1. Background
Graduate-level education in laboratory hematology plays a crucial role in training skilled professionals capable of effectively diagnosing and managing blood disorders. This specialized field requires a well-balanced integration of complex theoretical knowledge with practical laboratory skills, necessitating the implementation of innovative teaching methods to keep pace with the evolving demands of the healthcare sector. In recent years, there has been an increased emphasis on evidence-based teaching methods to improve educational outcomes and ensure that students are well-prepared for real-world clinical applications (1, 2).
One of the fundamental challenges in laboratory hematology education is the inadequacy of educational infrastructure and laboratory facilities. A lack of sufficient investment in modern educational tools, coupled with outdated laboratory setups, restricts access to advanced equipment, real patient samples, and high-fidelity clinical simulations, significantly impacting the quality of training (3). Without proper infrastructure, even the most effective teaching strategies may fail to provide students with adequate hands-on experience. To bridge this gap, educational programs must prioritize upgrading laboratory resources and incorporating technology-enhanced learning environments to enhance students' practical competencies (4).
Beyond infrastructure limitations, a critical issue in this field is the alignment of teaching methods with the real-world practical and clinical needs of students. Teaching approaches are generally categorized into two main types: Instructor-centered and student-centered methods. Traditional instructor-centered approaches, while offering structured content delivery, rely primarily on lectures, content transmission, and exam-based assessments, offering limited opportunities for student engagement (3). While effective for transmitting broad theoretical knowledge, this model does not adequately foster critical thinking, problem-solving abilities, or hands-on laboratory skills (5).
In contrast, student-centered methods focus on active and collaborative learning. These approaches encourage students to engage in problem-based learning (PBL), case studies, and group discussions to analyze complex scientific issues. Research suggests that these methods not only strengthen theoretical understanding but also promote independent thinking and enhance problem-solving skills, clinical decision-making, and practical proficiency (6, 7). In laboratory hematology, students benefit significantly from experiential learning opportunities, such as analyzing real clinical samples, simulating laboratory processes, and developing diagnostic competencies.
Furthermore, laboratory hematology education must address the field’s continuous advancements and emerging technologies. Hematology is a rapidly evolving discipline, with continual progress in diagnostic techniques, treatments, and research methodologies. Therefore, graduate programs must adapt to these changes to ensure that students remain up-to-date with the latest technologies and best practices (8). A significant and ongoing challenge in this regard is the insufficient integration of laboratory-based training with clinical applications (8). Educators must ensure that students not only understand the biochemical and physiological aspects of blood disorders but also develop the skills necessary to interpret laboratory results and make informed clinical decisions (9, 10).
2. Objectives
Given these considerations, this article evaluates and analyzes various teaching methods employed in graduate laboratory hematology programs. Using a qualitative research approach, selective codes were extracted, and feedback from key stakeholders was collected to assess the effectiveness of different pedagogical strategies. By providing comprehensive insights into the most effective and efficient teaching practices in this specialized field, this study aims to contribute to the enhancement of educational methods. The findings can inform the development of more adaptive, student-centered, and clinically relevant curricula, ensuring alignment with the evolving needs of graduate students and future hematology professionals.
3. Methods
Given that the researchers aimed to understand and describe teaching methods in postgraduate laboratory hematology education, the study was conducted in two phases: Qualitative and quantitative, and was descriptive-exploratory in nature.
3.1. Sample Size and Selection Criteria
The sample size for this study followed qualitative research standards, continuing until data saturation was reached, where no new information emerged. A total of 13 hematology and blood bank professors participated in the study. The selection was purposeful, including board-certified hematology professors, three highly experienced faculty members, and newly graduated professors who had recently joined university faculties. This selection aimed to gather diverse perspectives. Efforts were also made to include professors from various universities, such as Shahid Beheshti University of Medical Sciences, Kerman, Mashhad, Tabriz, Shiraz, Sanandaj, and Kermanshah.
3.2. Data Collection
Data were collected through semi-structured individual interviews. The interviews began with a broad question: "In your opinion, what teaching methods should be used at the master's and PhD levels?" Follow-up questions were employed based on participants’ responses to obtain authentic information and a deeper understanding of their experiences regarding the evaluation of teaching methods. The interviews were conducted in locations agreed upon by the professors and averaged 30 minutes in length. All interviews were recorded for subsequent analysis.
3.3. Data Analysis
The analysis process provided the opportunity to conceptualize shared experiences among participants into specific terms. Content analysis was the primary approach for analyzing qualitative data, utilizing a systematic multi-stage coding process. Researchers employed conventional content analysis, one of the common methods for textual data analysis.
(1) Initial coding: The transcribed text was carefully reviewed, and key phrases, patterns, and significant themes related to teaching methodologies were identified.
(2) Axial coding: The initial codes were then compared and categorized into sub-themes based on similarities and relationships. This phase ensured that overlapping concepts were grouped together, refining the structure of data categorization.
(3) Selective coding: The broader sub-themes were synthesized into main categories representing the core findings. During this phase, connections between theoretical approaches, practical training methods, and identified challenges were established to form a comprehensive framework for analysis.
(4) Validation and refinement: To enhance reliability, the coding process was independently reviewed by multiple researchers. Discrepancies in coding were discussed and resolved through consensus, ensuring the accuracy and consistency of categorized themes.
These categorized themes were then analyzed to identify recurring trends and correlations between teaching methodologies and their perceived effectiveness. This iterative approach enabled a detailed understanding of best practices and areas requiring improvement in laboratory hematology education.
3.4. Credibility and Trustworthiness
To ensure the credibility of this study, prolonged engagement with participants and member checks for validating the information were employed. Peer review methods were used to establish trustworthiness. The transcribed and coded text, along with the analysis, was shared with colleagues for feedback and validation.
3.5. Quantitative Section
The quantitative study population included experts, students, and graduates in postgraduate programs. A researcher-designed questionnaire, based on themes extracted from the interviews, was used. A total of 73 out of 100 available participants were selected based on Cochran’s formula.
If 75% or more of the stakeholders rated an indicator as "very important," it was classified as highly important.
If 50 - 74% rated an indicator as "important," it was considered moderately important.
If 25 - 49% rated an indicator as "somewhat important," it was classified as less important. Finally, if less than 24% rated an indicator as "not important," it was considered insignificant.
3.6. Ethical Considerations
The researcher introduced themselves, explained the significance and objectives of the study, and sought permission from the participants for conducting and recording interviews. The interview locations were chosen based on participants’ preferences. Participants were assured of the confidentiality of their information, and numbers were used instead of names to maintain anonymity. They were informed of their right to withdraw from the study at any stage.
4. Results
Fourteen selective codes related to teaching methods in laboratory hematology and transfusion sciences were extracted. Among these, five codes were shared between the master's and Ph.D. programs, while four codes were specific to the master's program and another four to the Ph.D. program (Table 1).
| Teaching methods | Master | Ph.D. | Common |
|---|---|---|---|
| Laboratory teaching | - | - | |
| Practical teaching | - | - | * |
| Virtual teaching | - | - | * |
| Morning reports | - | - | * |
| Journal club | - | - | * |
| Student-centered approach | - | * | - |
| Problem solving and case report | - | * | - |
| Clinical education | - | * | - |
| A combination of instructor-and student-centered approaches | - | * | - |
| Theoretical approach | * | - | - |
| Strong lectures | * | - | - |
| Instructor-centered approach | * | - | - |
a The signifies the application of the teaching method to it.
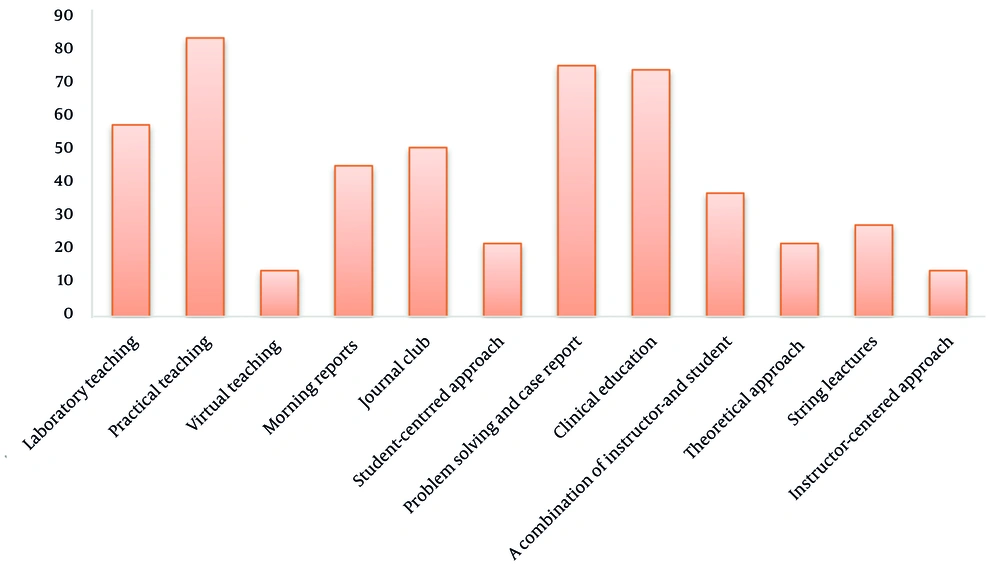
As shown in Figure 1, practical teaching methods (applied in both master's and Ph.D. programs) accounted for 83.6%, while problem-solving, case presentations, and clinical teaching methods (in the Ph.D. program) accounted for 75.3% and 74%, respectively, making them the most significant indicators. On the other hand, virtual teaching and teacher-centered approaches were the least significant, with a rate of 13.7% (Figure 1).
5. Discussion
Effective education in laboratory fields such as hematology and transfusion sciences is a necessity. While no precise historical documentation exists regarding the evolution of effective teaching methods, it is plausible that suitable techniques emerged alongside the concept of learning itself (11). Experts widely agree that no single teaching method can comprehensively address all educational needs; instead, a combination of methods often serves as the optimal approach. To enhance the effectiveness of laboratory education, structured integration of theoretical and practical components is essential. Studies indicate that well-designed teaching strategies directly impact students' ability to analyze laboratory results, make informed clinical decisions, and develop problem-solving skills, which are crucial in hematology-related professions (12).
Historically, teaching relied heavily on lectures and teacher-centered approaches. However, modern education has shifted towards deeper, more practical learning, especially in laboratory-based courses. Blended learning, which combines in-person instruction with online resources, has gained increasing recognition for its ability to reinforce laboratory skills while offering flexibility to students. For instance, virtual simulations can complement hands-on training by allowing students to practice diagnostic techniques in a controlled, risk-free environment before applying them in real laboratory settings. Similarly, online case-based discussions and interactive modules can enhance critical thinking and decision-making in hematology (13, 14).
Despite these advantages, the implementation of blended learning in laboratory education requires careful curriculum design, investment in digital infrastructure, and adequate faculty training to ensure effective integration with hands-on experiences (15). This study revealed that practical teaching methods were highly valued in both master's and Ph.D. programs, while problem-solving and clinical approaches were particularly significant in the Ph.D. curriculum. Clinical education, which immerses students in real-world diagnostic and treatment scenarios, has been shown to significantly enhance their ability to interpret laboratory data and apply theoretical concepts effectively. However, the findings suggest that current clinical training opportunities in hematology are still limited, highlighting the need for increased collaboration between academic institutions and healthcare facilities.
5.1. Limitations and Future Research Directions
While this study provides valuable insights into effective teaching methods in laboratory hematology, it does not fully explore the influence of cultural and institutional differences on educational outcomes. The effectiveness of online and blended learning strategies may vary across different regions due to disparities in technological access, faculty expertise, and student engagement with digital tools (14). Future research should examine how these factors influence learning outcomes and determine best practices for adapting modern teaching methods in diverse educational settings.
Additionally, this research primarily focused on students' and educators' perspectives on existing teaching strategies. Further investigations could assess long-term outcomes by tracking graduates' professional competencies and their ability to apply acquired knowledge in clinical and laboratory environments. Evaluating the direct impact of various instructional methods on real-world performance would provide a more comprehensive understanding of their effectiveness (15).
Furthermore, the rapid advancement of artificial intelligence (AI) and automation in laboratory diagnostics presents both opportunities and challenges for hematology education. Future studies should explore how AI-driven diagnostic tools and automated systems can be integrated into the curriculum to better prepare students for emerging trends in laboratory medicine.
5.2. Recommendations for Improving Hematology Education
To further enhance teaching strategies in laboratory hematology, educational institutions should consider the following approaches: Expanding the use of virtual reality (VR) and augmented reality (AR) in laboratory training, enabling students to interact with 3D models of blood samples and hematological disorders before engaging in real laboratory procedures; developing standardized clinical training programs in partnership with hospitals and diagnostic centers, ensuring that students gain exposure to real patient cases and laboratory workflows; enhancing faculty development programs to equip educators with the necessary skills for integrating digital tools, active learning methods, and competency-based assessments into their teaching practices; encouraging interdisciplinary collaboration, integrating knowledge from fields such as bioinformatics, artificial intelligence, and molecular diagnostics to keep pace with advancements in hematology research and practice; establishing continuous assessment and feedback mechanisms, allowing educators to evaluate the effectiveness of various teaching strategies and make data-driven improvements. By implementing these strategies, hematology education can evolve to better prepare future professionals for the complexities of laboratory diagnostics and patient care. The integration of innovative teaching methods, alongside continuous research and curriculum adaptation, will be key to ensuring high-quality education in this dynamic field.