1. Background
“Much education today is monumentally ineffective. All too often, we are giving young people cut flowers when we should be teaching them to grow their own plants.”
- John W. Gardner.
This phrase strongly highlights how education delivery methods are perceived in the 21 century. It contradicts the traditional concept of learning that happens between a qualified teacher and a student (1). Furthermore, many have shown that learning amplifies when one shares knowledge or skill by teaching others (2).
Medical graduates are expected to be work-ready with technical skills and abilities to be safe and competent, alongside possessing the interactional and interpersonal skills to communicate and function effectively (3). These expectations are described as ‘transferable skills’ (4), which generally consist of key competencies (5), generic attributes (6), or capabilities (7) designed to foster life-long learning. The “peer-assisted” and “self-directed’ learning methods are among the five teaching methods in undergraduate courses that have been explored and cited to be beneficial in encouraging lifelong learning, reflective practice, and fostering self-awareness (8). Peer learning encourages greater understanding as they share similar discourse while reinforcing their own learning by managing and organizing learning for others (9).
Various peer learning methods became popular over the last 20 - 30 years and were implemented at various levels of education, i.e., primary to tertiary and even postgraduate (10). Peer learning has already been proven to be an effective tool in education. However, peer learning has often been institution-centric, a top-down approach to further enhance and complete the medical training experience, while grassroots student-driven projects are unfortunately poorly sustained.
The method utilized in our clinical training is ‘peer-assisted learning,’ defined as ‘students learning from and with each other in both formal and informal ways’ (11). This ‘reciprocal’ method aims to assist students with the same interest and expectations in learning from each other while in clinical experiential learning. Due to the restriction in physical teaching and learning and limitations in students’ placement for authentic clinical experience during the COVID-19 pandemic, learning has been modified by moving it online.
2. Objectives
The study aimed to evaluate medical students’ confidence through the peer learning program and establish an appropriate student-driven peer learning framework.
3. Methods
3.1. Peer Learning Execution Process
3.1.1. What Is the Program – The IMU Consultoid Program
‘Consultoid’ is a peer-assisted learning program founded on an idea of a clinical year student. Over the two years, the platform has involved over 200 students within the university. Moreover, Consultoid successfully reached out to over 6,000 participants globally during the COVID-19 lockdown, when multiple online peer learning sessions catered to all medical students.
Consultoid combines the experience of fresh graduates and senior clinical students, simulating the role of consultants, to guide junior clinical students through clinical case-based discussion and practical workplace simulation. During these simulated rounds, patients are fully clerked and examined beforehand. The issues and management of the identified patients are reviewed and discussed within the team.
3.1.2. Recruitment and Implementation
Traditionally, proctoring programs involved more advanced undergraduates with recently demonstrated proficiency, tutoring undergraduates with less experience on a one-on-one basis (10). Our program adopted this concept but operated in groups. The eighth and ninth semester (year 4 and 5) students are assigned as peer mentors, while the sixth and seventh semester (year 3 and 4) students are peer mentees. Peer mentors are paired and facilitate the learning of four peer mentees. The participants who volunteered as peer mentees spent a semester, i.e., six months, with the peer mentors. After that, the members may be reassembled into a new group, or they may choose to remain in the same group.
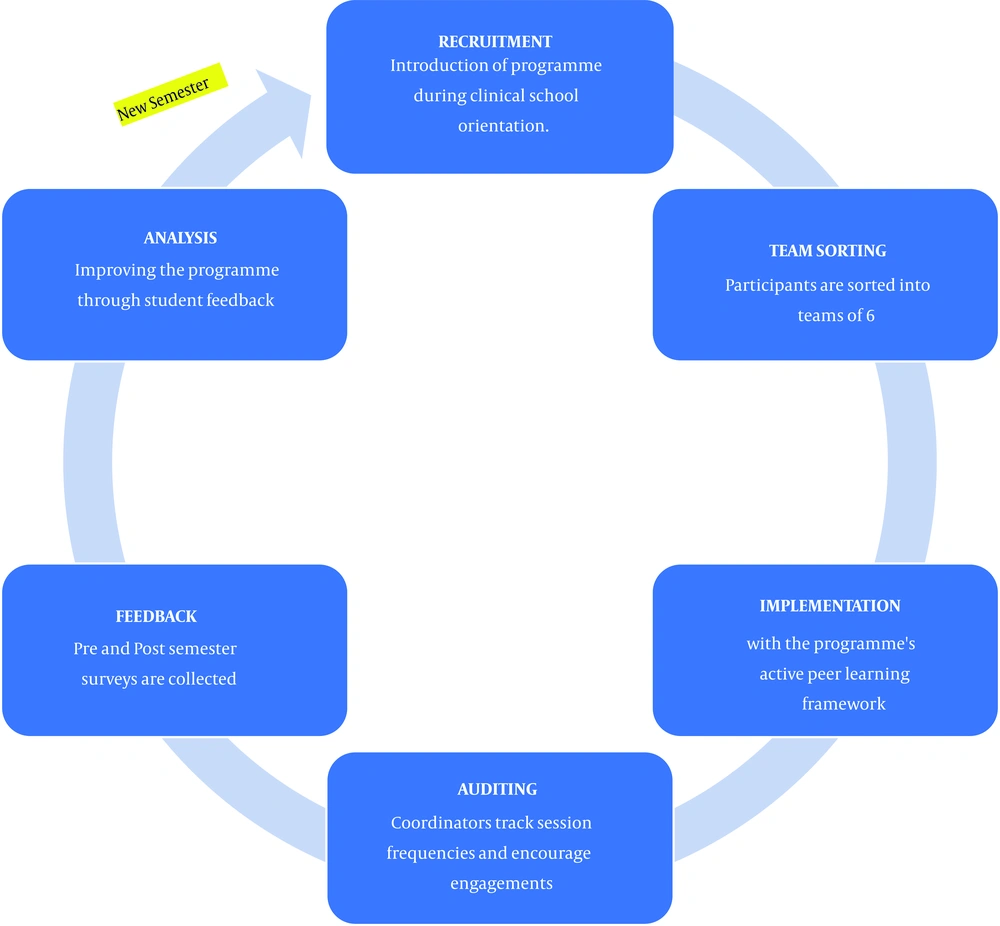
Working in a team boosts the building of transferable skills such as providing, receiving feedback, and critical appraisal, skills useful in medicine and other areas of life. Proctoring via simulated ward rounds also paves the way for peer mentors to provide immediate feedback to peer mentees regarding their history taking and examination skills. Feedback from mentors regarding the mentees’ clinical skills included both oral and written forms. This process cycle is represented in Figure 1.
Consultoid initially started with six volunteers as peer mentors to now about 14. The opportunity to participate is open to all students via multiple media. Marketing about the platform is also incorporated into the orientation program with the support of the university’s management. The choice of groupmates is based on individual preference for learning styles and scheduling compatibility. The teams will then proceed to conduct their own small team learning sessions, with the batch coordinators facilitating and auditing their progress. Junior medical students who were once participating as peer mentees will be upgraded to the role of peer mentors upon reaching the higher semesters. Participation is based on volunteerism with no financial incentive. The coordinators produced program guidelines to ensure that both peer tutors and tutees were informed of their roles, responsibilities, and expected outcomes.
3.2. Feedback and Evaluation for Enhancement
It is vital that a Plan-Do-Check-Act (PDCA) cycle exists to evaluate the platform’s effectiveness to ensure that we have achieved the expected outcome (12). The evaluation process helps the organizing team to reflect on necessary modifications and if newer methods need to be implemented. Plans of action involve revision of program structure, guidelines, and selection of tutors. Based on feedback from stakeholders and special circumstances (e.g., the COVID-19 pandemic), regular updates to the program guidelines are carried out.
3.3. Evaluation Method of IMU Consultoid Program
This study is performed by a nested mixed methodology design. The conceptual framework is derived from the qualitative theme for replication in future studies.
We recruited peer mentors and mentees for the evaluation exercise from 2019 until 2021. Informed consent was taken from participants who agreed, and all information and data were kept anonymous, private, and confidential by the six researchers. As this study was conducted as a pilot study and the recruitment of peer tutors was voluntary, ethical approval was not required.
Two sets of data are collected and analyzed. Set A represents the pre- and post-feedback from the internal participants consisting of peer mentors (senior students) and peer mentees (junior students). Set B contains feedback from internal and external participants after every online peer teaching over an academic semester (six months). The data were analyzed qualitatively and quantitatively.
3.4. Quantitative Analysis Methodology
The quantitative method uses the ‘five-point Likert scale’ with 1 being unconfident and 5 being the most confident. It is a pre- and post-self-assessment of clinical competencies: Communication (case presentation and summary skills), psychomotor, management, clinical reasoning, and self–confidence and leadership. The pre-test scripts were distributed to participants before the learning sessions, and the post-test was done within a week after completing all the sessions. There were about four months between the two tests. Paired t-test was used to analyze the difference between the two tests.
3.5. Qualitative Analysis Methodology
The qualitative method utilizes thematic analysis of the open comments from sets A and B, based on four factors of success or failure of its execution:
(1) Timing of activities allowing adaptability
(2) Peer teachers’ ability to engage with the learners
(3) Promoting participants’ intrinsic and extrinsic motivation
(4) Relevance of program content
The analysis was done using Braun and Clarke’s six-phase framework (13) The open comments were collected in written forms, and the items of interest were noted, then coded across the entire data set. Common themes were searched for. The themes were reviewed by mapping the provisional themes and their relationships. The themes were defined, and the analysis was finalized.
4. Results
4.1. Quantitative Analysis Results
We received 39 and 12 responses in set B from the peer mentee and mentor groups, respectively. The surveys consist of similar skills with some variations.
4.1.1. Peer Mentee Group Results Analysis
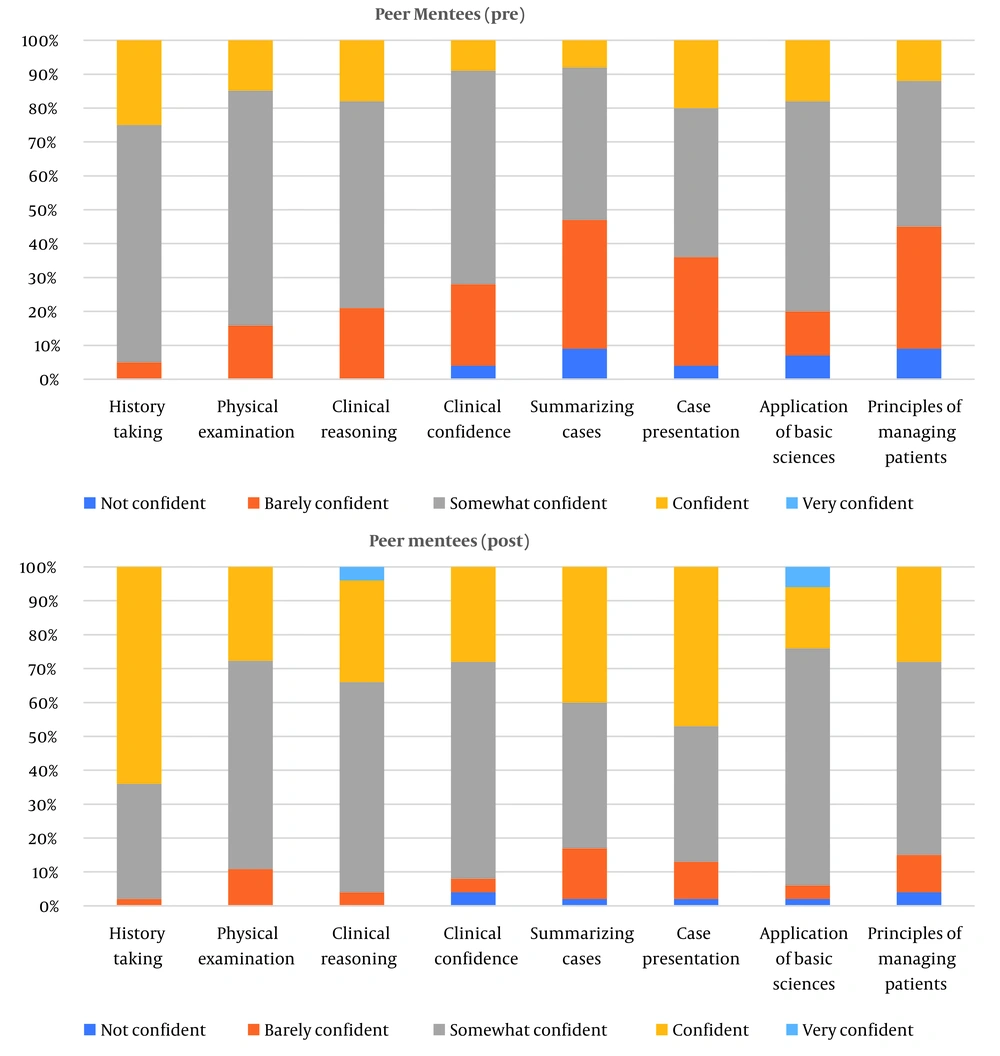
There was a total mean overall confidence increment of 15.5. The increase in overall confidence was statistically significant (P = 0.026). Table 1 and Figure 2 show the results of the mentee group pre- and post-program implementation. There was an increase of confidence in all skills, with the highest being in the communication aspects, from ‘somewhat confident’ to ‘confident’: History taking (39%), case summarizing skills (32%), and case presentation (27%). In terms of clinical reasoning skills, there was a marked improvement of 16% from ‘barely confident’ to ‘confident’ and ‘very confident’. There was also an encouraging improvement of confidence by 30% for management skills.
| Skills and Likert Scale | Pre (%) | Post (%) | Difference (%) |
|---|---|---|---|
| History taking | |||
| Not confident | 0 | 0 | -39 |
| Barely confident | 5 | 2 | |
| Somewhat confident | 70 | 34 | |
| Confident | 25 | 64 | +39 |
| Very confident | 0 | 0 | |
| Physical examination | |||
| Not confident | 0 | 0 | -13 |
| Barely confident | 16 | 11 | |
| Somewhat confident | 70 | 62 | |
| Confident | 15 | 28 | +13 |
| Very confident | 0 | 0 | |
| Clinical reasoning | |||
| Not confident | 0 | 0 | -16 |
| Barely confident | 21 | 4 | |
| Somewhat confident | 61 | 62 | |
| Confident | 18 | 30 | +16 |
| Very confident | 0 | 4 | |
| Overall clinical confidence | |||
| Not confident | 4 | 4 | -19 |
| Barely confident | 24 | 4 | |
| Somewhat confident | 63 | 64 | |
| Confident | 9 | 28 | +19 |
| Very confident | 0 | 0 |
4.1.2. Peer Mentor Group Results Analysis
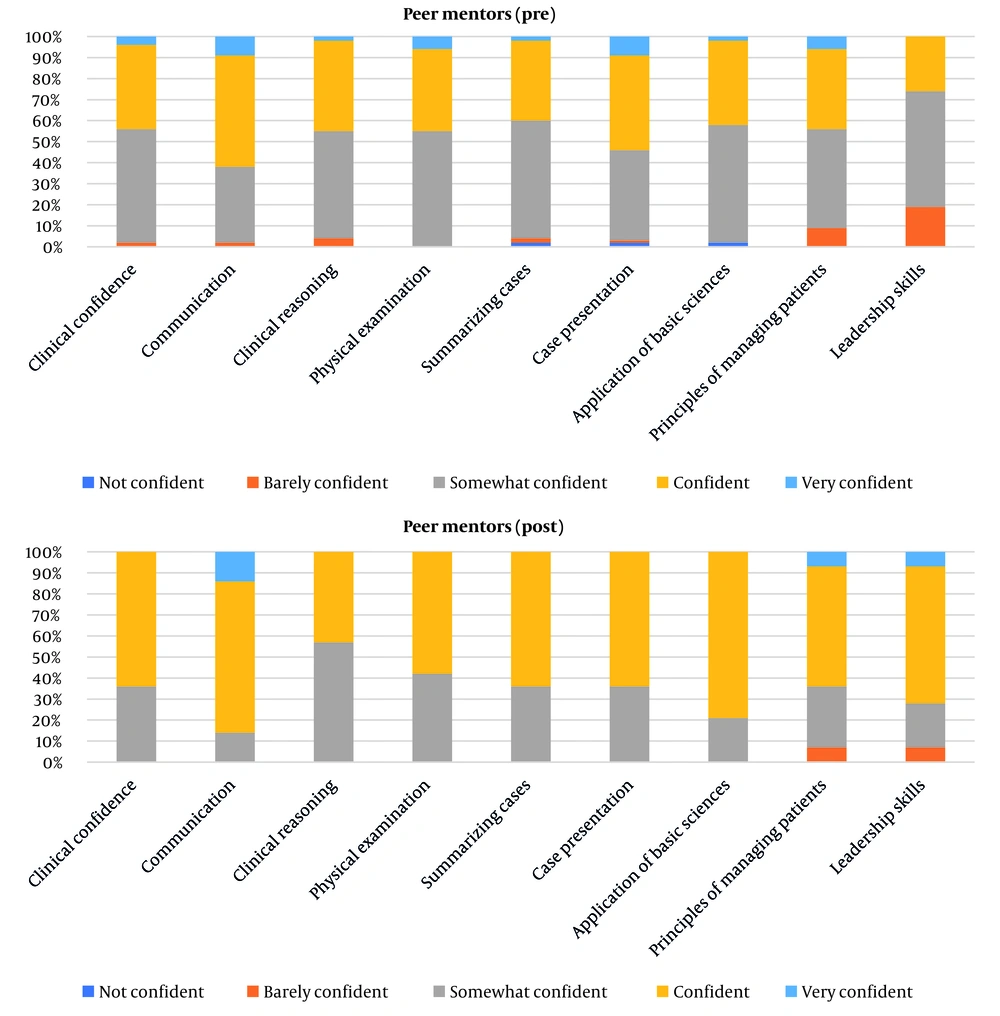
There was a total mean overall confidence increment of 14.4 (P value = 0.012). Among the peer mentors, the biggest increase in the percentage of confidence was in leadership skills at 45%. The second highest increment was in basic science application at 39%. Table 2 and Figure 3 represent the results of the mentor group pre and post-program implementation.
| Skills and Likert Scale | Pre (%) | Post (%) | Difference (%) |
|---|---|---|---|
| Clinical confidence | |||
| Not confident | 0 | 0 | -20 |
| Barely confident | 2 | 0 | |
| Somewhat confident | 54 | 36 | |
| Confident | 40 | 64 | +20 |
| Very confident | 4 | 0 | |
| Communication | |||
| Not confident | 0 | 0 | -24 |
| Barely confident | 2 | 0 | |
| Somewhat confident | 36 | 14 | |
| Confident | 53 | 72 | +24 |
| Very confident | 9 | 14 | |
| Clinical reasoning | |||
| Not confident | 0 | 0 | +2 |
| Barely confident | 4 | 0 | |
| Somewhat confident | 51 | 57 | |
| Confident | 43 | 43 | -2 |
| Very confident | 2 | 0 | |
| Physical examination | |||
| Not confident | 0 | 0 | -13 |
| Barely confident | 0 | 0 | |
| Somewhat confident | 55 | 42 | |
| Confident | 39 | 58 | +13 |
| Very confident | 6 | 0 |
4.2. Thematic Analysis Results
We extracted 263 comments with keywords that could be categorized into four themes. The more common comments were on two themes, ‘Peer teacher’s ability to engage with learners’ and ‘relevance of program contents’. The categorization of keywords is shown in Table 3.
| Theme | Students’ Comment |
|---|---|
| Timing of activities allowing adaptability | Really appreciate the efforts … even during the lockdown from our homes! I really like… that these lectures are recorded, making it accessible for everyone... It is really convenient … Thank you for rescheduling the event time to fit the participants’ buka puasa (breaking fast) hours during Ramadhan! I joined the program during the waiting period of housemanship… keeping the schedule fully flexible for all of us. |
| Peer mentors’ ability to engage with the learners | I like how Dr. L sustained our attention with his humor and the Q&A in between. The interactive session is very interesting. Fantastic, I enjoyed the session and loved the fact you answered all our questions! This session is very interactive and fun, I love it to bits! Thank you for your lecture, I love how you arrange each disease into a case discussion format. I love the Kahoot! session. I like how the speaker is responsive. The humor in the slide as well the audience. It was very interactive and easy to follow, can’t think of any improvements! |
| Promoting intrinsic and extrinsic motivation | Students are more willing to open up and ask questions amongst peers without pressure from faculty members… encourages me to be better prepared as I teach my juniors, making me more confident overall in my knowledge and skills. We are guided by seniors who are passionate and patient...this platform does exactly that it helps us all be better future doctors. |
| Relevance of program content | Haven’t had my psychiatry posting yet, but the session today definitely gave me an insight on what to expect ... I’m still not very familiar with the topic of psychiatry, but N. did a fantastic job in explaining the important points...student with not much knowledge about fluid management, but surprisingly the class was really simple and easy to understand. I do feel like I can better approach my ECG interpretations after some more practice. I’m so glad he went into detail in terms of anatomy… It’s always great when a lecture adds creative ways to improve understanding of a topic. Provides ground for teamwork, similar to the teams in the wards. It facilitates working together and sharing knowledge… allowed me to acquire skills I wouldn’t have gained otherwise. It also helped correct many misconceptions that I had… the program simulates a similar learning experience in the working environment as a junior or senior doctor while… helps to foster confidence, analytical skill, and communication skills… a great platform, especially for students who need extra exposure in these times of limited clinical exposure. |
4.3. Timing of Activities Allowing Adaptability
Participants found the timing of the sessions to be flexible.
“Really appreciate the efforts even during the lockdown from our homes! I really like that these lectures are recorded. Thank you for rescheduling the event time to fit the participants’ buka puasa (breaking fast) hours during Ramadhan!”
4.4. Peer Mentors’ Ability to Engage with the Learners
Many speakers participating in the peer lecture series could engage the audience and share their knowledge effectively.
“I like how Dr. L sustained our attention with his humor and the Q&A in between. I love the Kahoot! session.!”
4.5. Promoting Intrinsic and Extrinsic Motivation
The encouraging environment of this framework promotes positive interdependence amongst students.
“Students are more willing to open up and ask questions amongst peers without pressure from faculty members.…encourages me to be better prepared as I teach my juniors.”
4.6. Relevance of Program Content
The topics that were covered were relevant to the undergraduate medical curriculum.
“I do feel like I can better approach my ECG interpretations after some more practice.
5. Discussion
The “Consultoid” program is designed to promote questioning, clarifying, practicing, demonstrating, and justifying under conducive conditions to encourage independent deep learning that is required while coping with the dynamic changes of the medical world (14). This is best supported by nurturing them with skills to actively participate, be deep learners, and be reflective practitioners (15).
Though there are contradictory findings on peer learning’s impact on peer relationships, it is generally found to improve the learners consistently (16, 17). We have also found that it removes potential competitiveness among peers and creates a safe environment for professional and personal growth, especially in a hectic clinical environment with a lack of supervision due to the availability of trainers (18).
The Consultoid program is formalized without the strict structure of hierarchical lines where senior and junior students can interact comfortably. It fits into the concept of collaborative learning, which provides cognitive gain and creates a network to share wisdom, aiding students’ transition to clinical training (19, 20).
The quantitative data analysis from peer mentors and mentees showed a significant improvement in overall confidence, communication skills, and clinical reasoning. The peer mentors showed the highest increment of confidence level in leadership and application of basic science skills. This reflects the roles of mentors in organizing, planning, and executing the program. A similar study by Putri and Sumartini in a nursing program in Indonesia showed significant improvement in students’ competencies, especially critical thinking skills and professional approach (21). The peer mentors also reported improved knowledge, teaching skills, and confidence (22).
The sustainability is supported by the provision of training by the university to peer mentors for effective tutoring and the cultivation of new learning culture among students. During the COVID-19 pandemic, the learning methods shifted from the clinical case-based discussion, demonstration of physical examination, or management skills within a small group to online group discussion focusing on applying knowledge, clinical reasoning, and management. The attraction remains within the relevance of program contents and commitment from the coordinators and peer mentors. The advancement of technology has also permitted global networking via the teleconferencing platform provided by the host institution.
Previous literature has highlighted several critical components in creating effective peer learning. These include joint decision-making and highly individualized learning (23), formal inclusion in the academic program (24), less influence from the authority (25), decentralized learning roles and power (24), and importance of self-management alongside team leading (9).
5.1. Deriving a Framework of Sustainable Student-Driven Peer Learning
Guided by the thematic analysis results, a framework is developed to allow successful replication of such a platform. Figure 4 shows the conceptual framework intended to guide the sustainability of an entirely student-driven program. The framework emphasizes several core features: relevance to clinical practice, high flexibility and accountability, and participation based on volunteerism.
5.1.1. Encouraged Participation
Keeping it relevant to what benefits participants is the key to ensuring continuous recruitment of peer mentors and mentees. It is vital to allow participants to take charge of their own scheduling, working style, team dynamics, and learning outcomes (26).
5.1.2. Team Building and Networking
Berk (27) stated that young students’ participation in a program like this is usually associated with the recognition, improvement of skills, and performance evaluation, which are consistent with lifespan development theories. This aligns with the analysis made from the open comments where some felt that connecting with peers of similar or slightly higher maturity and capabilities has encouraged motivation to learn further.
5.1.3. Encouraged Motivation
Students are likely to recognize the values of peer learning when having the insights of needing more learning experience in actual practice, which could not be obtained through only formal teaching and learning. This should motivate students to intrinsically seek an alternative to improve their clinical competence to ensure patient safety (21). Rewarding participants, support from the organization or institution, and continuous evaluation for program enhancement are required.
5.1.4. High Adaptability
During the COVID-19 lockdown, hospital access was heavily restricted. The coordinating team produced a modified guideline for the participants to move sessions online. The program served as a supplement during the gap of training disruption.
The online “Consultoid Peer Teaching” sessions allowed students to share knowledge on specific clinical topics through webinars. A total of 48 sessions were carried out over four months. The initiative garnered a total outreach of over 6,000 students worldwide, involving medical students, fresh graduates, and registrars from Malaysia, the United States, the United Kingdom, Singapore, Russia, Australia, and the Republic of Ireland. The online platform allowed medical students to interact and network between medical schools, breaking down traditional barriers of the locality.
Details of the components of the framework are as follows:
(1) Relevance to clinical practice: The program allows the transfer of skills from simulated clinical learning during the pre-clinical phase to encounters with real patients in clinical practice.
(2) Peer Mentoring: The senior medical students can pass on their clinical knowledge to the junior medical students. This mutualistic system boosts the clinical confidence of all participants and their intrinsic motivation to become better clinicians.
(3) Team-based reciprocal learning: The program is set in teams conducting their own simulated ward rounds, heavily emphasizing teamwork, peer feedback, and evaluation.
5.2. Limitations
This study has several key limitations, namely the small sample size, potential sample selection bias, potential harm from peer learning, and the Dunning-Kruger effect (28). This is a preliminary study; hence, further study of a larger sample size across multiple centers should be considered.
The participants joined the program voluntarily, resulting in convenient sampling and potential inherent biases. Generalizing the program’s success to all student groups will require complete randomization of sample selection.
This study lacks a higher level of evaluation (i.e., levels 3 and 4) of the Kirkpatrick evaluation model due to its short study duration. A longer-term longitudinal study of various stakeholders is required to show a true and reliable impact on participants’ performance. Following up on the participants’ academic results and workplace performance is being planned.
Peer learning has always been controversial for its potential to harm the learning process (29). Misinformation cannot only affect students’ academic performance but may also influence patient care negatively. Active auditing and regular review of teaching-learning content are required to ensure content accountability, validity, and quality.
Finally, as the study was primarily based on self and peer evaluation, the apparent positive results gained from the program could manifest the Dunning-Kruger effect (28). As participants progress through the program, the perceived improvement may not be proportional to the actual objective improvement due to limited experience as aspiring clinicians. This effect can be mitigated through a longer-term longitudinal study to reflect the true clinical improvement of the participants.
5.3. Conclusions
Peer learning benefits students’ learning outcomes and overall personal development. It should supplement any formal teaching-learning of a stressful program with a possibly threatening learning environment. A systematic approach to implementing peer learning in medical school may alleviate the reservations in the practice of peer evaluation (30).
We have shown that the major factors to drive peer learning programs are flexibility, adaptability, and evaluation or auditing for enhancement. The recruitment of participants and the execution process need clear guidance and promotion. Nevertheless, support from faculty or institution is undeniably crucial in areas of training to improve teaching, mentoring, or coaching techniques. We hope the Consultoid framework will assist future educationists and researchers in replicating the peer mentoring programs at their respective institutions to generalize our results.