1. Background
Clinical training refers to a process in which students apply their theoretical knowledge in actual situations on real patients under the supervision of an instructor. Any weaknesses in clinical training will lead to inefficient midwives; affecting the maternal and neonatal health services provided and the quality of spontaneous vaginal delivery (SVD) (1).
The mission of midwifery faculties is to train competent midwives to promote SVD, reduce unnecessary cesarean sections and their costs and provide healthcare services for women (2). The clinical skills of midwifery students are tightly linked to the quality of clinical training. The mission of schools of midwifery is to train competent and skilled midwives. Some studies suggest that clinical training does not provide students with the ability required for acquiring clinical skills and competency (3). Given the importance of clinical training and training of midwives capable of accomplishing their duties, reviewing the status of training and its challenges is essential in midwifery students in teaching hospitals (4). Numerous quantitative researches have been done to investigate the perspective of midwifery students on the status of clinical training (5), which can be pointed to: examining clinical training stressors (6), clinical training problems (7), experiences and satisfaction of nursing students with clinical training (8) and perceived feedback in clinical training and support and supervision in clinical learning settings (9).
None of these studies provided a detailed description of the midwifery clinical training process from the standpoint of midwifery instructors and midwifery students. Given the interdependence of learning of teaching in any educational process, efficient learning and training can be ensured by evaluating the effectiveness of this process from the perspective of both the students and the instructors. Given the few studies conducted in this context and the differences in the views of the instructors and students in different universities, the challenges of and the barriers to implementing midwifery clinical training are required to be individually examined in each educational center, and the results to be used to improve the quantitative and qualitative levels of clinical training and strategic planning in the future.
2. Objectives
The present research was conducted to address the challenges of midwifery training from the perspective of the instructors and students.
3. Methods
A multi-center qualitative study was conducted in Hamedan University of Medical Sciences (HUMS), Hamadan, Iran, and Rasht University of Medical Sciences (RUMS), Rasht, Iran. Purposive sampling was used to select the samples and reach theoretical saturation. Ten midwifery instructors and ten undergraduate midwifery students consented to participate in individual interviews.
The present study was approved by the Ethics Committee of HUMS. Before beginning the study, the role and contribution of the authors, the study objectives and the way the data would be used were determined by common consent in the research team. The participants were ensured of their voluntary participation and their right to withdraw at any time point at their own discretion. They were also ensured of the confidentiality of their information. Moreover, the lecturers briefed the participants on the study objectives and benefits. They were then asked to sing informed written consent forms for recording the interviews.
The researcher received the email address and phone number of the participating students and instructors. The participants decided on the time and location of the interviews through the phone calls made by the researchers.
It is worth noting that no one else was involved in this study except for the participants and the researchers.
The following steps were taken to conduct a content analysis:
Step 1: All the interview transcripts were reviewed several times to gain a deeper understanding of the qualitative data.
Step 2: The interview transcripts were split into small meaningful units.
Step 3: Several codes were merged to extract categories from the meaningful units.
Step 4: The categories were reviewed for extracting and labeling the themes (data analysis).
To collect focused qualitative textual data, semi-structured interviews were conducted with 6 of the students and 6 of the instructors, and a focus group meeting of 4 senior midwifery students and 4 instructors was also held. The objective of focus group discussions was to enhance the validity of the study through cross-checking and triangulation of the qualitative data obtained from different sources, and to acknowledge data saturation (10).
An interview guide was developed to ensure the similarity of the data collected by the interviewer from the participants (10). A panel of experts confirmed the content validity of the interview guide. The interviews began with a general question, and they were guided according to the participants’ responses. The instructors’ and students’ perspectives on midwifery trainings in the labor unit constituted the core of the questions. The general open-ended questions first asked included “what do you do during the day when you go to the labor unit?”. Depending on the responses of the participants and the way the conversation proceeded, proper follow-up questions, including open-ended and direct or indirect questions, were used such as “please explain your educational problems”, “could you please elaborate on this point?” or “what are your suggestions for solving the problems you mentioned?”. The individual interviews lasted 45 - 90 minutes.
In the focus group, the participants were encouraged to discuss with one another, ask questions and exchange their views about the study subject. The focus group discussion lasted 75 - 85 minutes. Notes were also made during the interviews and focus group discussions. The interviews, focus group discussions and the extracted codes were stored in Max QD. Furthermore, each participant was identified with a participant number.
The present study data were back-translated into English. The four steps mentioned above were then taken manually. Before performing content analysis on the data, all the participants confirmed the interview transcripts.
4. Results
The mean age of the study instructors was 35.12 ± 9.62 years, and that of the students 21.24 ± 8.54. Some of the main characteristics of the participants are presented (Table 1). The interviewer was a faculty member of the School of Nursing and Midwifery at the time of the study. The researchers and all of the participants were female, and all the researchers had experiences in teaching the participants.
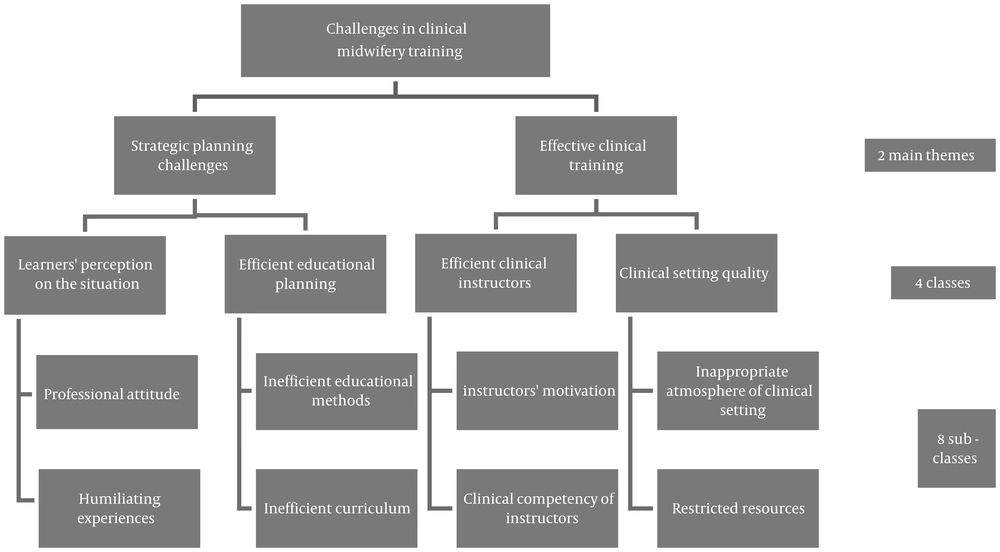
A total of 235 codes were extracted from the data. The two main themes, four categories and eight subcategories obtained after merging the similar codes were associated with the interviews on midwifery clinical training challenges and solutions (Figure 1).
4.1. Instructors’ Motivation
Based on the participants’ perspective, the occupational motivation of the instructors as well as factors such as lack of independence in the field of midwifery duties, not paying attention to the midwifery instructor’s wage system and a lack of legitimate support for the instructors were challenges of midwifery clinical training.
“The views of the instructors in the labor units are not taken into consideration. While midwifery instructors have adequate skills in SVD, they do not have the right to independently express their ideas and views in cases of low-risk deliveries” (an instructor).
“The midwifery instructors used to receive labor fees from the hospital, which encouraged them; nevertheless, these fees were later eliminated” (an instructor).
4.2. Instructors’ Clinical Competence
Based on the participants’ perspective, the research-oriented performance of the instructors and ineffectiveness of the instructors’ selection and evaluation system were important issues in midwifery clinical training.
“The instructors would certainly focus on their number of papers published in international journals as the current evaluative criterion for the performance of instructors rather than improving the training of the students. Given the ineffectiveness of these papers in improving the quality of our student training, this system should be revised” (an instructor).
“Some universities use instructors with inadequate training skills, and this issue can reduce the quality of midwifery training” (a student).
4.3. Professional Attitude
Some participants believed that the instructors’ professional attitudes and factors such as their lack of interest in their job and willingness to perform tasks unrelated to their job are among the problems exerting indirect negative effects on midwifery.
“When the midwifery instructor is not interested in her job, this attitude is also transferred to the student” (a student).
“Midwifery students are concerned about their future occupation. This problem causes a low interest in midwifery and a tendency to do the tasks defined as physician tasks” (a student).
“The lack of a midwifery position in the clinic has caused the midwifery students to avoid clinics” (an instructor).
4.4. Humiliating Experiences
Some participants believed that humiliating experiences and factors, including undue rigor, aggressive treatment of midwifery students for their mistakes in the presence of the patient or other staff, the instructor’s bad temper and the discriminatory behavior of the staff, negatively affect the students.
“Undue criticism may develop hatred in students for their field of study and the clinical setting” (an instructor).
“Harsh aggressive behaviors of the instructors or physicians negatively affect and annoy me” (a student).
4.5. Restricted Resources
The participants mentioned problems such as limited resources, lack of facilities required for SVD training and violation of patient privacy.
“Although we are expected to teach SVD to the students, we lack the necessary facilities for training” (an instructor).
“Limited hospital facilities have caused the physicians to take turn in using facilities such as the conference hall and the rest room. In the labor unit, we lack a place for presentations or rest, and we have to stand up in this unit for long” (a student).
“The number of patients does not match the number of students, causing the violation of patient privacy by learners and lack of patient cooperation” (an instructor).
4.6. Inappropriate Atmosphere of Clinical Setting
According to the participants, inappropriate atmosphere of the clinical setting and factors such as the staff failure to cooperate and the gap between theory and practice in midwifery make up the challenges of clinical training. There appears a lack of efficient communication between the authorities of the faculty and the hospital authorities.
“Unfortunately, there is yet no common understanding of midwifery clinical training between the faculty members and the hospital authorities” (an instructor).
“The executive routine in the labor unit is different from the theory of some midwifery processes” (a student).
4.7. Inefficient Curriculum
The participants mentioned issues such as the need for reviewing midwifery references and curriculum, changing attitudes in midwifery training and rewriting the curriculum based on the job description of Iranian midwives.
“The available references are entirely medical oriented, whereas they should cover both medicine and midwifery given that midwifery is multi-disciplinary and encompasses care, health, behavior, etc.” (an instructor).
“Determining the objectives of midwifery training is crucial for developing the curriculum and resources based on the needs” (an instructor).
4.8. Inefficient Educational Methods
The other problems mentioned by the participants included inefficient educational methods, using conventional clinical training methods, failing to develop basic skills and a lack of a uniform educational procedure.
“A few professors use modern educational methods such as role play in clinical training” (an instructor).
The conventional type of training is a barrier to developing basic skills involving problem-solving, decision-making and design of a healthcare program in midwifery students. “Clinical instructors pay less attention to reflection, problem solving, critical thinking and giving feedback to the students” (an instructor).
| University | Number of Students Participating in Interviews | Number of Instructors Participating in Interviews | Number of Students Participating in Focus Group Discussions | Number of Instructors Participating in Focus Group Discussions |
|---|---|---|---|---|
| HUMS | S6 = 1, S8 = 2 | 3 | 2 seniors | 2 |
| RUMS | S6 = 1, S8 = 2 | 3 | 2 seniors | 2 |
The Main Characteristics of the Study Subjects Participating in Individual Interviews and Focus Group Discussions
5. Discussion
The present study adopted a qualitative approach to providing a detailed description of the experiences of midwifery instructors and students with clinical training.
Compared to previously-conducted studies in this context, the present study sought more comprehensive results on the challenges of midwifery clinical training. In contrast to literature, the present research integrated the views of the midwifery students and instructors in two universities as the study setting.
Identifying the challenges of midwifery clinical training is the first step towards achieving the educational and training goals of midwives. The present study found the clinical instructors to be efficient in improving midwifery clinical training, as their most important responsibility. The instructors should therefore have or acquire the skills required for responding to the educational needs of the students (8). The lack of adequate skills in the clinical training instructors was found to be a major challenge of clinical training (11).
The instructors’ motivation was mainly affected by professional autonomy in the area of duties and professional support. The autonomy of the midwifery instructors is necessary for developing trust, respect, skill and competency (12). The factors reported to affect professional autonomy include transparency in the definition of the concept of professional autonomy, receiving the support of the managers, the midwifery teamwork based on evidence and regular study and using a comprehensive theory of professional autonomy (13, 14).
Professional attitude was another concept identified in the present study. Having a positive attitude is considered a prerequisite for achieving success in different fields of study. The steps required to be taken to reform the policies and clinical training programs and eliminate or add new fields of study include the recognition of different factors associated with the students’ attitude towards their field of study (15, 16). The authorities in charge of midwifery clinical training are expected to develop strategies to institutionalize beliefs and values in line with the field of study and due expectations, and modify physical clinical conditions to attract students and develop self-esteem, motivation and positive educational attitudes in midwifery students.
Humiliating experiences were another concept identified in this study, as the majority of the participants reported the unfriendly behaviors of the physicians and staff and sometimes of the instructors towards the midwifery students. Unfriendly behaviors included a wide range of verbal abuse, bullying and disrespect, and threatened the students’ health in clinical training settings (17). The clinical setting did not support the students, and was referred to as the phenomenon of “vertical violence against students” (18). Developing a safe setting and friendly behaviors in clinical settings can develop a sense of value in midwifery students and improve teaching and learning conditions.
Limited resources were reported as a challenge of midwifery clinical training. Clinical training settings have always faced with shortcomings. Admitting midwifery students based on the clinical capacity of the university, providing and promoting welfare facilities in line with the educational needs of the departments, and providing facilities for the students are essential for improving the quality of education. Midwifery clinical training requires that facilities and resources be provided, which is consistent with similar studies (19).
Identifying and resolving the shortcomings and deficiencies, and preventing discrimination in the allocation of resources and facilities to medical and non-medical students appear the main mission of academic training systems.
The inappropriate atmosphere of the clinic was reported as a challenge of midwifery training in the present study. The facilitating role of the staff and the physicians’ collaboration with the students was reported in literature to contribute to the efficiency of clinical trainings. Several Iranian researchers reported disrespect in the staff and a lack of coordination between the treatment and educational systems of the university (20). The supportive behavior of the staff can contribute to professional growth and affect the teaching and learning process (21). The supportive behavior of the staff towards midwifery students and the intra-organizational coordination between the faculties and hospitals appear to improve the status of midwifery clinical training (22).
Inefficient curriculum was considered a challenge of midwifery training. Given the extent of midwifery services and developments in the midwifery profession in Iran, paying attention to the efficient training of this profession has turned into a pivotal issue (23). The instructors mentioned the review of the curriculum based on the duties of Iranian midwives. Curriculum in this field of study should be developed in such a way that the objectives expected by the health system are met. Ensuring the quality of midwifery training programs is crucial for the clinical training system. The educational needs of medical students and the professional goals of the training are considered the components of training based on the system needs (24).
The present study reported inefficient educational methods as a challenge of midwifery training. Using efficient teaching methods is crucial for developing the skills required for students. As an objective of clinical training, developing basic skills involving problem-solving and efficient communication improves the quality of clinical training. The instructors’ lack of knowledge on modern teaching methods and the inability of the students to make decisions were reported as the main clinical training problems from the nurses’ perspectives. Using active teaching methods in midwifery training causes a more profound learning, and improves the clinical skills of students. Given the complexity of the midwifery field of study, using modern clinical training methods enhances the level of clinical training.
The present study identified a more comprehensive view of the problems in the instructors, as they emphasized the improvement in their motivation and training on modern teaching methods. In addition, the students emphasized their professional future, professional discrimination and the need for employing experienced instructors.
5.1. Conclusions
The present study identified ineffective educational methods as a challenge of midwifery clinical training. Using efficient teaching methods is crucial for developing the skills required for midwifery students. Failing to pay attention to developing basic skills in midwifery students was another concept reported by the participants. Critical thinking, problem-solving skills and clinical decision-making as well as reasoning and judgment based on documents and evidence are considered the essential parts of midwifery clinical trainings. As the objective of midwifery clinical training, developing basic skills involving problem-solving, efficient communication and critical thinking and actively involving midwifery students can improve the quality of midwifery clinical training. The educational system authorities appear to have failed to pay adequate attention to this dimension of training. Reviewing this area, changing the attitudes of clinical training authorities and holding retraining classes are therefore urgently needed. The instructors’ lack of knowledge on modern teaching methods and the students’ inability to make decisions were reported as the main midwifery clinical training problems from the perspective of the midwives. Using active teaching methods in midwifery clinical training causes a more profound learning and improves critical thinking and clinical skills in the midwifery. Given the complexity of the midwifery field of study, using modern clinical training methods enhances the level of clinical training.