1. Background
Pathology is one of the fundamental sciences in medical curriculum. In most institutions, pathology teaching is mostly lecture-based, with practical and tutorials as interactive sessions. Due to this system of lecture taking, there is less active participation by the students, which leads to a passive acquisition of knowledge. Moreover, pathology is taught as an individual subject without any interdisciplinary interaction. Thus, there is a failure to associate and correlate the pathophysiology of the disease with the clinical presentation and diagnosis of the disease and apply this theoretical knowledge to clinical practice (1). It is now realized that there has to be a mix of basic and clinical sciences as an integrated curriculum. For this, clinical work has to be included early in the medical course. There is also an immense need to create an environment of active learning where students are involved, which may help in teaching critical thinking and problem-solving skills.
With the introduction of competency-based medical education (CBME) for medical graduates as per the graduate medical education regulations (GMER), the educational scenario in India has undergone a paradigm shift. The main objective of the new CBME pattern is application of the knowledge and not only gaining knowledge (2). This new curriculum aims to deemphasize the compartmentalization of traditional medical disciplines through integration methods. Several innovative methods have been developed over the years to achieve this. One of them is case-based learning (CBL), where clinical cases are used to assist in teaching the concepts. It is an effective teaching method as it links learning across multiple disciplines and allows for clinical integration (3).
CBL focuses on exploring real-life situations using an interactive student-centered approach. In this method, the case serves as a trigger to initiate the process of learning. Usually, clinical cases are given as problems to the students with detailed patient history and clinical situations. Additional information such as relevant physical examination, and radiological or laboratory investigations are given to support the clinical decision-making (4). It helps the medical students integrate the clinical history of patients with their laboratory investigations and use it for the diagnosis and further management of the patient. This enables the medical graduates to correlate their knowledge of pathology with the clinical case and diagnosis of disease (5). Hence, this is a learner-centered method that involves maximum interaction among participants. CBL emphasizes teamwork and a multidisciplinary approach in evaluating a clinical case with the help of existing knowledge. The instructor plays the role of a facilitator only, with students being the principal analyzers of the given case (6). A systematic review concluded that both teachers, as well as students, enjoy the process of CBL (7). A recently published study by Sangam et al. evaluated the efficacy of CBL as compared to traditional lectures in anatomy. They concluded that CBL was more effective in retention of knowledge by the students (8).
With the above knowledge, the literature was reviewed to find original research in the area of implementation of CBL in pathology and its effectiveness as a teaching method. Although some relevant articles were found, there was an overall dearth of recent original studies, especially in pathology subject in second medicine and bachelor of surgery (MBBS) students. Also, there were no such studies previously performed in our institute in pathology.
2. Objectives
Thus, this study aimed to evaluate the effectiveness of implementation of CBL in the medical students in the Pathology Department. Furthermore, the perceptions of students and faculties regarding the CBL as a teaching method were also appraised.
3. Methods
This was a pre-post interventional study carried out at Government Medical College affiliated with a civil hospital in the second year MBBS students coming to the Department of Pathology. After taking permission from Institutional Ethics Committee, faculties and students were oriented regarding the process of CBL and the role of faculties as facilitators. For the study, two CBL exercises with their learning objectives were prepared on anemia and jaundice in consultation with a physician. The cases used for CBL were developed by pathology faculties and were approved by subject experts in alignment with educational goals. A pre- and post CBL subject-based assessment sheet as well as a post-CBL questionnaire to record the perceptions of students and faculties were prepared and pre-validated and were also pre-approved by the Ethics Committee.
The students of the second-year MBBS were divided into two groups based on their roll numbers. Group A (n = 75) received anemia cases and group B (n = 75) received jaundice cases. After the theory lectures and practical classes on anemia and jaundice had been covered, both groups were given pre-test, which included clinical scenario-based multiple-choice questions (MCQs). This was done before applying CBL approach to record the knowledge of students after regular teaching. The same MCQs were again given to the students after the CBL session to record the results after CBL sessions. After this, the groups were divided into five subgroups, and one CBL exercise, along with learning objectives, was given to each group, group A was given anemia, and group B was given jaundice for discussion and implementation of theoretical knowledge. Each group was assigned a facilitator.
Three sessions on one CBL exercise were conducted. The case was disclosed to the students one page at a time, with learning objectives of the case. Students worked collaboratively to analyze the case, considering what they already knew and applying their knowledge to the case. They also developed learning goals and study questions for each session of the case. The facilitators had the cases with certain highlighted trigger words (that stimulate questions and learning) to guide the flow of discussion toward learning objectives. They also had a list of resources, so that structure and direction could be provided to the students. At the end of each session, learning goals were told to the students. They would need to work before the next CBL session, and facilitator provided them with resources for studying. Similarly, all further sessions were conducted. In the last session, students reviewed the whole case, and students from each group also presented a seminar on varying aspects of the topic. Ten days after the last session, post-test was taken.
Evaluation of the effectiveness of CBL was done by improvement in performances of students by pre and post-test analysis. Perceptions of students regarding usefulness of CBL were recorded by a 5-point Likert scale questionnaire containing 18 questions followed by a focused group discussion. Similarly, perceptions of faculty staff were recorded by a 5-point Likert scale questionnaire containing 16 questions followed by an in-depth interview.
3.1. Data Analysis
All data were entered into Microsoft Excel 2016. The data were represented using means and percentages. Compilation and statistical analysis were done using SPSS software version 16. The paired sample t-test was used to analyze the in-group data obtained before and after applying CBL to both groups separately. P < 0.05 was considered statistically significant.
4. Results
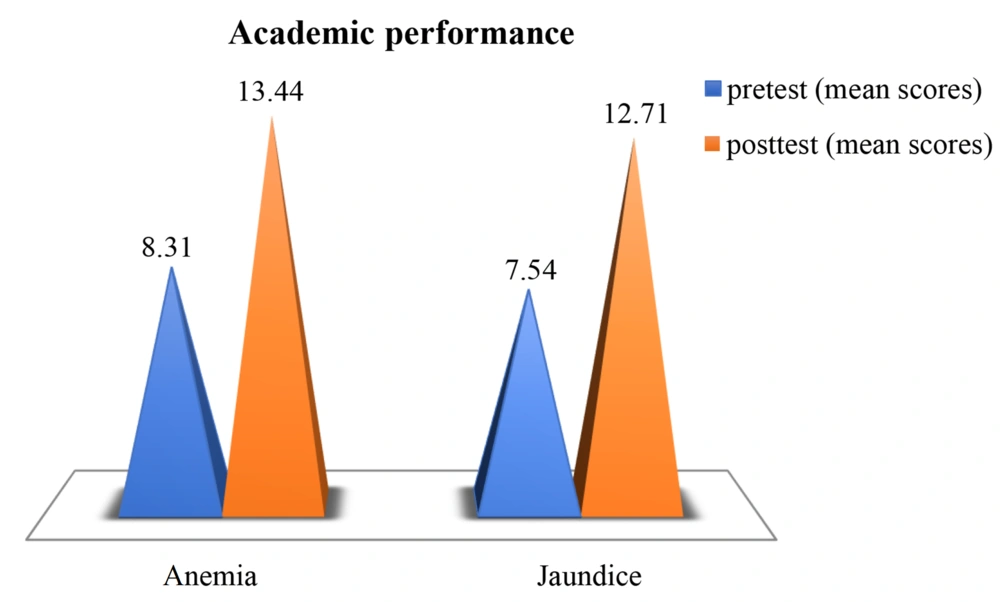
A total of 150 students of the second-year MBBS were exposed to this new teaching intervention in the form of case-based learning. Of these, 110 students gave pre- and post-CBL tests and also completed the feedback analysis. As evident in Figure 1, there was a significant improvement in learning of the students with CBL as compared to the didactic lectures (P < 0.001). This is based on their mean scores on the pre-and post-test MCQs. Mean score before implementing the CBL in group A with anemia cases was 8.31 and after the CBL in group B with jaundice cases was 13.44 (P = 0.001) and 7.54 and 12.71 (P = 0.001).
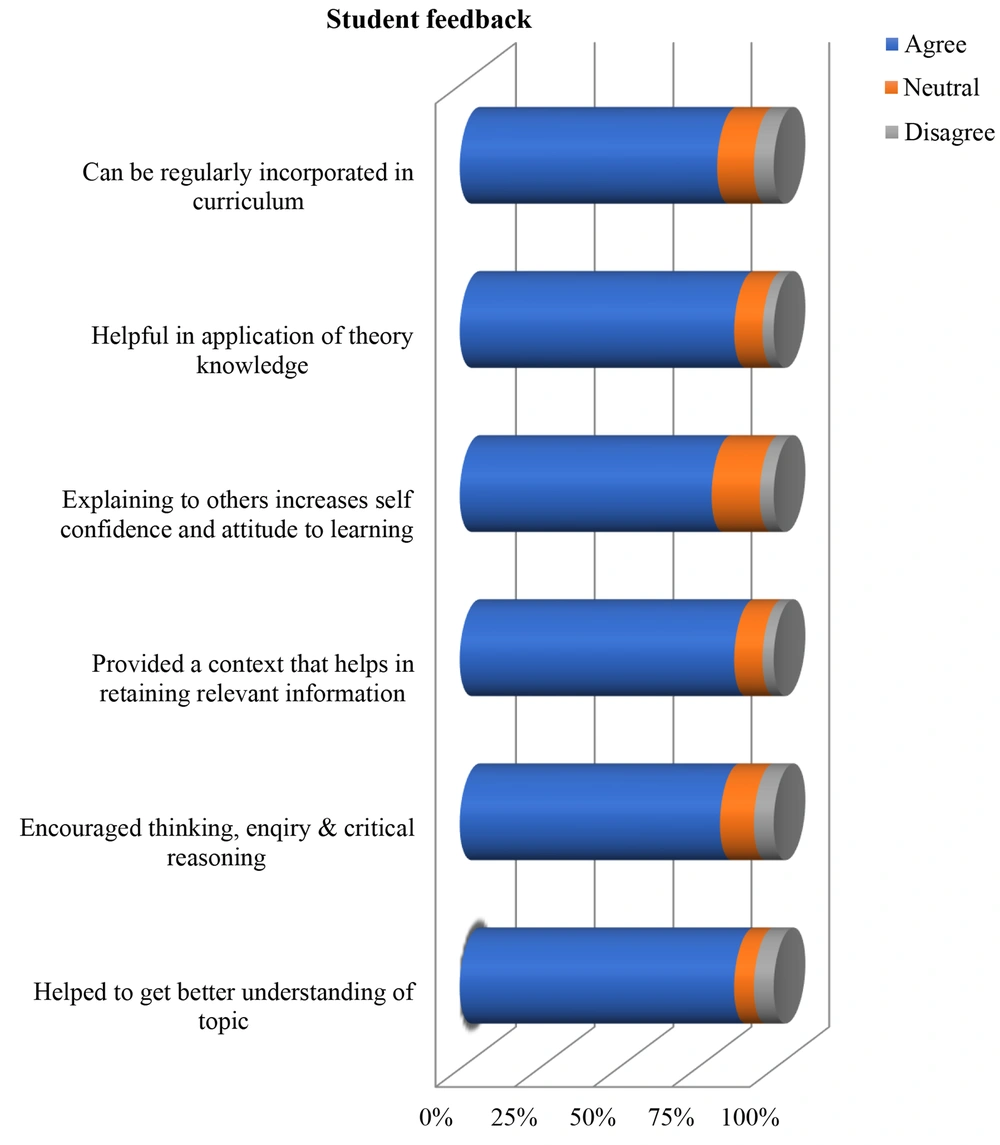
Feedback analysis from the students, as shown in Figure 2, revealed that 87% of the students agreed that CBL helped in application of theoretical knowledge and was useful in understanding the topic. Moreover, 87% of the students experienced longer retention of the topic as the CBL provided a context to the learning. In addition, 82% acclaimed that it encouraged their thinking and inquiry. Also, 86% of the students believed that small group discussion helped valuable exchange of ideas, and 82% of the students found their communication and interpersonal skills improved after the CBL session. They also agreed that this exercise should be regularly incorporated into the curriculum. Focus Group discussion revealed that they found small group teaching more interactive, useful, and enjoyable in contrast to traditional teaching, which was monotonous. They could retain the topic due to discussion and interaction among them. They suggested didactic lectures should be followed by related CBL.
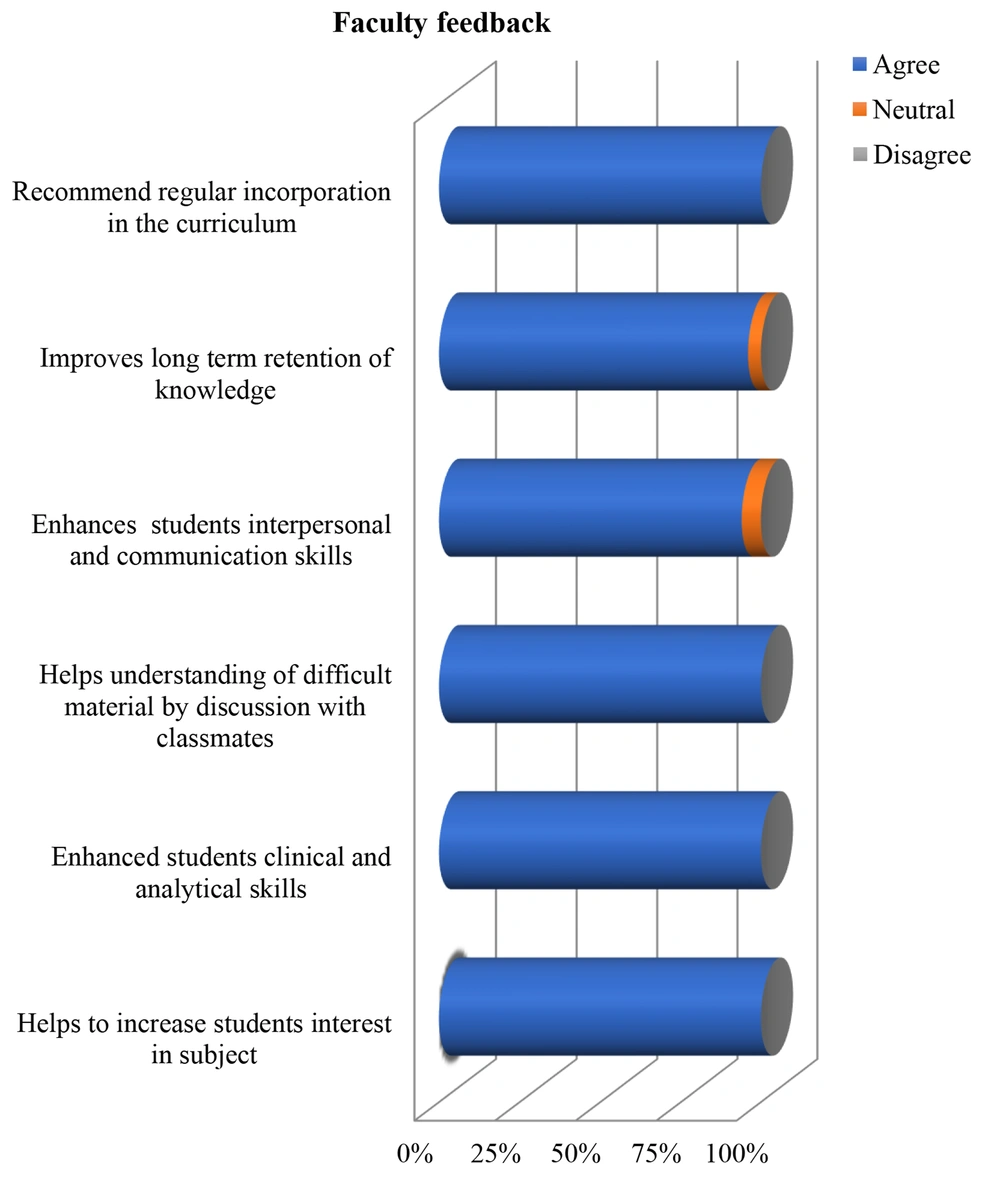
Six faculty members were involved as facilitators in the CBL session, and their feedback was taken. Five of them were third-year residents, and one was an assistant professor in the Pathology Department. Feedback from faculty, as shown in Figure 3, revealed that all of them agreed that CBL increased the interest of students in learning and it should be promoted, as discussion and interaction with friends helped to learn and also increased recall capacity. In the words of assistant professor “with CBL, interaction increased and confidence of the students built up. Shy students also participated. Thinking process activated.” It helped increase the interest in a subject itself. Small group promotes participation and interaction of students. Faculty also perceived that it also improved self-directed learning ability among students. As mentioned by one of the 3rd year residents during the interview, “few of the students are sincere, so they read and learn and few of the students are not sincere, if they are facilitated, then it becomes easy for them to learn.” Interview revealed that faculty believed that CBL increased communication skills of students. They thought that it was difficult to apply it to the whole subject because of the limitations of manpower, infrastructure and time, so it must be applied to vital and must-know topics in each system. Integrated CBL can be done with involvement of other departments because the same topic is taught in multiple departments. So we can use resources in a good way with the integration.
5. Discussion
It has been understood that education needs to be an active productive mental activity. To make someone comprehend a certain area of knowledge, it is best to involve them in the learning process (9). Many modalities can be used to implement this acquisition of knowledge. They range from traditional didactic methods, integrated learning models and also some modern methods like problem-based learning and CBL. Our institute has always put its faith in the time-tested traditional didactic method of learning. Changing times, new evidence-based research, and improved understanding of memory retention and reproduction have revealed the shortcomings of such traditional methods. Considering these aspects, implementation of case-based learning was attempted for the first time in our institute. The purpose of this study was to compare the effectiveness of CBL compared to traditional didactic method among MBBS students in the subject of pathology.
With the introduction of CBL, faculties and students were sensitized to this active-interactive small group teaching method. We reported statistically significant improvement in retention of study material. Students also reported a better understanding of the topic and were eager to adopt these learning methods. It encouraged self-learning and collaborative learning. The majority of the students and faculties embraced and enjoyed the CBL exercises. According to the student perception results, it was observed that CBL also improved logical thinking, clinical decision-making, and diagnostic interpretations among them.
Previous studies by different researchers in different geographical locations and studying different subjects corroborated our findings. A study by Ciraj et al. found that including the CBL in routine teaching as a learning strategy was superior to teaching without any CBL sessions in the curriculum (10). Surapaneni evaluated CBL as a part of integrated learning and observed that the majority of students reported a better understanding of the topic with CBL, and it also helped them exchange ideas and knowledge application in the future (11). Two recent studies conducted on the pharmacology subject also concluded that CBL was an effective tool in teaching the subject to a large group of students (12, 13). CBL provided better motivation and satisfaction to the students. It also improved students’ attendance in class (13). Hasamnis et al. also concluded that CBL helped in amalgamating theoretical knowledge into clinical pharmacology practices (12).
The main question is that although CBL is beneficial for the students, does it warrant the replacement of current teaching methods with CBL? Garvey et al. studied PBL vs. CBL. They noticed that even though the goals of PBL and CBL were common, each teaching method had unique characteristics (14) in PBL, the learning was driven by the problem. Whereas, for the case-based approach, some previous knowledge about the topic is required to solve the clinical case. While comparing CBL with traditional methods, Garvey et al. and Engel and Hendricson, using a combination of questionnaires and Likert scales, observed that the majority of the students enjoyed CBL, and it improved students’ confidence (14, 15). The same findings were reported by Setia et al. while comparing CBL vs. PBL. The researchers found that the majority of the students felt motivated to work more on the subject and also agreed that CBL improved their problem-solving skills and facilitated interaction between students and faculties (16). This was inconsistent with the findings of a previous study conducted by Kassebaum et al., who concluded that students preferred lectures to be better than CBL approach as it helped them prepare better and score more in the written exams (17).
This study had some limitations. CBL, owing to its interactive teaching method, needs more resources and is time-consuming. It requires more staff. All topics cannot be taught by this method. The faculty suggested the use of this method only for must-know topics, ideally one from each system. The students felt that some prior knowledge of the topics was essential to reap the benefit of this system. They suggested that first few sessions should be theoretical to know the background/concept, and it should be followed by related CBL. Also, simultaneous teaching of the same topic in different subjects would be more rewarding as it would integrate various aspects of the same topic. Thus, CBL is not a perfect model and is not capable of replacing other methods of teaching. Also, the study did not compare the effect of CBL vs. didactic lectures on the results of written subject exams.
5.1. Conclusions
It can be concluded that case-based learning stimulates student-centered exploration of cases which promotes their logical, analytical, clinical skills, and collaborative skills. It promotes active learner-centered learning. It may serve as an effective tool in bridging the gap between preclinical and clinical subjects and various disciplines. Though it is a good educational method, it cannot replace didactic lectures. Thus, it may become an effective supplement to the traditional lecture methods. If used strategically, CBL may prove to be an effective tool in bridging the gap between theory and practice, and so relevant topics should be taught by CBL. Further studies conducted in various subjects with a large group of students will help provide a more student-focused approach to the medical education curriculum. Also, studies comparing the effect of CBL + didactic lectures vs. only regular lectures on students’ exam performances can also be conducted to evaluate the effectiveness of CBL better.