1. Background
The critical central themes in the career and professional identity includes one’s professional self-concept based on attributes, beliefs, values, motives, and experiences.
In the literature (1), professional identity formation has become a key focus of medical education (2). To elucidate the process of work identity formation, social development and learning theories may help, although many experiences comprising physician education occur in groups at the medical workplace. Medical students endeavor to develop their professional identity. For example, they reconcile their ideal concept of a physician with modern medical realities (3). Everyone can compare expectations and ideals only in the workplace, where essential exposure changes into reality (4). An essential strategy for fostering PIF may be early clinical experiences (5).
Bandura’s (1969) social learning theory identifies learning as observing others, particularly peers’ behaviors and role models. This can be realized through endeavors to optimize learning during these experiences. When they commence their residency, this professional identity focuses on the graduate medical training they receive and their working environment (6).
Recently, medical educators have widely acknowledged professional identity construction as an important goal in medical education, primarily focusing on constructing the “doctor” identity amongst medical students (7). To develop professional identity, learning opportunities should be provided for learners to directly participate in experiences similar to their future professional roles and give them the opportunity to allow them to reflect on, practice, and manage such affairs and require learners to take responsibility for the experience and train them. Therefore, considering the abovementioned points, medical education should foster professional identity formation, but there is much to be learned about supporting learners in developing their professional identity. This study examined the role experiences that support professional identity development at the University of Tehran Medical Sciences.
2. Objectives
This study aimed to explain the role of experience in shaping the professional identity of medical residents of the Tehran University of Medical Sciences.
3. Methods
This study had a qualitative design and conventional content analysis with the aim of understanding and discovering data by semi-structured interviews with residents of Tehran University of Medical Sciences hospitals (Imam Khomeini Hospital, Sina Hospital, Shariati Hospital, Moheb Yas Hospital, and Pediatric Medical Center who had important responsibilities in assistant training. The interviews were saturated with 15 assistants, and three other interviews were continued to obtain more information and details and clear up some ambiguities in up to 18 interviews. The interviews were conducted by appointment and choosing a place for the interview inside the hospital (conference hall, pavilion, restaurant, coffee shop, etc.) according to the choice of the assistants. At the beginning of the interviews, the study’s objectives were explained to the assistants, and their consent was obtained for voice recording. Assistants were assured that the recorded material would remain anonymous and confidential. Also, to confirm the statements of the assistants or the need for further interviews and obtain more information, consent for subsequent contacts was obtained at the end of the interviews. An interview guide was used to ensure all topics would be precisely covered in the interviews. The questions were designed in a manner that the participants could freely express their thoughts. Research questions included: what experiences affected your professional identity formation during the residency courses? Participants were asked to provide examples if the contents were not clear. All interviews were recorded, listened to, and, at the earliest opportunity, typed word by word and analyzed before implementation before the next interview. Data were analyzed manually using the content analysis method. Since the content analysis method was used to determine the specific words and concepts in texts, which the data was reduced and given structure and order (8), the interviews were read several times to generate a general sense. Then, after specifying the initial codes in the right margin of the text, data were gathered in an encoding table.
Consequently, the following data set was formed, and coding was continued. Partial codes were categorized into more general subsets, thereby reducing a large number of primary codes. Then the codes were categorized based on similarity, and subclasses were formed. Similar classes were arranged next to each other, merged in similar characteristics, and entered into another significant class labeled as the main class. To ensures the validity and reliability of the study and to ensure the validity of the findings by establishing a favorable relationship with the participants, the research team members agreed on how to conduct the interview, codify the texts, and describe the results in depth using the views of external observers; thus the findings were obtained. In this study, as shown in Table 1: 18 medical residents 26 - 40 years old (male and female) participated from four major specialty groups, namely obstetrics and gynecology, surgery, internal medicine, and pediatric.
| Participants | Gender | Age (y) | Year of Specialty | Resident’s Specialty |
|---|---|---|---|---|
| 1 | Female | 31 | 3 | Pediatric |
| 2 | Female | 26 | 1 | Pediatric |
| 3 | Female | 32 | 4 | Pediatric |
| 4 | Female | 27 | 2 | Pediatric |
| 5 | Female | 36 | 4 | Obstetrics and gynecology |
| 6 | Female | 32 | 2 | Obstetrics and gynecology |
| 7 | Female | 32 | 3 | Obstetrics and gynecology |
| 8 | Female | 28 | 1 | Obstetrics and gynecology |
| 9 | Male | 26 | 1 | Internal medicine |
| 10 | Female | 27 | 2 | Internal medicine |
| 11 | Male | 29 | 3 | Internal medicine |
| 12 | Female | 30 | 4 | Internal medicine |
| 13 | Male | 30 | 4 | Surgery |
| 14 | Male | 28 | 2 | Surgery |
| 15 | Male | 30 | 1 | Surgery |
| 16 | Female | 40 | 3 | Surgery |
| 17 | Male | 33 | 2 | Surgery |
| 18 | Female | 31 | 2 | Obstetrics and gynecology |
4. Results
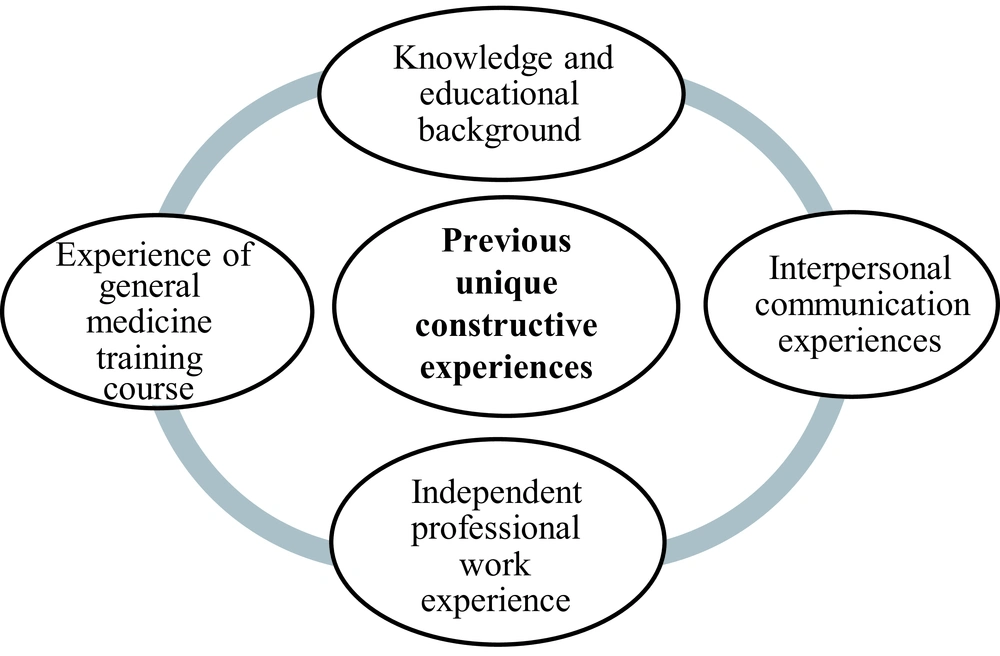
According to data analysis demonstrated in Table 2, previous unique constructive experiences at the Tehran University of Medical Sciences were acquired during the residency period. They were categorized into four main categories, namely interpersonal communication experiences, independent professional work, general medical education course and knowledge, and educational background of the unique experiences of each residency in professional development and increasing his responsibility is involved.
| Previous Unique Constructive Experiences | Values |
|---|---|
| Interpersonal communication experiences | |
| Practice in communication | Many patients and referring companions; A variety of exposure to different diseases; Collaborating with various levels of assistantship (leveling) |
| Having a partner (couple/married) | More adaptation in married people |
| Independent professional work | |
| Working with a general medicine degree | Independent practice before the assistantship previous healthcare responsibilities |
| The forced scheme | Having full responsibility and accountability opportunity to identify interest |
| General medical education course | |
| Symbolic events | Participate in the white coat ceremony; Early exposure in clinical practice |
| Learnt competencies of GP | Learned knowledge of general medicine course; Learnt skills available in medicine course |
| Beneficial reforms and integration in general medical education | Providing community service during learning Teamwork plans |
| Knowledge and educational background | |
| The education level among families | Parents role modeling Learning within the family Performance promotion under stress |
| The education quality level among schools and Institutes | Decision-making training Self-confidence promotion Problem-solving training |
In this study, based on data analysis, as shown in Figure 1, previous unique constructive experiences included four main categories of interpersonal communication experiences, independent professional work experience, experience of general medicine training, and knowledge and educational background.
4.1. Interpersonal Communication Experiences
Interpersonal communication experiences are a subset of the former unique constructive experiences.
4.1.1. Communication Practice
The study showed that one of the critical factors in the formation of the residents’ professional identity is the experience of practicing and repeating a treatment many times on patients with diverse diseases who were referred to the teaching hospitals. Participant No. 1 commented: "It is a great blessing that our country has great teaching hospitals where the multiplicity of cases means that our residents see many cases. Books are written about different diseases in Western countries. Physicians of the Western countries may not see many diseases, but our trainees see them all, and this is a real blessing" (female, pediatric resident, third year). Participant #8 commented on the practice: “we acquire a lot of knowledge, skills, and good practice by communicating with residents and assistants at different levels” (female, obstetrics and gynecology resident, first year).
4.1.2. Having a Partner (Couple/Married)
The data demonstrated that some assistants considered being married as one of the factors affecting coping and adaptation in the workplace. "I think it makes an impact; even I can say that people who are married and have children who commence this period are very adaptable, and the outcomes are different compared to someone who is not married," participant #13 (female, obstetrics and gynecology resident, second year).
4.2. Independent Professional Work
Independent work was one of the most important experiences that participants believed affected their professional identity.
4.2.1. Working with the General Medicine Degree
The findings showed that assistants who had delivered services in the community after graduation from general medicine were institutionalized in their medical professional identity and were practical and progressive in the identity of their medical specialty. Participant No. 17 stated: “that they worked as doctors who had a significant impact on the formation of their professional personality; and I saw in different people that those who had this experience before commencing the residency had a constitutional difference with those who had no such experience (male, orthopedic resident, first year).
Participant No. 3 also said: “the first time we came to the hospital emergency clinic, we saw a patient, and maybe we didn't have anything. It was the experiences of the general medicine course that helped so much” (female, pediatric resident, fourth year).
4.2.2. The Obligatory Scheme
Based on the results, the experience of having complete responsibility and accountability for serving in the obligatory scheme was important in professional identity development.
Participant No. 18 also stated about that: “I practiced on a mandatory plan in the emergency clinic of the hospital for two years, I took shifts, and I became competent in management and providing care” (female, surgery resident, third year).
Participant No.19 said: “The obligatory scheme also helps the process of professional identity formation and can help one in choosing their future career better. I went to the obligatory scheme after medicine, and I just realized what field I was suitable for; I mean, in fact, my interest in obstetrics and gynecology was tested there” (female, obstetrics and gynecology resident, first year).
4.3. General Medical Education Course
The general medicine training course creates constructive experiences that include: Symbolic events and the acquired capabilities of general medicine, and beneficial feedback and integrations in general medical education.
4.3.1. Symbolic Events
The findings showed that one of the first effective contributors to forming a professional identity is holding symbolic events such as celebrating the white coat and briefings on medical responsibilities. Wearing a white coat and a imagining its responsibilities is a novel experience for fresh students. "White, blue and green in the hospital .... accepting the color of the dress and the symbolic celebration of the white coat celebration (dress coating) creates responsibility and commitment towards it."
The study’s findings showed that briefings on medical responsibilities, such as early attendance of medical students in basic sciences courses in hospitals, are another important factor in internalizing their medical professional identity. "It feels so good to be in a hospital where you think you’re a doctor where you have to spend your whole life practicing," said participant #7 (female, obstetrics and gynecology resident, third year).
4.3.2. Learnt Competencies of GP
Research findings showed that being a good specialist doctor depends on being a good general practitioner. Participant #7 commented on the general medical skills acquired: "You must study and be diligent from the beginning. It is impossible to say that I did not pass the general course well, but then I kept trying (male, Internal medicine residents, third year).
4.3.3. Beneficial Reforms and Integration in General Medical Education
Assistants in implementing the reform program (reform) in general medicine and familiarizing them with community service and teamwork plans are effective in their efficiency and self-confidence.
Participant No. 7 commented: "I came up with the reform, we saw the general practitioner's patients and stamped the doctors’ to the end.” It boosted our confidence; it was the best way, this system was excellent" (male, internal medicine resident, third year).
4.4. Knowledge and Educational Background
Knowledge and essential background are one of the most important sub-categories in the unique past constructive experiences. How to teach the family and how to teach the school was a sub-class school formed from the statements and gestures of the participants.
4.4.1. The Education Level Among Families
The findings of the study showed that the education provided to the child in the family during childhood, having parents who have a positive role model in the family, and performance promotion on stresses was influential in shaping the assistants’ professional identity.
Participant #19 stated: “I think that family upbringing is fundamental, it seems that people are all under a lot of stress, upbringing by which parents or in which environment? The educational environment to reach that final stage” (female, obstetrics and gynecology resident, first year).
4.4.2. The Education Quality Level Among Schools and Institutes
The study showed that in education children receive at schools and colleges, decision-making and self-confidence, and problem-solving skills are gradually influential in the formation of their professional identity in the future. Participant No. 1 stated: “decision-making and self-confidence and problem-solving skills, in my opinion, should be taught in childhood, and I think it is really effective (female, obstetrics and gynecology resident, third year).
5. Discussion
In this study, we investigated the formation of the professional identity of medical assistants. According to psychologists, how a stimulus is perceived at a given time largely depends on the reaction that the same stimulation could have already produced (9). Previous unique constructive experiences were identified as an important factor in shaping residents' professional identity. Interpersonal communication experiences, independent professional work, general medical education courses, and knowledge and educational background are unique experiences of any assistant involved in professional development and increasing their responsibilities. Contemporary structuralism studies have shown that professional identity formation and dynamic nature can be changed by facing different experiences or environmental changes (10). In a qualitative study in 2019, Kay et al. demonstrated that: (1) transfer to a medical student; (2) clinical experience in previous years; (3) exposure to the medical profession; and (4) availability (exposure) to physicians in clinical practice are experiences that can stimulate identity formation (11). Although the present study was at a postgraduate level, in comparing the study results, it appears that it also deals with academic experiences and previous knowledge that are not dealt with in the study of Kay et al. According to the findings of the current study, acquiring competence during the specialty training period continues to acquire competencies related to the general medicine course.
A specialist doctor cannot have a good performance without the experience of being a good general practitioner and attainment of professional success. In Shiraly et al.'s study (12), it was demonstrated that basic communication skills lead to success in medical practice and can have a significant impact on patient satisfaction, adherence, and outcomes of the interventions.
Although these skills depend on various personal factors, it is demonstrated that with training and experience, communication skills can be boosted (12).
In Park and Hong’s study (“not yet a doctor”), it was demonstrated that although a competitive student culture and an isolated medical community hindered the study subjects from searching for their professional identities, informal learning experiences, including active interaction with patients, senior doctors, and others outside the medical community, assisted them in developing their professional identities (13).
In addition, establishing effective communication with patients is considered one of the main competencies in clinical practice, and using the clinical knowledge of physicians in their daily practice (2). Mastalerz et al., in his study, suggested that medical resident PIF evolved throughout residency and was strongly influenced by inter and intra-professional interactions, even in optimal interprofessional clinical learning environments (14). In this study, exposure to patient was considered as the best experience for many clinical students during their medical studies. For example, after talking to patients, the students felt that they had succeeded, and they increased their self-confidence by informing and reassuring patients and participating in the collective decision-making.
In his study, Sawatsky et al. stated that autonomy and independent practice allowed assistants to feel personally responsible and confident in caring for patients. Independence allowed assistants to engage in "real decision-making" process in patient care. By showing confidence in decision making, assistants gained more independence. Lack of independence led to isolation and lack of authority and responsibility in patient care. Lack of independence led to isolation and lack of authority and responsibility in patient care. Background, behavior, and identity are influential in the formation of professional identity (15). In the present study, one of the important experiences that the participants believed could affect their professional identity was independent work. In his study entitled "Discovering the experiences of assistants during six months of family medical assistantship", Martin et al. demonstrated that assistants learn what it means to perform the role of family medicine. This learning process involves adapting to significant responsibility changes in knowledge, performance management, and relationships, since they have more responsibility for the management outcomes (10). In this study, one of the factors in shaping the professional identity of the assistants was the symbolic events of the general medical course (such as early exposure), which is consistent with the findings of a study by Schei et al. entitled “Resilience: The use of initial clinical contact to influence the formation of professional identity in medical students” which concluded that early clinical encounter with medical students evokes emotional responses that can serve as stimuli for the development of emotional maturity, communication skills, and patient-centered attitudes. Conversely, they can lead to uncertainty and astray the doctors from patients' apparent concerns. These findings highlight the role of structured and monitored educational strategies that can assist students in performing the emotional work necessary to transfer from the identity of the " a person" to the identity of "a physician" (16). In a study entitled Teaching Critical Thinking and Problem-Solving Skills to Health Care Providers, Chacon and Janssen argues that critical thinking skills are essential for growth. They believed that healthcare professionals are not fully trained in these skills, and the material taught "must be learned by the students. “ Instructors provide learning experience through which students can acquire necessary skills and experiences. Mastery of the content should be the responsibility of the students. Students are provided information and assistance, but they themselves are responsible for learning. But this does not mean that trainers are without any responsibilities. Trainers should definitely spend more time planning and preparing. In contrast to the time spent on educational lectures, the students will be the focus of attention. The generated content is learned, and the instructors can easily update their sessions with each assessment (17). The present study is consistent with the finding of Chacon and Janssen’s study in terms of the findings and conclusion. The findings of Kalen et al. entitled "Medical students' professional development experiences over three clinical courses: a prospective study" concluded that even in clinical courses, there should be different areas of professional competence in the incorporated program and definition of lesson and relate these skills to actual learning activities (18). In the present study, applying the reform program (reform) in the general medical curriculum and familiarizing the students with community service, self-confidence, and forming their professional identity were demonstrated to be effective.
In conclusion, in this study, it can be concluded that one of the essential elements in the residents’ professional identity formation is experience, practice, and repetition of the treatment plans on many patients with various diseases who are referred to teaching hospitals. Some assistants consider marriage and the experience of living with a partner to be another influential factor in interaction with others and adapting to the workplace. They thought working independently and providing care and treatment services, as well as practicing and experiencing responsibility towards the community after graduation from general medicine to be the institutionalization of professional identity and the practical driving force in shaping their specialized identity. Some assistants saw the Ministry of Health's obligatory service scheme as an opportunity to identify themselves with interest in the field of specialization and the formation of professional identity. One of the first factors influencing the formation of professional identity was holding symbolic events such as the celebration of white robes in general medicine, and students should be exposed to patients in early stages. The assistants found that the implementation of the reform program in general medicine and their familiarity with community service were influential and boosted their self-confidence. The training they received within the family, school, and college in the past was the foundation of their learning today. This is effective in assisting professional development through building new knowledge and skills. Based on the results, if trainees in school strengthen their decision-making and problem-solving skills and boost their self-confidence (cultivating positive personality traits), they have the necessary foundation for the formation of the professional identity of the future as a physician.
5.1. Conclusions
In summary, this study investigated medical residents’ professional identity development through experiences they acquired and internalized in the Tehran University of Medical Sciences medicine school. The study’s findings indicated that medical residents, in their experience, accept difficulties encountered and extend their understanding of professional identity and prepare for becoming a specialist doctor. We found that experiences influence medical residents’ PIF. Study participants named several important occasions that affected their identity formation. Thus we should redesign educational curricula and organizational structures (update knowledge, skills, and attitude) to nurture and support professional identities.
One limitation of this study was that the residents did not have enough time for the interviews, especially the first-year residents, because they were busy with their professional responsibilities or needed to rest. Moreover, there were incidences where the researcher had to stop the interview due to patient overcrowding so that the assistant could participate more fully in the interview. Since most interviews were conducted in hospitals, the interview circumstances were challenging. It was very difficult to arrange interviews with medical education specialists or clinical consultants who were either involved in ministerial meetings or busy training students and assistants. Observation for data collection also had its own environmental problems. Undoubtedly, the researchers endeavored to solve this problem by reviewing notes in the field from the previous interviews and also by remembering most of the categories extracted from the earlier interviews.