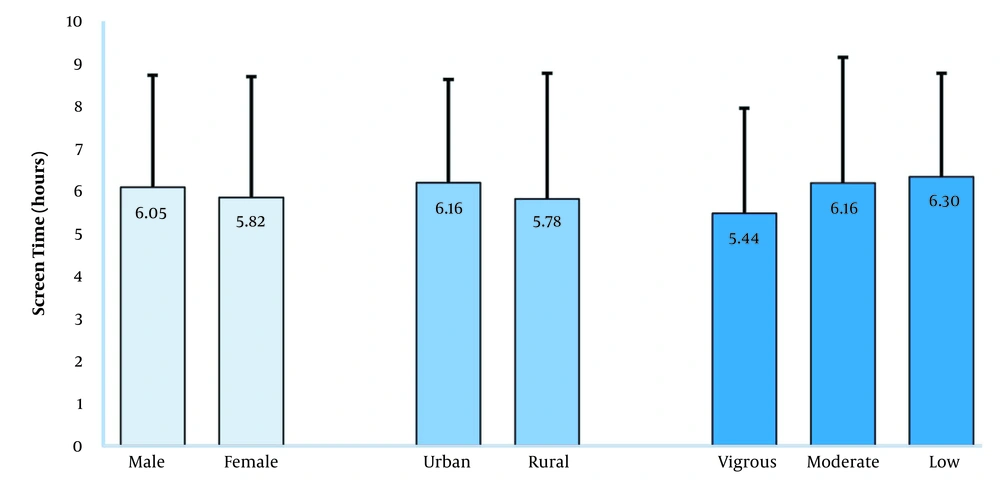
During the lockdown period due to COVID-19, the average screen time for the medical students was 5.97 hours per day (SD: 2.7 hours per day). More than half of the students (56.89%) documented the restriction by parents in terms of total screen time, while only 1/3 of the students (27.58%) disclosed the restriction in terms of content on screen. The students interacted with devices within seconds after waking up (14%), after several seconds (38%), and until the class begins (48%). The screen time was numerically more in males and urban students with low physical activity than in their counterparts, although statically insignificant (Figure 1).
The positive affect scores were higher (28.15) than the negative affect scores (21.79) in the medical students. The emotional status of the students was unaffected by gender and residency since a non-significant difference was noted. The students from rural backgrounds had a higher numerically positive affect score than the urban students. Students who engaged in vigorous exercise had a significantly higher positive affect compared to students who engaged in low exercise (Tables 2 and 3).
| PANAS Positive Affect | PANAS Negative Affect | |
|---|---|---|
| Total students (n = 174) | 28.15 ± 8.72 | 21.79 ± 8.34 |
| Gender | ||
| Male (n = 114) | 28.18 ± 8.87 | 21.50 ± 8.14 |
| Female (n = 60) | 28.10 ± 8.43 | 22.35 ± 8.68 |
| P-value | 0.954 | 0.523 |
| Residency | ||
| Urban (n = 86) | 27.42 ± 9.32 | 21.83 ± 8.54 |
| Rural (n = 88) | 28.86 ± 8.03 | 21.76 ± 8.15 |
| P-value | 0.276 | 0.956 |
| Physical activity level | ||
| Vigorous (n = 54) | 30.20 ± 8.18 | 20.76 ± 7.74 |
| Moderate (n = 77) | 28.14 ± 8.51 | 21.91 ± 7.87 |
| Low (n = 43) | 25.58 ± 9.06 | 22.88 ± 9.65 |
| P-value | 0.033 c | 0.454 |
Multiple Comparisons of the Dependent Variable (Positive Emotions) with MET Categories
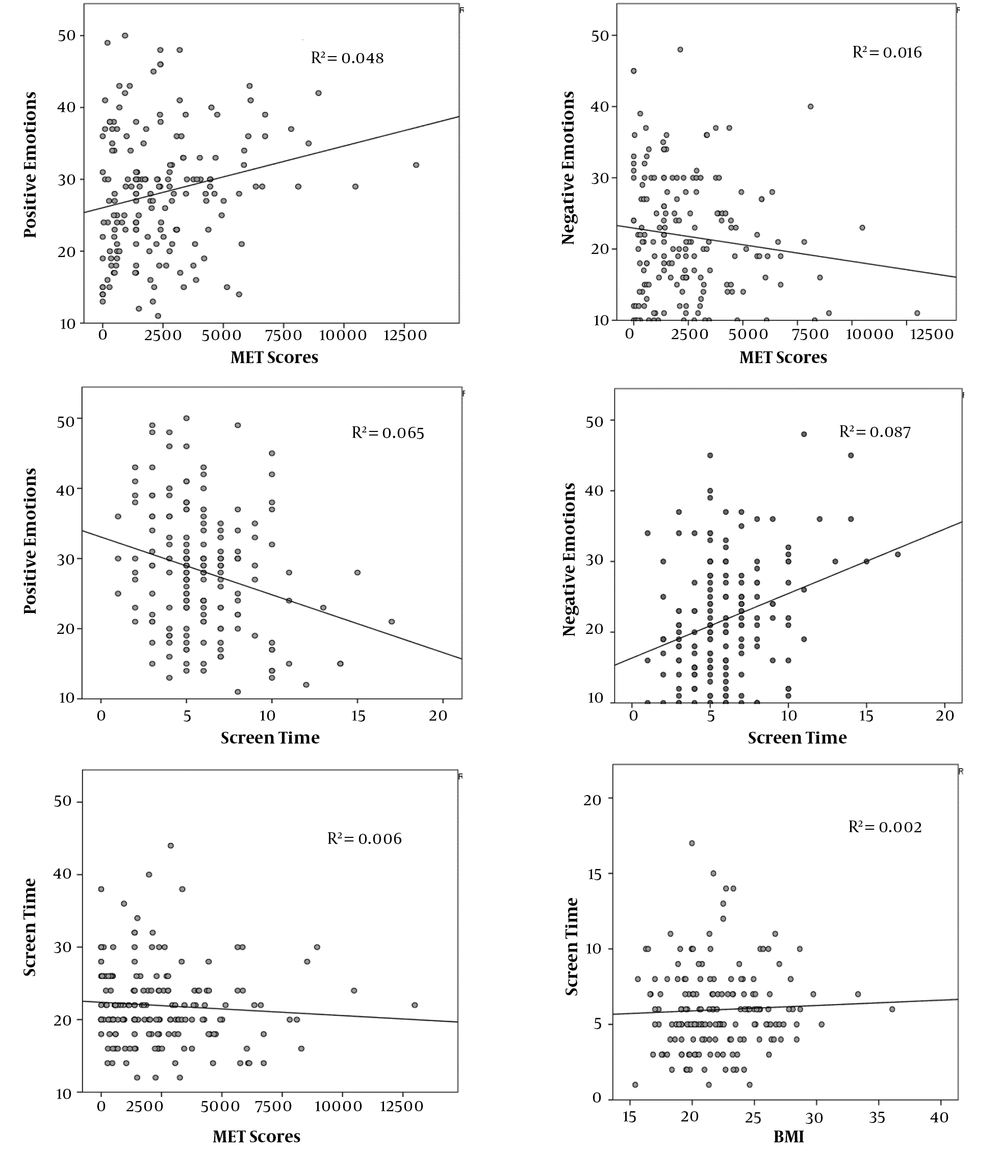
The MET scores were positively correlated with positive emotions and negatively correlated with negative emotions. The MET scores (the independent variable) explained the amount of variance (R2) in the positive and negative emotions (the dependent variable). Positive and negative emotions respectively explained 5% and 2% variance due to the students’ physical activity. Likewise, screen time was accountable for 9% variance in the negative scores and 7% variance in the positive scores. The increased duration of screen time expanded negative emotions but lowered positive emotions. Also, screen time was slightly raised with higher BMI scores but was slightly reduced with the MET scores. The correlation of the MET and BMI scores with screen time had a variance below 1% (Figure 2).
A two-tailed Pearson bivariate correlation analysis depicted that screen time was positively correlated (r = 0.295) with negative emotions and inversely associated (r = -0.255) with positive emotions. Also, the MET scores positively correlated significantly with positive emotions (r = 0.220). In contrast, the other study variables were non-significantly correlated (Table 4).
| BMI | Screen Time | Positive Emotions | Negative Emotions | MET Scores | ||
|---|---|---|---|---|---|---|
| BMI | Pearson correlation; Sig. (2-tailed) | 1 | 0.045 | -0.059 | 0.078 | 0.036 |
| 0.556 | 0.437 | 0.308 | 0.638 | |||
| Screen time | Pearson correlation; Sig. (2-tailed) | 1 | -0.255 a | 0.295 a | -0.076 | |
| 0.001 | 0.001 | 0.319 | ||||
| Positive emotions | Pearson correlation; Sig. (2-tailed) | 1 | -0.464 a | 0.220 a | ||
| 0.001 | 0.004 | |||||
| Negative emotions | Pearson correlation; Sig. (2-tailed) | 1 | -0.125 | |||
| 0.100 | ||||||
| MET scores | Pearson correlation; Sig. (2-tailed) | 1 |
Bivariate Correlations of Various Study Outcomes (n = 174)
5. Discussion
The present cross-section survey found that the medical students’ physical inactivity during the COVID-19 pandemic was 24.7%, and the average screen usage was 6 hours per day, which was unaffected by gender, residence, or physical activity. Exercise expanded positive emotions but slightly decreased negative emotions. Accordingly, the MET scores accounted for 5% positive and 2% negative variance. Moreover, screen time statistically significantly correlated with emotions, as with rising screen time, positive emotions declined (7% variance), and negative emotions were enhanced (9% variance). However, no influence of the BMI and MET scores (physical activity) was observed on screen time. Thus, lifestyle changes like more physical inactivity and more exposure to screen time influences the student’s emotional status in the lockdown period during the COVID-19 pandemic.
Physical activity must be done regularly to maintain good physical and mental health (6). Many studies found that lower physical activity was associated with the poor mental health of medical students and healthcare workers (19-21). Joy and Vincent revealed that 28.9% of medical students were physically inactive during the non-pandemic phase in a study conducted in 2019 at a medical college in Kerala, India (29). There is a strong negative relationship between sedentary behaviour (particularly screen-based activities) and many quality-of-life indices (30). Furthermore, a rise in any form of sedentary behaviour was linked to an increase in psychological complaints, such as depression or a reduced sense of wellbeing (31). According to the displacement hypothesis (32), prolonged screen time would inevitably reduce physical activity time. However, the current study does not support the displacement hypothesis, which states that excessive screen time will necessarily diminish physical activity time, as a very weak correlation was observed between screen time with the MET and BMI scores in the present study. Another research by Garcia-Hermoso et al. corroborated our findings, indicating that screen time and physical activity might alter health dimensions independently (33). Tandon et al. assessed child mental health using the Strengths and Difficulties Questionnaire and found that more screen time was correlated with higher total difficulties among younger and older children (18). Similarly, the present study found that with increased screen time, negative emotion was enhanced with a 9% variance, and gender made no significant differences in mental health. Yang et al. (34) discovered a clear dose-response link between screen-based activity use and various adverse health and emotional markers (sad, appetite, lonely, want to cry, sleeping problems, and hopelessness). The present study also supports previous research findings (5, 31) that physical inactivity is a significant risk factor for poor mental health. The present study also revealed a significant correlation between physical activity (MET scores) and positive emotions with a 5% variance, reinforcing the previous finding on the relationship between a sedentary lifestyle and psychological disorders (6-8). Furthermore, according to the present research, students engaged in vigorous physical exercise had better emotional states than those engaged in moderate physical activity.
The current outcome might be explained by the notion that online classes increase screen time and social distancing, and negligible outdoor activities in peer groups urge students to spend viewing entertainment on the screen. It is observed that an increase in screen usage has an inevitable detrimental influence on students’ emotional wellbeing. There is less awareness in society about mental health and the impact of screen time on emotional wellbeing. In this technically advanced era, it is necessary to address students’ mental health. The unwise use of screen exposure should be discouraged. The current study observed that physical exercise improved positive emotions, but screen time had a more significant negative impact on students’ moods, of which students, instructors, administrators, and family members might be unaware.
5.1. Strengths
The current research examined how increased screen time exposure during online teaching or other sources affected the medical students’ mental health. The present study’s findings highlight the importance of early health promotion and fitness advice during home quarantine. This might be helpful in future policy and programmatic health promotion planning in the event of health emergencies management.
5.2. Limitations
The study’s primary limitation may be recall bias, as the students had to recall physical activities and screen time usage hours during the lockdown period. Even though a WHO-approved physical activity questionnaire (IPAQ-S) with good reliability and validity was employed, self-reported data on physical activity may not be as accurate as pedometer readings. Also, as the study only included younger students, age considerations may have influenced the findings.
5.3. Conclusions
The present study concluded that the physical inactivity of the medical students during the COVID-19 pandemic was 24.7%, and the average screen time usage was six hours per day during the lockdown phase, with all categories of students being equally exposed to increased screen time. Students who were more physically active and had less screen time exposure presented a more positive effect on emotions, and a reverse trend was observed for their counterparts. Physical activity explained 5% of the variance in positive emotions and 2% of the variance in negative emotions. Also, screen time accounted for 9% of the variance in negative emotions and 7% of the variance in good emotions. Physical activity and BMI were not linked with screen time usage. Thus, physical inactivity and screen time emerged as major and independent risk factors for the students’ mental health.
5.4. Future Recommendations
This is an objective study based on a questionnaire; thus, for validating and generalising its results in future, we recommend using subjective methods like using a pedometer for recording physical activities. Similarly, authentic software applications can be used for recording screen time. Moreover, we can record EEG and PET scans for accuracy and validity for emotional wellbeing.