1. Context
The family physician program (FPP) in Iran was implemented in rural areas in 2005, employing general medical school graduates. It was expanded in 2011 to include all communities with a population of up to 20 000, and a pilot implementation included cities with populations between 20 000 and 50 000 in 3 provinces (1).
As the first point of contact for patients, family physicians must be proficient in (1) interpersonal communication, (2) screening, diagnosis, and treatment of diseases, and (3) assessment of psychological, economic, and social determinants of health, and chronic disease management (4). Leading the health care team, they also need good management skills (2). Therefore, the educational system of FPs should properly address the required competencies of FPs.
There are different methods for training and education of FPs in different countries. The family physician education in the USA begins during medical school, continues during residency, and finishes by getting a physician career. In medical school, students have a 2-step exam, and after acceptance, their education starts with the family physician part. In Singapore, volunteers for family physician education have 2 ways. The first way is to study Master of Medicine (Family Medicine) or choose private practitioners’ stream. Egypt’s rule for family physicians does not need additional education; the only thing required is to stay in Family Medicine for 3 years (5).
Quality education plays an important role in the performance of family physicians. However, the hasty implementation of FPP did not allow adequate time to develop a job description for each member of the health team, clinical guidelines, or educational content. Maftoon et al. reported that nearly 15% of family physicians received no training beyond medical school, and the others completed only simple in-service training (2). At the time of his study, no graduate medical education (residency) was available in Iran for the specialty of family medicine. This contributed to the inconsistency of the educational programs at medical universities, and the training needs of FPP were not met (4).
Training for FPP has been enhanced through the years by adding features such as Master of Public Health (MPH) degree programs or modular training courses for general practitioners (GPs). The Ministry of Health and Medical Education (MHME) introduced residency programs to train GPs as family physician specialists. While this program was successful at equipping GPs to provide FPP services, it had many disadvantages, including prolonged educational time, high financial costs, and a lack of acceptance by the rest of the graduate medical education community and practicing non-specialist GPs (5).
2. Objectives
To achieve the goals of FPP, it is essential to develop a training program that takes into account both the needs of the physicians and the challenges encountered during the FPP implementation. To improve the quality of care provided by FPs, overcome challenges associated with providing an effective gatekeeper for increasing the efficacy of the health care system, aid in planning the next phase of the training for family physicians, and ensure the future effectiveness of FPP, this systematic review of the literature was conducted to comprehensively identify and collate the challenges associated with the education of family physicians in Iran.
3. Evidence Acquisition
All published articles and official reports related to FPP in Iran were the subjects of this study. The inclusion criteria included original articles and official reports published in English or Persian between 2011 and 2021 (since its expansion to some urban areas) related to challenges associated with the education/training of FPs in Iran. Exclusion criteria were gray and unpublished literature, systematic review, and studies published in languages other than English or Persian.
4. Data Sources
In January 2022, credible international scholarly databases (Google Scholar, Scopus, and PubMed) and Persian databases [Iran Medex, Magiran, Irandoc, and Scientific Information for Database (SID)] were searched. The references of the selected articles were hand-searched to find relevant studies.
4.1. Search Strategy
The search strategy was defined based on the search syntax and keywords, which was first defined for the PubMed database and then revised according to each databases’ specific framework of search method.
The following keywords were used in both English and Persian: “Family physician,” “Family Physician Care Program,” “general practice,” “General Medicine,” “General Practitioner,” “General physician,” “education,” “training,” “retraining,” “in-service training,” “skill,” “attitude,” “health-oriented,” “preventative approach,” and “Iran.” Searches employed terms individually and in combinations using Boolean operators AND and OR.
5. Study Selection
First, based on the title and abstract of the articles, 2 reviewers independently selected articles that met the inclusion criteria. Also, the selected abstracts were rechecked for the accessibility of their full texts. Studies were classified into 3 categories: “excluded,” “included,” or “probable.” The full text of the articles categorized as “probable” were reviewed, and the paper was re-categorized as “included” or “excluded.” Where both reviewers agreed, the article was excluded or included, respectively. Papers upon which the reviewers did not agree were included or excluded based on the vote of a third reviewer.
6. Data Extraction
All selected articles were carefully studied, and the following data were extracted. As the type of the systematic review was a qualitative systematic review, data extraction was based on the SPIDER (sample, phenomenon of interest, design, evaluation, research type) technique, which describes the situation. These data include title, authors, year of publication, name of the journal, study design, participants, instruments, settings, variables, strengths, and weaknesses.
6.1. Data Items
The challenges related to the education of family physicians in Iran were the data item in this study.
6.2. Study Risk of Bias Assessment
As noted above, 2 independent reviewers conducted the eligibility, quality assessment, and data extraction stages of the systematic review and sought the opinion of a third reviewer in case of a difference of opinion. Subsequently, a methodologist checked the validity of “included” studies based on the international reporting guidelines, such as COREQ (consolidated criteria for reporting qualitative studies), case reports (care) guideline, PRISMA (preferred reporting items for systematic reviews and meta-analyses), STROBE (strengthening the reporting of observational studies in epidemiology). Articles with low validity were excluded.
7. Results
7.1. Study Selection
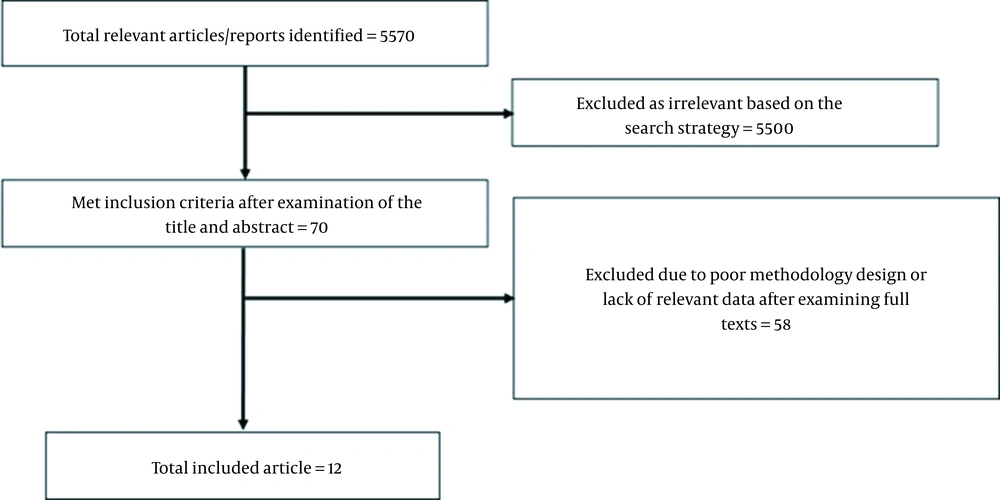
A total of 5570 potentially relevant articles and reports were identified by the search strategy; after examining their title and abstract, 70 studies met the inclusion criteria. Following the full-text review, 58 studies were excluded due to either poor methodology design or irrelevant data. Eleven empirical studies and 1 report were included in the present review (Figure 1).
7.2. Study Characteristics
Table 1 shows the general characteristics of included studies. Nine of the studies and a report used qualitative methods; data were collected by interviews and focus group discussion, and 1 study used document analysis. Two studies applied cross-sectional methods employing questionnaires for data collection.
| Authors | Publication Year | Study Design | Data Collection | Participants | Sample Size | Location | Urban/Rural Family Physician |
|---|---|---|---|---|---|---|---|
| Delavari et al. (6) | 2016 | Qualitative study | Interview | Experts from the health system, GPs currently or previously working in rural areas | 28 | Rural areas in Iran | Rural |
| Jabbari et al. (7) | 2019 | Qualitative study | Focus group | Family physicians, key organizing palliative/end-of-life care stakeholders | 2 focus groups (36) | Tabriz | Rural |
| Mehrolhassani et al. (8) | 2021 | Qualitative study | Interview | Policy-makers and managers at national and provincial levels | 44 | Kerman Province | Urban |
| Dehnavieh et al. (9) | 2015 | Qualitative study | Interview | Informed individuals from medical universities, health insurance, health system, social physicians, researchers in the field of family medicine | 21 | Cities in Kerman Province | Urban |
| Gharibi and Dadgar (10) | 2020 | Qualitative study | Interview | key informant of FPP | 32 | Tabriz University of Medical Sciences | Urban/rural |
| Farzadfar et al. (11) | 2018 | Qualitative study | Interview and focus group | Family physicians, midwives, managers, health insurance managers, service recipients | 37 interviews and 21 focus groups | Kordestan, Alborz, and West Azarbaijan provinces | Urban |
| Alaie et al. (12) | 2020 | Qualitative study | Interview | Policy-makers and informants | 26 | Iran | Urban/rural |
| Mohammadi Bolbanabad et al. (13) | 2019 | Qualitative study | Interview and focus group | Managers, experts, family physicians, specialists, midwives, health insurance experts, service recipients, and behvarz | 30 interviews and 5 focus groups (36) | Kordestan province | Rural |
| Shiyani et al. (14) | 2016 | Qualitative study | Interview and document analysis | Policy-makers, managers of medical universities, key informants | 26 | Iran | Urban |
| Omid et al. (15) | 2014 | Cross-sectional descriptive study | Questionnaire | GPs who volunteered for the FPP | 507 | Isfahan University of Medical Sciences | Urban |
| Kabir et al. (16) | 2018 | Cross-sectional study | Questionnaire | Urban family physicians and health workers | 464 | Cities in Fars and Mazandaran provinces | Urban |
Abbreviations: GPs, general practitioners; FPP, family physician program.
a Report.
A total of 244 interviews and 28 focus group discussions were conducted in qualitative studies, and 971 participants completed the questionnaires. The participants included physicians in FPP, community medicine specialists and other medical specialists, current or former GPs experienced in rural areas, community health workers (behvarz), midwives, palliative and end-of-life care stakeholders, government policy-makers and managers, representatives of medical universities and the medical system, researchers in the field of family medicine, health insurance managers, and health service recipients.
Six out of 9 studies investigated the urban FPP, 3 studies investigated the rural FPP, and 2 studies and a report investigated both. The main findings of the included studies are shown in Table 2.
| Authors | Challenges Associated with the Education and Training of Family Physicians |
|---|---|
| Delavari et al. (6) | Educational priorities: (1) GPs’ therapeutic role is emphasized, neglecting their health promotion role during training; (2) The entrance exam for higher education focuses on complex diseases instead of rural and health promotion topics; (3) Medical students face only complex patients in the hospitals during the internship; and (4) Medical students work on secondary or tertiary care patients––not outpatients––in their internship. Missing or inadequate experiences: (1) No contact with rural patients during medical school or internship; medical students are not experienced working with rural patients and their specific needs; (2) Urban students lack the required communication and cultural skills to interact with rural populations; (3) Misconception about working in rural underserved areas; (4) Most instructors have not worked in rural settings; (5) The rural internship does not prepare GPs for rural practice; and (6) Lack of familiarity by graduated GPs with FPP. Missing components of training: (1) Lack of education on common diseases in rural settings; (2) Lack of patient management skill training; (3) Lack of education on health indicators; (4) Lack of training in management skills; (5) Lack of training in conducting meetings; (6) Lack of training in coordination skills; (7) Lack of training in resource management skills; (8) Lack of training in advocacy skills; (9) Lack of training in proper communication skills; (10) Lack of education on types of patients in rural areas; (11) Lack of training in required work ethics in deprived settings; and (12) Lack of training in medical ethics. |
| Jabbari et al. (7) | (1) No education regarding organizing palliative end-of-life care; and (2) Lack of required communication skill training relevant to palliative/end-of-life care. |
| Mehrolhassani et al. (8) | The medical education system emphasizes a centralized treatment approach like hospital-based training, but education of FPs should have a preventive nature and health-oriented approach. |
| Dehnavieh et al. (9) | Physicians lack the necessary clinical and management skills to participate in FPP. |
| Gharibi and Dadgar (10) | Lack of management skills: (1) Related to leadership; (2) Related to quality improvement; and (3) Related to teamwork. Lack of knowledge and skills related to preventive and social medicine: (1) Medical students neglect public health courses; (2) Lack of in-service training in these fields; (3) Lack of competence regarding disease prevention and health promotion; (4) Physicians’ activities are limited to conventional therapeutic approaches; and (5) Misunderstanding of the nature and activities of this program. |
| Farzadfar et al. (11) | (1) Discordance between GPs training curriculum and the needs of family physicians; (2) Treatment-based and not prevention-based education; and (3) Lack of training for staff before the implementation of FPP. |
| Alaee et al. (12) | (1) Treatment-based education; (2) Physicians’ unfamiliarity with the cultural and social characteristics of the target population; and (3) Lack of required competencies to provide services and perform their duties. |
| Mohammadi Bolbanabad et al. (13) | Discordance between university education and family physician responsibilities, including treatment-oriented education instead of health-oriented education. |
| Shiyani et al. (14) | Malfunctioning health education system: (1) Lack of coordination between physicians’ education, community needs, and existing job opportunities; (2) Treatment-oriented education; and (3) Lack of skills and competencies of family physicians. |
| Omid et al. (15) | The most important educational needs: (1) First aid training and management in emergency conditions such as respiratory emergencies, cardiopulmonary resuscitation, and endotracheal intubation; and (2) Proper emphasis on the management and provision of health services such as methods of contraception, principles and skills of family planning, psychiatric emergencies, patient communication, and health education skills. |
| Kabir et al. (16) | The most important educational needs: (1) Management of cardiovascular diseases, diabetes control and prevention, psychiatric pharmacology, and cardiopulmonary resuscitation; and (2) Proper emphasis on health resource management, communication skills, teamwork skills, meeting skills, and providing health services. |
Abbreviations: GPs, general practitioners; FPP, family physician program.
7.3. Challenges to the Education of Family Physicians
Table 3 summarizes the reported educational challenges encountered by FPP. There were 6 broad themes as described below.
| Theme | Subtheme |
|---|---|
| Challenges of the health education system | Discordance of GP education training curriculum with the needs of family physicians. |
| Treatment-oriented approach. | |
| Neglecting public health courses by medical students. | |
| Lack of training and in-service training for physicians and health team members. | |
| Lack of valid training courses. | |
| Lack of cooperation of family physician specialists in the empowerment of GPs. | |
| Hospital-centered model education. | |
| Not including practical and widely used skills in the training. | |
| Insufficient emphasis on medical ethics. | |
| Not including the skills and knowledge required for working in rural settings in training. | |
| Lack of awareness of GPs regarding FPP | The unfamiliarity of the graduated GPs with FPP. |
| Lack of awareness of family physicians regarding the nature and activities of FPP. | |
| Lack of awareness of family physicians working in the private sector regarding the policies and protocols approved by MHME. | |
| Lack of awareness of GPs about social conditions | The unfamiliarity of physicians with the cultural and social characteristics of the target population. |
| Misconception about working in rural and underserved areas. | |
| Lack of awareness regarding the needs of the community. | |
| Lack of clinical competencies by public health GPs | Lack of practice and knowledge regarding common and outpatient diseases. |
| Lack of patient management skills. | |
| Lack of education for health care providers regarding organizing palliative end-of-life care and how to behave properly with the patients in need of such care. | |
| Lack of skills and knowledge of first aid measures and emergency management. | |
| Lack of knowledge about the types of patients in rural areas. | |
| Lack of health competencies by GPs | Lack of knowledge and skills related to disease prevention and health promotion measures. |
| Lack of knowledge and skills related to social medicine. | |
| Lack of knowledge regarding health indices and indicators. | |
| Lack of social and management competencies by GPs | Lack of communication skills and knowledge. |
| Lack of teamwork skills and knowledge. | |
| Lack of management skills and knowledge. | |
| Lack of leadership skills and knowledge. | |
| Lack of meeting skills. | |
| Lack of coordination skills. | |
| Lack of advocacy skills. | |
| Lack of training skills. |
Abbreviations: GPs, general practitioners; FPP, family physician program; MHME, Ministry of Health and Medical Education.
7.4. Educational System
There was a lack of coordination between the training offered and community needs, FPP physician responsibilities, and existing job opportunities (4, 11, 14).
The treatment-oriented approach in medical schools does not include meaningful training for the individual health-promotion and prevention-oriented approach of FPP. Training in public health was also minimal (6, 8, 10-14). The current hospital-centered model focuses on complicated diseases. Medical students work on patients with complicated diseases in referral hospitals and have limited experience managing illness in the outpatient setting during their internship. The entrance exam for higher education is focused on complicated diseases to the near exclusion of common diseases (6).
A lack of training and in-service training programs for GPs and other health team members was another area identified (4, 10, 11). Incorporation of the residency-trained family physician specialists into the continuing professional development of GPs in FPP never occurred. In addition to a missed opportunity for the education and empowerment of GP, a cohesiveness between the generalists and specialists in family medicine never developed (4).
Studies have reported that family physicians lack the necessary skills and competencies to participate in FPP due to a lack of effective skill-based training (9, 14). Hands-on training in common skills is not often included in the training.
There is a lack of exposure to rural medicine. Medical students do not encounter rural patients during training, and most instructors do not have rural working experience. Studies indicate that rural internship does not prepare GPs for rural practice (6).
A lack of sufficient emphasis on medical ethics was noted. Despite the importance of working in disadvantaged settings in FPP, the ethics of working with underserved populations are neglected (6).
7.5. Awareness of FPP
Another associated challenge was a lack of familiarity of the graduated GPs with the nature, activities, policies, and protocols of FPP (4, 6, 10).
7.6. Knowledge and Awareness of Social Conditions
The educational system does not familiarize graduates with assessing and adapting to the cultural and social characteristics of rural communities and their needs. Misconceptions about working in rural and underserved areas were prevalent (6, 12).
7.7. Clinical Competency
Clinical skills and knowledge in FPs were lacking. This included the areas of common and outpatient diseases, chronic disease management, palliative, and end-of-life care, first aid and emergency management, and the diagnostic approach to the undifferentiated medical patient in rural settings. Specific examples include tracheal intubation, cardiopulmonary resuscitation, care for poisoned patients, chronic cardiovascular diseases care, diabetes management, and psychiatric pharmacology (4, 6, 7, 15, 16).
7.8. Public Health Competency
Knowledge and skills related to disease prevention and health promotion measures, social medicine, and interpreting health indicators were among the identified challenges. This lack of exposure leads to have physicians who do not recognize their needs, such as preventative services, contraception, and family planning skills (4, 10, 15, 16).
7.9. Managerial Skills Competency
Another issue was training in managerial skills such as communication, teamwork, organization and leadership, advocacy, and training others. These abilities are crucial in rural settings (6, 10, 12). FPP physicians ranked management and social skills very low on their priority of educational needs (15, 16).
8. Discussion
Since the initiation of FPP in Iran, many studies and reports (6-16) have provided some lines of evidence that show a variety of challenges in the educational system of FPs in Iran. As this program is going to be expanded across the country, this systematic review of the literature was performed to provide a comprehensive view of the existing challenges associated with the education of family physicians in Iran.
This current review of the literature identified consistent themes associated with the educational system and challenges encountered in preparing physicians for FPP upon graduation.
The focus on curative medicine to the near-exclusion of preventative medicine results in physicians being ill-prepared to function in the role envisioned by FPP (17). A move away from the exclusively hospital-based model to incorporate more outpatient clinical training is a critical step forward for the success of FPP. Many studies related to the education of GPs show that medical schools throughout the world are increasing the time allocated to outpatient clinics (18, 19); however, in Iran, medical training is still hospital-based. Addressing a change from hospital-based medical training to increase outpatient clinical training is not without barriers of its own, including a lack of integration between outpatient and university curricula, limited interaction between decision-makers in the community outpatient clinics and the medical university, and conflicting priorities between medical education and health care delivery (20), which should be addressed for improvement of FPs education/training.
The absence of training courses specific to the duties of physicians in FPP is unfortunate. Kabir et al. proposed changes to the accreditation process for colleges and training centers to ensure that such courses are included as a part of the standard curriculum (17) and policy changes to address the lack of training in practical hands-on skills needed for effective implementation of FPP.
A lack of clinical competencies in the areas of first aid and emergency management is concerning and likely related to the lack of adequate training courses noted above. Changiz et al. showed that physicians in FPP had average skill levels in only 52% of competencies specified for general medicine doctoral graduates (21). GPs also demonstrated inadequate knowledge and skills in social medicine, disease prevention, and health promotion. Other studies have also shown similar results; for instance, Changiz et al. showed that GPs were weak in community health, preventive medicine, occupational health, geriatric medicine, evaluation of malnutrition and growth chart in children, promoting breastfeeding, pregnant mother care, and in data analysis and interpretation of health indicators (21). As many of GPs would serve as FPs at the primary level of health care services, significant curricular improvement is needed throughout the medical education system.
The ability to interact with patients of different social and cultural backgrounds also was underdeveloped. As Wilson et al. pointed out, family physicians should be familiar with the community background, culture, and social environment, especially in rural settings (22). There is limited instruction in cross-cultural communication in Iranian medical school curricula. Training in this area is important and has been demonstrated to be effective when implemented in other countries (23).
Formal training in communication, management, and coordination skills was minimal. In this regard, Shadpour and Malekafzali demonstrated a gap between the training provided in medical universities and the skills needed in daily practice as a family physician (24). Shiraly et al. identified that although most family physicians in Iran had the required knowledge for effective communication with patients, they lacked practical skills. Family physicians working in private sectors had lower practice and communication skills compared to those working in public sectors (25). The reason for these discrepancies is unclear. Manifestations of this deficiency include problems such as ineffective communication and teamwork between nurses and physicians (26). Heidarzadeh et al. identified generalized low-level knowledge and lack of appreciation for the importance of communication skills in Iranian medical educators and emphasized communication skills as a part of medical training (27). Also, Rezaeian et al. showed that communication skills should be incorporated into continuing professional development programs in medical universities (28).
This study showed that physicians in FPP were not well acquainted with the program itself. Other studies also show a similar finding that there is limited knowledge of the origins, intent, structure, priorities, policies, or procedures of FPP (29). For a program like this to succeed, it is important that all participants understand its goals and structure. FPP involves many physicians working in both private and public sectors who are not sufficiently aware of the policies and protocols developed by MHME. Implementing training and in-service training programs to familiarize physicians with these expectations is essential for FFP success. This important factor was unfortunately neglected.
In Iran, the phrase “family physician” refers to both generalist physicians and those who are residency-trained as family physician specialists. Those in the latter group have received formal training in most of the areas of deficiency identified in this review. As FPP is expanded, involving the specialists in the training of generalists will be important, leveraging the family physician specialists’ experience and expertise in the ongoing professional development of the generalists, both young and old, who provide the backbone of FPP. It is vital that they participate in the empowerment of GPs for FPP to realize its full potential.
8.1. Study Limitations
There was no way for the authors to evaluate or justify the credibility of gray literature and unpublished data. Therefore, the current study did not include the gray literature and unpublished data; thus, some information might be missing in this review. However, the provided information is validated by being peer-reviewed or officially published by authentic sources.
9. Conclusions
This review sheds light on the existing challenges of FPP in Iran and provides a basis for improving the educational system of FPP in Iran. These challenges are not insurmountable. Policy-makers, planners, medical universities, and academicians may benefit from the results of this study to improve the quality of education and training of FPs by the coordination between the training modules and community needs, better training of medical students in primary care, rural working experience for GPs, familiarization of the graduated GPs with the nature, activities, policies, and protocols of FPP, familiarization of the preventative services, and familiarization of the managerial skills such as communication, teamwork, organization and leadership, advocacy, and training others for GPs.