1. Background
Self-directed learning (SDL) is an essential teaching-learning method for transforming medical students into lifelong learners, which enables them to identify their learning needs, allocate resources, formulate learning objectives, and evaluate the learning process throughout their medical career (1). Self-directed learning, as proposed by Knowles, is one of the critical components of adult learning (2). Knowles describes SDL with seven crucial components as a process in which individuals take the initiative, with or without the help of others, in diagnosing their learning needs, formulating goals, identifying human and material resources for learning, choosing and implementing appropriate learning strategies, and evaluating learning outcomes (2). Mezirow have pointed out that "No concept is more central to what adult education is all about than SDL" (3). In SDL, the learner is accountable for his learning process. Learners select the resources and methods of learning with the help of teachers who act as facilitators. Gradually, the learning control shifts from teacher to learner. Self-directed learning is one of the teaching-learning methods used in medical education. Under the new Competency-Based Medical Education (CBME) curriculum, the Medical Council of India (MCI) has recommended SDL as a mandatory method for undergraduate medical students to study all subjects. Out of the total 280 hours of teaching allotted, according to the new CBME curriculum in Biochemistry, 20 hours have been assigned for SDL to deal with the subject in 1st phase of MBBS (4, 5). In SDL, medical students should take the initiative in their learning to deal with an educational challenge and as a promising methodology for lifelong learning in medicine (6). Lifelong learning is a necessity to cope with fast-expanding medical knowledge. Medical institutes worldwide are now emphasizing on adoption of SDL (7, 8). It is an additional benefit for teachers and learners, and helps curriculum makers to choose this method in alignment with some other learning objectives. The conduct of SDL is quite variable in different places as students from different parts of the country differ in their cultural and social backgrounds (5, 8). Hence if students were subjected to didactic lectures alone without active learning, they could lose interest in the early part of graduation. With a large group of students who are slow learners and coupled with limited trained faculty, lecture-based teachings are often considered less productive. Moreover, many apprehensions exist among medical faculty regarding "when" the SDL should be implemented? For "which" topic it should be implemented? And "how" it should be implemented? Therefore, further clarification of the concept, conduct, and placement in the new curriculum can play a vital role in the acceptability and implementation of SDL (9, 10). First-year MBBS students mostly need training and support to become self-directed learners. This support is necessary as the students are not ready at the beginning of the undergraduate medical course for self-directed learning and usually depend on the teacher until they pass through different phases of MBBS (11). A study by Frambach et al. investigating students from three medical schools has suggested that students from different cultures are progressively accustomed to the principle of SDL from year to year (12). Specific modules in the curriculum play significant roles in promoting SDL in the early phase of medical studies. Kidane et al. have emphasized that Problem based learning, tutorial discussion, and tutors have strong influences on self-directed learning (13). In contrast, other curricular components, such as lectures and assessments, negatively influence students’ SDL (13).
2. Objectives
Given the above background, the present study aimed to evaluate the outcome of adopting SDL for first-year MBBS students in biochemistry along with supplementing SDL with a lecture.
3. Methods
This cohort study was undertaken to investigate the volunteer first-year MBBS students from Department of Biochemistry in October, 2021 in a tertiary care hospital in South India. It was designed to be conducted in two sessions. Of 177 first-year MBBS students, 158 students responding to questionnaires and attending both sessions were included in the study. First-year MBBS students who were absent for even one session were excluded from the study. Written informed consent was obtained from all volunteered participants. The study was conducted after obtaining approval from the institutional ethics committee.
In session one, Lecture cum SDL was implemented, whereas in session two, only SDL was employed. Pre-test and post-test were conducted before and after the completion of both sessions. Pre- and post-test answer sheets were evaluated, and students’ perception forms were analyzed based on a 5-point Likert scale.
Step 1: Potential, team-based SDL topics for sessions one and two were selected based on the new curriculum of biochemistry. Pre-test and post-test questionnaires consisting of five 1-point, multiple-choice questions relating to the topic for sessions were prepared.
Step 2: Session one was started by the facilitator giving a 1-hour lecture on the topic selected for that session. After the lecture, the students were sensitized about the SDL method and were given five days to assess and fill the gaps in their knowledge of the discussed topic on their own. A pre-test was conducted after the completion of the lecture. Total students were divided into groups, and a leader was selected for each group on a volunteer basis. Facilitators were in continuous communication with students to guide and help them find resources like textbooks, related videos, scholarly articles, etc. To this end, students were encouraged to utilize the central library. Group leaders communicated with their respective groups for the given five days and shared the information with their team members. After five days, students were asked to present the topic allotted to their group to other groups, and each group was given 10 minutes for their presentations. Students were encouraged to submit their topics as PowerPoint presentations, Flip charts, Skits, and debates. The facilitator ensured that all the students in each group were involved by contributing to the presentation. After completing their presentations, facilitators gave feedback about their learning outcomes based on the quality of their explanations about knowledge gaps and the reliability of the sources from which they had collected the information. A post-test was performed after the completion of the session.
Step 3: Session two SDL was implemented in the same way as session one, except that the lecture before SDL was omitted. A pre-test was completed before the session, and a post-test was conducted after the session on the allotted topic.
Step 4: After completion of the sessions one and two, all participants were asked to fill out the perception and feedback form about the SDL sessions. The given form consisted of 10 close-ended questions about workload, team effort, acquisition of new knowledge, etc. The forms inquiring about students’ perceptions of SDL were prepared based on a 5-point Likert scale rating from 5-strongly agree to 1-strongly disagree. Students were also requested to reflect on how this session affected their perception of SDL, and their opinions were sought by asking a few open-ended questions.
Step 5: Both pre- and post-test answer sheets were evaluated without giving any negative marks, and students’ perception forms were analyzed and entered into excel sheets.
Statistical Analysis: The obtained data were expressed as mean ± standard deviation. Statistical analysis of pre-test and post-test data from each session was performed using paired t-test. The differences among post-test scores from both sessions were compared using an unpaired t-test. A two-tailed P-value of < 0.05 was considered statistically significant. Students’ perception form, prepared based on a 5-point Likert scale, about SDL was analysed in percentage terms of agreement or disagreement on the statement. All statistical analyses were performed using Microsoft Excel spreadsheets and the Statistical Package for social sciences for Windows 25.0 (SPSS Inc., Chicago, IL, USA).
4. Results
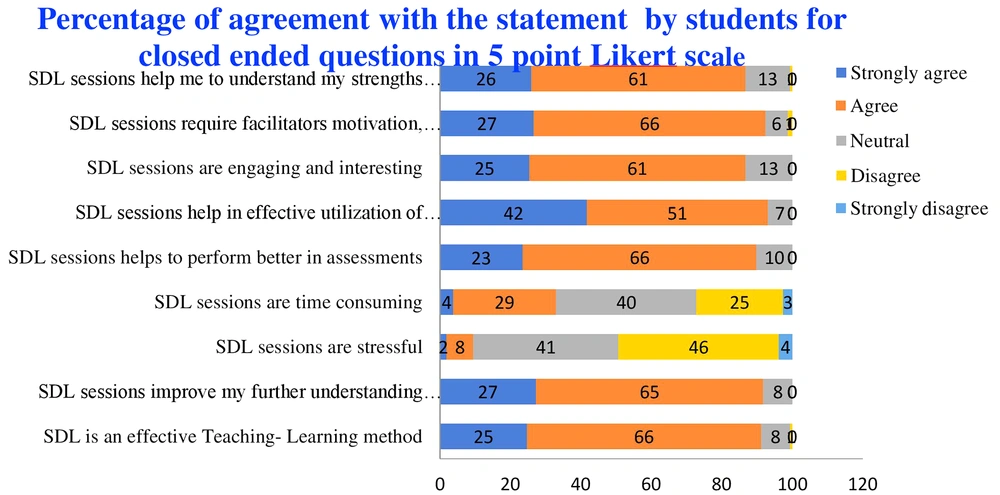
The scores obtained in both sessions’ pre- and post-test were compared. A statistically significant increase was observed in the mean scores obtained for post-test of both sessions compared to pre-test scores (Table 1). A statistically significant increase was also detected in post-test scores of session one compared to post-test scores of session two (Table 2). The response rate of student’s perception and feedback obtained from survey forms was 100%. Students’ perception form evaluating SDL based on a 5-point Likert scale was analyzed in percentage terms of agreement or disagreement on the statement (Figure 1). In total, 93% of students believed that facilitator’s guidance played a significant role and that SDL helped them utilize the available resources effectively.
Abbreviation: SDL, self-directed learning.
a Significant at the 0.05 probability level.
| Score | Lecture and SDL (n = 158) | SDL (n = 158) | P-Value |
|---|---|---|---|
| Post test score | 3.78 ± 0.72 | 3.28 ± 0.85 | < 0.001 a |
Abbreviation: SDL, self-directed learning.
a Significant at the 0.05 probability level.
Moreover, 92% of students were of the same opinion that SDL facilitated further understanding of a topic, 87% of them agreed that SDL sessions helped them identify their strengths/weaknesses, and 86% of them believed that these sessions were engaging and interesting. However, 33% of students partially agreed that SDL was time-consuming, and 10% believed that SDL was stressful. Students’ feedback was collected by posing a few open-ended questions and recording their responses to the questions (Table 3). Majority of the students argued that self-directed learning motivated them and gave them a sense of responsibility for their studies.
| Set of Questionnaires to Assess Self-directed Learning Activity | The Students Response |
|---|---|
| What is your motivation for self-directed learning? | To understand and communicate more effectively. Exploring the knowledge about the subject. |
| What are the difficulties you face when adopting self-directed learning? | Time management and some topics are difficult to self-understand. Finding information through resources. |
| Did you attend self-directed learning sessions at school? | Majority No: we didn’t attend self-directed learning sessions at school. |
| Did attending self-directed learning session help you achieve more favourable learning outcomes? | Majority yes. |
| How can a facilitator help you with self-directed learning? | By giving clear instructions on how to read, giving guidance on necessary information, and introducing appropriate resources. |
5. Discussion
Self-directed learning has been recognized as a promising methodology for lifelong learning in medicine. In the present study, the mean scores of the post-test for both sessions (P < 0.001) were significantly higher than those of the pre-test, suggesting that SDL was an effective teaching/learning method. Comparing the mean post-test scores obtained in both sessions revealed a statistically significant increase (P < 0.001) in Lecture cum SDL session scores in comparison with scores from SDL session alone, indicating that SDL supplemented with an introductory lecture produced more favorable outcomes. Other previous studies had reported similar findings (11, 12), suggesting that a hybrid teaching module was capable of enhancing students’ performance (14, 15). Training first-year MBBS students to become successful self-directed learners as well as providing them with support from faculty, are essential. This support, in particular, is necessary because the students are not familiar with self-directed learning at the beginning of the undergraduate medical course and largely depend on their teachers until they pass through different phases of MBBS (15). However, further studies on different stages of MBBS should be conducted across the country in order to corroborate this assumption. Lee et al. examined the relationship between curricular elements and SDL, and demonstrated that the lectures correlated with SDL positively regarding six curricular components (16). They also discovered that tutorial discussion and unit/case objectives correlated with SDL weakly (16). Furthermore, Shokar et al. determined that self-directed learning improved students’ performance (17). In a systematic final analysis review which included 59 studies exploring 8011 learners and 25 studies (42%), Murad et al. reported that SDL was moderately associated with the knowledge domain and that SDL was more suitable for adult learners who had already had background knowledge and put their learning immediately into practice (18). Therefore, they recommend that SDL should be adopted as an effective strategy for medical students in their later years of medical school or residency and internship (18). Furthermore, the feedback from students revealed that majority of them had a positive attitude toward this strategy. Taking into account the results from the present study, it was emphasized that adopting a sensible combination of didactic lectures and self-directed learning may have been more effective than implementing either method alone. These findings were in line with the results from a few other studies (19, 20). A study by Pai et al. carried out in India found no influence of didactic lecture on SDL (10). They attributed this finding to a heterogeneous mix of students with different learning abilities and variations in the learning environment (10). In our study, however, the effect of SDL on students with different learning abilities was not explored. Therefore, it was recommended that further studies should be conducted in order to compare the knowledge increment among students achieving highest and lowest scores.
5.1. Conclusions
Active participation of the students plays a significant role in gaining knowledge when adopting SDL. Overall, students’ performance was improved when they attended a short lecture about the topic before the implementation of SDL. Students perceived the activity as a valuable learning experience and appreciated the benefits of active, self-directed learning. Therefore, it was highly recommended that a sensible combination of lectures and SDL, rather than the implementation of SDL alone, should be used for teaching first-year MBBS students.