1. Background
Workforce planning includes comparing the current workforce to future needs and making plans to acquire this workforce (1, 2). The most obvious way to determine the number of healthcare professionals to support a system or an organization might be to match the healthcare needs of a population (3, 4). Need-based assessment refers to the number of professional staff or the number of services required to provide the best services to maintain the health of the community. Demographic characteristics, including the prevalence of diseases, age, gender, and educational level of the population, are the key elements of this approach (2). Demand is somewhat independent of the need for care. In practice, need and demand are very closely related; however, economically, demand is equal to use (5).
Evidence-based health workforce planning models have been recommended in new approaches (6). In contrast with other scientific fields where a set of well-defined methods are adopted and refined to solve a given problem, in health workforce planning, there are still not commonly accepted or preferred methods to accurately predict the need for physicians (1, 2). Each of these models is designed in specific time and place conditions; therefore, it is not appropriate to use them in societies with different conditions (7). In the methods adopted by each country, there is a wide range of options that have been considered for the accuracy of forecasting in that country (8), such as socioeconomic status (9, 10), education (11, 12), and target population characteristics (13). The aforementioned factors are different in the context of different countries.
About the necessity of workforce management in the field of specialties, workforce planning in specialties is critical because an imbalance in the supply and demand of physicians in a given specialty cannot be compensated by other specialties (14). Modeling of human resources both on the supply side and on the need and demand side should be performed according to the requirements of each country, and there is no integrated and coherent model in the fields of specialties and subspecialties in Iran. Therefore, the researchers decided to carry out the present study in the field of need and demand.
2. Objectives
The present study aimed to design a need adjusted with demand model of the health workforce in the fields of specialties and subspecialties.
3. Methods
Walker and Avant’s synthesis theory was used for designing the model. In theory synthesis, a theorist gathers available information about a phenomenon (15). Concepts and statements are organized into a network or a whole, and a theory is formulated. Synthesis can be in the form of language (theory) or graphic (model) (15). Researchers use this method because understanding and performing Walker and Avant’s theory synthesis is easier for beginner researchers, and it is the most suitable method to develop prescriptive theories (15-17). For this purpose, the following steps were taken:
(1) Based on the methodology, the two concepts of “demand” and “need” should be determined as focal concepts based on the opinion of the research team.
(2) In order to determine the factors related to the focal concepts, the results of the previous systematic review conducted by the researchers (18), a supplementary study on other books and articles (19-23), and the regional reports of the World Health Organization (1, 24-26) about health workforce planning and modeling, plus the viewpoints of research teams, were used.
It should be noted that the research team included the two former and current secretaries of the Development Council of the Ministry of Health and Medical Education (MOHME) and the colleagues of this center in estimating the health workforce project, the former head of the Education Development Center of MOHME, and the former research director of the Center for Strategic Research in Medical Education who were also health policymakers. The researchers had a prolonged engagement with the topic of the current study; accordingly, their opinions can be cited.
(3) In the third stage, a model was presented for the integrated representation of the components.
4. Results
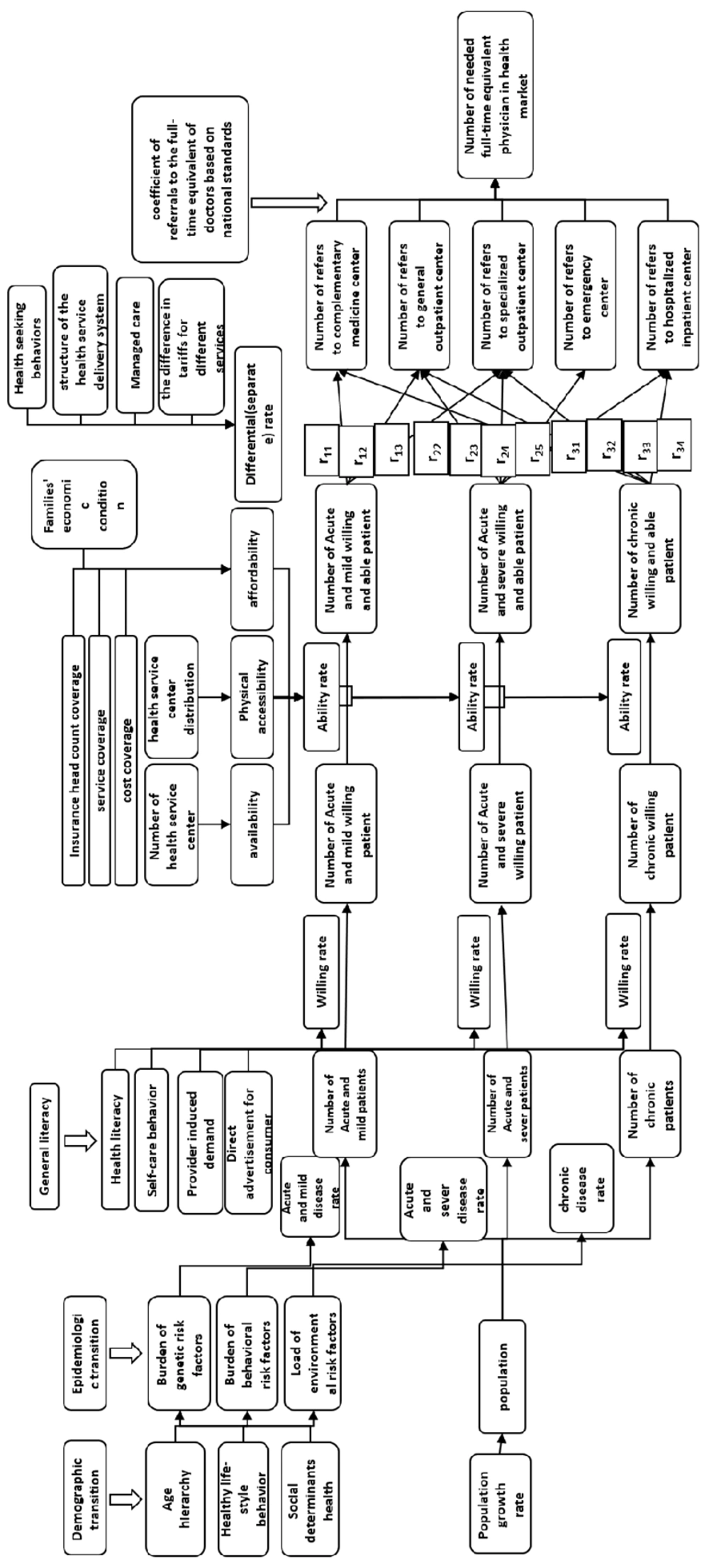
Figure 1 illustrates the model. The basis of this model is a definition of demand in economics, stating that demand is the number of goods or services that a consumer wishes for and can buy in a certain period of time (27). In this model, the types of flows were headcounts. The boxes that were not headcount type were named influential factors (i.e., the factors that affect individuals’ health, needs, and demands), which will exert their influence on the model through rates. These rates either exist or can be estimated.
The first main column in the model is related to population and demographic changes. The second column is related to the population in need of services. In this study, the needs are divided into three categories by the researchers, namely acute and mild, acute and severe, and chronic diseases. Each category has a rate, and by multiplying the rate by the number of the population at any time, the number of individuals who need each category of services will be identified.
According to the definition, acute and mild diseases refer to those conditions that are mostly treated with self-care and mostly require outpatient care services. Acute and severe diseases are those conditions that require prehospital emergency services, hospital emergency, or hospitalization in the emergency department (under observation emergency). Chronic diseases are those conditions for which an individual receives mainly specialized and sometimes general inpatient or outpatient services.
The rates of this part of the model are affected by the demographic and epidemiological transition. Demographic transition is caused by the age pyramid, healthy lifestyle behavior, and social health determinant factors. The epidemiological transition has an effect on genetic, behavioral, and environmental risk factors.
After determining potential needs, for converting to demand according to the definition that it presented at the beginning of the Results section, the next step (i.e., the third column) is to convert the needs into the willingness to receive services by willingness rate; accordingly, there are a number of potential needs, and the individual has a willingness to receive services. The transformation of potential needs into willingness is influenced by general literacy. General literacy results from a number of factors, including health literacy, self-care behavior, health service provider-induced demand, and direct-to-consumer advertising.
After the determination of need and willingness in individuals, the discussion of ability is raised. The rate of ability is influenced by three main components, including availability, physical accessibility, and affordability. Finally, using the ability rate, the number of individuals who need health services and are willing and able to use them will be determined. The number of medical centers is effective in availability. The geographical distribution of medical centers has an effect on physical access. Moreover, some factors, such as the type of insurance coverage and the economic status of families, have an effect on affordability. The economic status of families is a function of gross domestic product, economic growth or recession, and inflation or other factors that are introduced under this general term and affect affordability.
In the next step, it is important at what rate and what type of specialist an individual who has a need is willing and able to refer. Acute and mild patients who are willing and able to refer to health service centers might refer to complementary, alternative, and traditional medicine centers or refer to general or specialized outpatient service centers with separate rates. Acute and severe patients willing and able to refer to health service centers might refer to general or specialized outpatient service centers and emergency or inpatient service centers with separate rates. Chronic patients willing and able to refer to health service centers might refer to complementary, alternative, and traditional medicine centers, general or specialized outpatient service centers, or inpatient service centers with separate rates.
The rates determine the number of individuals who need, wish for, and are able to use health services according to the number of individuals referring to each type of service. Numerous factors affect the rates of this part, including health-seeking behaviors, the structure of the health service delivery system, managed care, and differences in tariffs for services.
Since, in the end, the final product in the need-adjusted with demand model should be the type of headcount, by using the conversion coefficient of referrals to the full-time equivalents of physicians based on national standards, the number of referrals would be converted to the number of full-time functional equivalents required by physicians in the health market of the country. This coefficient can be the number of patients that a physician visits per day or something similar based on national standards or the opinion of experts.
5. Discussion
The model presented in this study is a model for estimating the need adjusted by the demand of the health workforce and the effective factors in this regard, which is designed to be used in dynamic system modeling. Several factors have a dominant effect on the supply and demand of human resources (28). As many of the aforementioned factors as possible should be included to have a comprehensive conceptual approach. A literature review provided a large number of these factors. Considering the complex interactions between variables affecting the supply and demand of human resources is another important feature. For example, population size, average income and level of education, insurance coverage, incidence of diseases, and rate of service utilization are among the factors affecting the demand for health manpower (29). This principle has been observed in the current study.
Considering the population and its changes (30-34), dividing disease into categories (33), demographic (35) and epidemiologic changes (36-38), insurance status (14, 39, 40), economic condition (30, 41-43), health literacy (39, 44), general health (44), and service accessibility (39) are in line with the results of other studies or recommended by them. Using full-time equivalent factor, number (33) and average time (33, 45) of visits, or number of services (32, 34, 45) are in line with the results of other studies, and the present study used them to calculate the number of referrals and conversion coefficient of referrals to the full-time equivalent of physicians.
The relationships between the components of the model were determined with the demand definition (27) and the existing logical relationships between them from the viewpoints of the research team. In the need-adjusted with demand model, initially, the needs are considered in each category of disease and were converted into need-adjusted demands according to some factors, such as willingness and ability (27).
There are a very limited number of need-based models in health workforce planning (38). Most of the models focus on demand; nevertheless, in the need-adjusted demand model presented in this study, the needs are considered, and this issue is an innovative aspect of this model. The researchers did not identify any health workforce planning model that addresses the needs in Iran.
In the need-adjusted demand model, it is attempted to take into account all the effective factors, including the change in epidemiological and demographic conditions, general literacy, economic conditions, and insurance, which have been mentioned in similar studies. In addition to the items mentioned in previous studies, the innovation of this model is that some factors, such as the willingness and ability of individuals to use services, the number of health service centers and their accessibility, the structure of health service provision, behaviors of seeking services, and managed care, are included.
All the effective factors have an effect on the model’s calculations through their impact on the rates. During application, it should be noted that for the rates specified in this model, if there is a real number in national or regional datasets, that number should be placed, or interchangeably the results of studies in other countries, especially comparable countries, can be taken into account; otherwise, if no rate is available, the opinions of the expert panel can be used for estimation.
One of the limitations of this model is that referral levels are not taken into account because these levels do not exist officially and legally in Iran’s healthcare system. It should be noted that while using this model in other fields with reference levels, the model should be adjusted according to this issue.
5.1. Conclusions
This study presented a model for needs adjusted with demands. It has been attempted to consider all the factors affecting the needs and demands that are effective in the current and future conditions of the country. Designing complex and integrated models that take into account more factors provide a better perspective for the sustainability of the health system. The model can provide a suitable tool for stakeholders and decision-makers to estimate the needs and demands of the health workforce in the fields of specialties and subspecialties or with a slight adjustment in the field of clinicians. It is suggested to implement the current model in a system dynamic modeling in future studies.