1. Background
Informing patients is a crucial aspect of the responsibilities of diagnostic and therapeutic staff, and its necessity in medical imaging centers has been well established for a long time. However, in practice, due to the limited duration of interactions between radiographers and patients, education is often incomplete (1).
Proper patient education can prevent unnecessary repeat exposures, enhance patient cooperation in maintaining correct positions, reduce anxiety, increase satisfaction, and ultimately improve the diagnostic value of medical images (2, 3).
If the importance of patient education in medical imaging is not recognized by the directors of imaging centers and considered a priority, no substantial effort will be made to address the barriers to effective patient education. Thus, the establishment of a clear, universal guideline on patient education in medical imaging is essential (4).
Numerous studies worldwide indicate that the lack of patient education in medical imaging is often due to disagreements and unclear delineation of responsibilities between physicians and radiographers regarding patient education (5). Other studies have revealed that patient education is sometimes neglected, or, when provided, it is incomplete (6). Consequently, researchers emphasize the need to address barriers to patient education more urgently. They recommend creating brochures and instructional materials tailored to each imaging modality, to be made available in imaging clinics (3, 6).
Unfortunately, the critical impact of patient education in medical imaging has not been fully communicated to radiographers. Clear guidelines regarding the timing, location, and responsible personnel for delivering patient education are still lacking. As a result, radiographers may neglect adequate patient education due to the numerous barriers they face (7).
Studies on the significance of patient education have identified several barriers, including insufficient time and staffing in medical imaging, a lack of necessary facilities and resources for patient education, inadequate knowledge and skills among radiographers regarding effective educational methods, and insufficient attention given to the need for patient education by radiographers (8, 9).
2. Objectives
Understanding the barriers to patient education is critical for making informed decisions to improve practices. However, there is limited information available about these barriers in Iranian medical imaging centers. Therefore, this study was conducted in 2021 to determine the obstacles to patient education in medical imaging from the perspective of radiographers.
3. Methods
This study employed a cross-sectional descriptive design and was conducted in 2021 among 548 radiographers in western Iran, focusing on the importance of patient education in medical imaging. Participants were selected through convenience sampling. Of the 548 distributed online survey forms, 499 (91%) were completed fully. The survey was anonymous, and participants provided informed consent before participating in the research.
A researcher-developed online questionnaire was used, with its validity assessed through the content validity method. Feedback from seven academic experts in the relevant field was gathered, and their recommendations were implemented and approved. The reliability of the survey was determined using the test-retest method. Initially, 20 radiographers from the target population completed the survey. After 30 days, the same group filled out the questionnaire again, and the results were analyzed using Cronbach’s alpha test, yielding a reliability coefficient of 78%.
The questionnaire comprised two sections: Demographic information and specific questions on the obstacles to patient education in medical imaging. The demographic section collected data on age, sex, job interest, degree, workplace, work experience, and shift work of radiographers. The second section consisted of seven specific questions addressing barriers to patient education from the radiographers’ perspective, evaluated using a three-option Likert scale.
The completed surveys were analyzed using SPSS software version 22. For quantitative variables, mean and standard deviation were calculated, while qualitative variables were summarized using frequency tables. Parametric tests such as one-sample t-tests and analysis of variance (ANOVA) were used for normally distributed variables, while non-parametric tests such as Mann-Whitney and Kruskal-Wallis tests were applied for non-normal variables.
4. Results
In this study, 548 radiographers were surveyed. Out of the 548 distributed electronic survey forms, 510 (93.1%) radiographers completed the forms fully. Among the participants, 67% were female, 53.6% reported average career interest, 86.4% held a bachelor’s degree, 40.5% had 10 years or more of work experience, 42.9% worked morning shifts, and 51.1% were employed in the radiography unit (Table 1).
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Female | 384 (67) |
| Clinical experience (y) | |
| ≤ 5 | 247 (45) |
| Between 5 and 10 | 79 (14.5) |
| ≥ 10 | 222 (40.5) |
| Job interest | |
| Much | 190 (34.6) |
| Medium | 294 (53.6) |
| Low | 64 (11.8) |
| Degree of education | |
| Technician | 28 (5.1) |
| Bachelor of science | 473 (86.4) |
| Master of science | 47 (8.5) |
| Shift work | |
| Morning | 235 (42.9) |
| Evening | 147 (26.8) |
| Night | 166 (30.3) |
| Workplace department | |
| Radiography | 280 (51.1) |
| CT scan | 151 (27.5) |
| MRI, angiography, and etc. | 117 (21.4) |
Demographic Characteristics of Radiographers
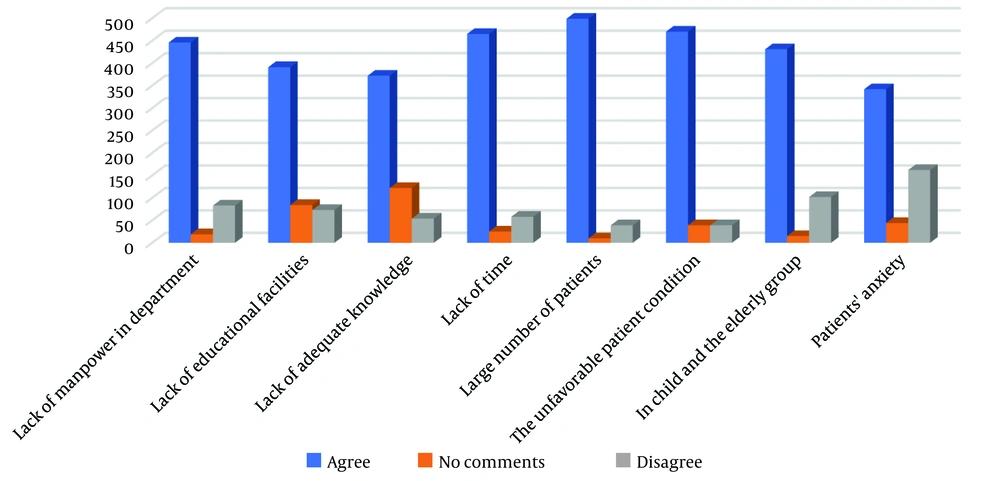
According to the findings, the most significant barriers to informing patients in medical imaging from the perspective of radiographers were identified as follows: A large number of patients (499, 91.1%), unfavorable physical and mental condition of the patients (470, 85.7%), lack of time (465, 84.9%), lack of manpower (446, 81.3%), challenges associated with patient age, particularly in children and the elderly (431, 78.6%), lack of hospital educational facilities (391, 71.4%), lack of knowledge and adequate skills among radiographers regarding effective communication methods (372, 67.9%), and patient anxiety (342, 62.5%) (Figure 1).
5. Discussion
The primary barriers to informing patients in medical imaging, as identified by radiographers in this study, included the large number of patients referred to medical imaging centers, lack of manpower, insufficient time, and the unfavorable physical and mental condition of patients. These were cited as the four main obstacles to providing patient education prior to imaging examinations. Similarly, in the study conducted by Newman, lack of time was highlighted as a significant barrier to patient education (10), a finding consistent with the results of other studies (10-13).
In contrast, Ukkola et al. identified different barriers to patient education in medical imaging, emphasizing the lack of responsibility among radiographers, unawareness of the importance of patient education, and patient anxiety as key challenges (7). Providing adequate education and communication with patients in medical imaging requires significant time and effort, which, in practice, is often constrained by manpower shortages and limited imaging equipment. To prevent overcrowding and reduce patient waiting times for imaging examinations—particularly in trauma centers—radiographers often try to streamline processes, minimizing time spent on patient education.
In this study, radiographers also cited patient age, varying levels of learning ability, and inadequate facilities for patient education as additional barriers. These findings align with the results of studies by Younger et al. and Davidhizar et al., who reported that differences in patients' learning capacities and a lack of imaging equipment were significant obstacles to patient education (9, 14).
However, in the study conducted by Williams et al., patient-related factors, such as age, socioeconomic status, and education level, were identified as the most critical barriers to patient education in radiotherapy settings. Williams et al. recommended strategies to improve patient understanding, such as breaking down examination information into smaller sections, keeping explanations concise and clear, and providing information in the actual sequence of the examination process. These approaches can enhance the comprehension and learning outcomes for patients with limited age or literacy levels (15).
Finally, the lack of knowledge and adequate skills among radiographers and patient anxiety were reported as additional barriers to patient education in this study. These findings are consistent with the results of studies by Newman (10, 14). Insufficient knowledge among radiographers regarding how to educate patients about radiation risks and the correct principles of patient communication has been highlighted in other studies as a significant barrier to effective patient education (16, 17).
Patient anxiety substantially impacts their ability to absorb and retain information. Anxious patients may struggle to recall the information provided or may forget it before the examination. Furthermore, improperly presenting information about radiation risks may inadvertently heighten patient anxiety, potentially causing them to avoid necessary tests.
From the perspective of radiographers in this study, the primary reason for the lack of adequate patient education in medical imaging was the large number of patients referred to imaging centers. This finding suggests an imbalance between the number of imaging centers and the volume of patients, compounded by shortages in equipment and manpower. These issues can lead to a diminished emphasis on patient education by radiographers, resulting in inadequate care services, inefficiencies in the diagnostic process, delayed recovery, exacerbated patient anxiety, increased diagnostic and care costs, and overall dissatisfaction among patients.
Barriers to patient education are the root cause of neglecting its importance by radiographers, ultimately compromising the quality of care provided. This neglect can lead to diagnostic inefficiencies, delayed patient recovery, heightened anxiety, escalated healthcare costs, and reduced patient satisfaction. Addressing these barriers is crucial to improving patient education, ensuring better diagnostic outcomes, and enhancing the overall healthcare experience.
5.1. Study Limitations
The limitations of this study included the lack of enthusiasm among radiographers in completing both the online and offline questionnaires. This may have influenced the response rate and the comprehensiveness of the collected data.
5.2. Conclusions
The absence of specific guidelines related to patient education in medical imaging may contribute to suboptimal performance in this critical area. Therefore, the development of universal guidelines for patient education in medical imaging is both important and necessary.
Addressing the barriers to patient education in medical imaging can be achieved through several measures. These include developing and equipping imaging centers, increasing the workforce by employing more radiographers, and implementing proper planning for patient admission and queuing. In imaging centers with high patient volumes and workloads, providing educational resources such as brochures, posters, or monitors displaying information to patients while they wait for their examinations can enhance the quantity and quality of patient education.
Eliminating barriers to patient education improves the efficiency of medical imaging centers and enhances patient satisfaction. It is therefore recommended that the findings of this study be utilized to address these barriers, improve the quality of hospital services, and guide further research in this field.